Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.2 Lima abr./jun. 2021
http://dx.doi.org/10.31403/rpgo.v67i2321
Case Report
Diagnosis and treatment of Herlyn-WernerWünderlich syndrome: Report of two cases
1Departamento de Especialidades Quirúrgicas, Instituto Nacional de Salud del Niño San Borja, Lima, Perú
Müllerian malformations are congenital anomalies that usually manifest after menarche. Among them, Herlyn-Werner-Wünderlich syndrome (SHWW) is characterized by didelphic uterus, obstructed hemivagina and ipsilateral renal agenesis. The clinical presentation of SHWW is usually asymptomatic until menarche; most are diagnosed 2 months to 1 year after first menstruation. Presenting symptoms are dysmenorrhea, recurrent cyclic abdominal pain, irregular menses, and sometimes palpable pelvic mass. Occasionally, hematocolpos or hematometra may develop pyocolpos, pyosalpinx and pelviperitonitis, and some patients manifest only infertility or recurrent pregnancy loss. We report the cases of two patients aged 11 and 13 years who presented with cyclic abdominal pain and describe the clinical history, imaging and specific treatment performed in each patient.
Key words: Herlyn-Werner-Wünderlich syndrome; Uterus; Müllerian ducts; Hematocolpos; Hematometra
Introduction
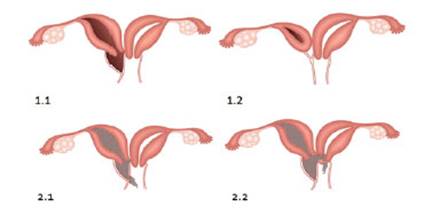
Herlyn-Werner-Wünderlich syndrome (SHWW) is a rare anomaly of the Müllerian ducts, characterized by uterine duplication with obstructed hemivagina and ipsilateral renal agenesis1,2. Congenital malformations of the Müllerian ducts have a prevalence of 2% to 3% in women, with a prevalence of 1/200 to 1/600 in fertile women. Didelphic uterus accounts for 11% of Müllerian duct anomalies and 30% of them are associated with renal tract anomalies3. SHWW is associated with mesonephric duct anomalies, with an incidence of approximately 1/2 000 to 1/28 000. The syndrome is recently known by the acronym OHVIRA (obstructed hemivagina and ipsilateral renal anomaly syndrome)4). A new classification of the syndrome is proposed due to the clinical characteristics which, according to Lan Zhu (see Figure 1), differ according to the level of complete and incomplete obstruction of the vaginal septum, allowing a timely diagnosis and effective treatment5,6.
Lack of development or fusion of the distal segments of the Müllerian ducts causes this anomaly and its etiology is unknown. The incidence is variable. It usually presents after menarche with a diverse clinical picture, cyclic pelvic pain, dysmenorrhea, palpable mass due to hematometra or hematocolpos and sometimes pyocolpos or pelviperitonitis. Diagnosis should be made early to avoid complications such as endometriosis, pelvic adhesions or other pelvic complications.
A careful pelvic examination is necessary to identify the cervix and vagina4-6. Ultrasonography is the first method to evaluate the gynecologic abnormality. However, magnetic resonance imaging (MRI) provides certainty of the findings, allowing timely and correct treatment. Prior to surgical intervention, it is recommended to classify SHWW according to Lan Zhu. Surgical treatment consists of drainage and resection of the vaginal septum1,2,4. In this article we present two cases of Herlyn-Werner-Wünderlich syndrome. The clinical history, the results of imaging tests and the treatment performed are described.
Clinical Case 1
A thirteen-year-old patient was attended at the Instituto Nacional de Salud del Niño de San Borja in 2017 due to cyclic abdominal pain and fever of 7 hours of evolution. She did not have a significant history, menarche was at age 11, with catamenial regimen of 4/30 and tolerable dysmenorrhea. Physical examination revealed weight 42 kg, breasts Tanner stage 4, painful abdomen on palpation in the left iliac fossa, with the presence of a slightly movable 6 cm mass. The vulva showed Tanner stage 4 and vaginometry of 3 cm from the hymenal border. Abdominal ultrasound showed two endometrial cavities and two cervices, compatible with a didelphic uterus. The left cervix had continuity with heterogeneous cystic formation without Doppler flow, suggesting hematocolpos with hematic content of approximately 154 mL and measured 6.9 x 5.5 x 7.4 cm. Both ovaries were observed and no free fluid was found in the cul-de-sac. The left kidney was not visualized. Magnetic resonance imaging revealed a right didelphic uterus with preserved myometrium, endometrium and vagina. The left uterus showed elongated morphology with no contents inside. There was a vaginal distension of 78 x 37 x 62 mm that displaced the bladder and showed restriction in the diffusion technique, in relation to purulent content (Figure 2). The diagnosis was didelphic uterus with hematocolpos of the left hemivagina, ipsilateral hematometra and left renal agenesis, compatible with Herlyn Werner Wünderlich syndrome.
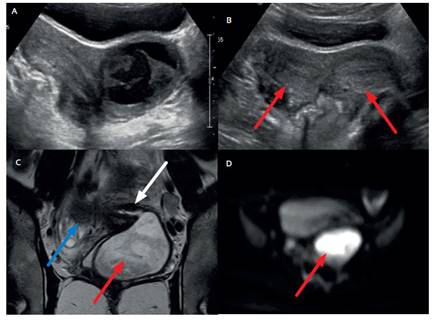
Figure 2 (a) ultrasound shows both hemiuteri, with distension of the left hemivagina. (b) one month after surgery, ultrasound control displays both hemiuteri (red arrows). (c) t2 coronal magnetic resonance image shows continuity between the left hemiuterus (small white arrow) and the left hemivagina (small red arrow), which is distended. the blue arrow shows the right hemiuterus. (d) diffusion technique suggested restriction compatible with abscess, which was later confirmed during surgery.
The patient underwent physical examination prior to anesthesia and posterior recession of the septum of the hemivagina; 150 mL of pyocolpos were drained. According to Lan Zhu's classification, she would correspond to type 2.1: didelphic uterus with partial resorption of the vaginal septum. Vaginoscopy was performed to identify and observe the permeable right and left cervix. Culture of the pyocolpos discharge isolated Streptococcus alpha hemolyticus. The patient was discharged the day of surgery and was clinically free of symptoms.
Clinical Case 2
The 11-year-old patient attended the Instituto Nacional de Salud del Niño de San Borja in 2018, with a history of left renal agenesis. During the previous 3 years she had consulted for abdominal pain that intensified with menstruation, of 4 months of evolution, which improved with analgesics. Menarche was at the age of 10 years 8 months, with catamenial regimen 4/30. Physical examination showed Tanner stage 3 breasts, painful abdomen on palpation, normal Tanner stage 2 external genitalia, scant vaginal bleeding and rectum occupied by collection. Ultrasound study showed hematocolpos and didelphic uterus. Magnetic resonance imaging revealed two uterine horns with severe dilatation of the left uterine cavity, communicating with the left hemivagina dilated by blood content of 13 x 8 x 5.4 cm. The left uterine tube appeared dilated; 10 mm thick (hematosalpinx). The findings were compatible with a didelphic uterus with closed left hematometra and left hematocolpos (Figure 3), as well as left renal agenesis, consistent with Herlyn-Werner-Wünderlich syndrome.

Figure 3 magnetic resonance of the pelvis. in the axial (a) and coronal t2 wi (b) sections, part of the left hemiuterus (white arrow) and left hemivagina (red arrow) are distended, with hypointense fluid representing blood products. c. pelvic ultrasound after surgery shows the right and left hemiuterus, with no evidence of significant distention of the vagina.
Physical examination was performed under anesthesia, with drainage of the hematometra and hematocolpos, as well as vaginoplasty and resection of the septum, finding 600 mL of retained menstrual blood and a 3 cm transverse septum. According to Lan Zhu's classification, it would correspond to type 1.1: Didelphic uterus with completely obstructed hemivagina. The patient had a favorable evolution and was discharged the day after surgery, clinically stable and asymptomatic.
Discussion
The etiopathogenesis of Herlyn-Werner-Wünderlich syndrome is unknown1,2,4. This anomaly may result from lack of fusion of the Mullerian ducts in the midline to connect with the urogenital sinus, or from the creation of an adequate lumen at the top of the vagina and uterus by resorption of the central vaginal cells and the septum between the fused Mullerian ducts, resulting in duplication of the body and cervix4.
The clinical presentation of Herlyn-Werner-Wünderlich syndrome is usually asymptomatic until menarche; most are diagnosed 2 months to 1 year after the first menstrual period. Presenting symptoms are dysmenorrhea, recurrent cyclic abdominal pain, irregular menses, and sometimes a palpable pelvic mass. Occasionally, hematocolpos or hematometra may develop pyocolpos, pyosalpinx and pelvic peritonitis, and some patients manifest only infertility or recurrent pregnancy loss4,7. In the two cases presented, patients reported abdominal pain that increased with menstruation, as well as symptoms described in similar cases5,8. The age of presentation was also similar to other reports, starting menstruation starting between 11 and 13 years of age8. One case has been described in an adult female(9) whose initial diagnosis was an ovarian-related pathology due to abdominal pain. Ultrasound and MRI were requested for further evaluation and the results were compatible with Herlyn-Werner-Wünderlich syndrome.
Lan Zhu's classification allows to identify the type of obstruction, and provide better management. The surgical treatment of choice is wide resection of the septum. When the obstructed hemivagina is bulging, management is easier (Zhu classification 1.1), as in case number 2, in which 600 mL of retained blood was drained. When the hemivagina is not bulging or is partially bulging due to a communication, the management is extensive resection of the septum, as in the first published case, in which purulent material was drained (Zhu classification 2.1). In both cases, the vaginal septum was resected and the hematocolpos or pyocolpos was drained, with satisfactory results.
Our report is relevant, because pyocolpos in Herlyn-Werner-Wünderlich syndrome is extremely rare5,10. It is important to consider this type of presentation in febrile patients with acute abdominal pain. Ultrasound allows detection of the syndrome and is inexpensive. However, MRI is recommended for better resolution and anatomical definition.
Although Herlyn-Werner-Wünderlich syndrome is a very rare presentation, it is believed that these cases may be relatively frequent in our country, so it should be suspected in adolescents with abdominal pain and dysmenorrhea, for correct diagnosis and management and to avoid complications such as chronic pelvic pain, endometriosis and infertility.
REFERENCES
1. Sosa-Tejada R, Hernández-Díaz EM, López-Ruano A, Bolaños-Bendfeldt, J, González-Arrechea, F, Alvizures-Borrayo F, et al. Síndrome de Herlyn-Werner Wunderlich o Síndrome OHVIRA. Reporte de Caso. Rev Guatem Cir. 2016;22. [ Links ]
2. Wu T-H, Wu T-T, Ng Y-Y, Ng S-C, Su P-H, Chen J-Y, et al. Herlyn-Werner-Wunderlich syndrome consisting of uterine didelphys, obstructed hemivagina and ipsilateral renal agenesis in a newborn. Pediatr Neonatol. 2012 Feb;53(1):68-71. DOI: 10.1016/j.pedneo.2011.11.014 [ Links ]
3. Del Vescovo R, Battisti S, Di Paola V, Piccolo CL, Cazzato RL, Sansoni I, et al. Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging. 2012 Mar;12:4. [ Links ]
4. Afrashtehfa CDM, Piña-García A, Afrashtehfar K. Malformaciones müllerianas. Síndrome de hemivagina obstruida y anomalía renal ipsilateral (OHVIRA). Cir Cir. 2014;82:460-71. [ Links ]
5. Jung EJ, Cho MH, Kim DH, Byun JM, Kim YN, Jeong DH, et al. Herlyn-Werner-Wunderlich syndrome: An unusual presentation with pyocolpos. Obstet Gynecol Sci. 2017 Jul;60(4):3747. DOI: 10.5468/ogs.2017.60.4.374 [ Links ]
6. Zhu L, Chen N, Tong J-L, Wang W, Zhang L, Lang J-H. New classification of Herlyn-Werner-Wunderlich syndrome. Chin Med J (Engl). 2015 Ene;128(2):222-5. DOI: 10.4103/03666999.149208 [ Links ]
7. Moshiri M, Seyal AR, Cruite I, Bhargava P. Herlyn-Werner-Wunderlich syndrome with a partially obstructed hemivagina. Radiol Case Rep. 2015 Dic;7(4). DOI: 10.2484/ rcr.v7i4.800 [ Links ]
8. Kapczuk K, Friebe Z, Iwaniec K, Kedzia W. Obstructive müllerian anomalies in menstruating adolescent girls: A report of 22 cases. J Pediatr Adolesc Gynecol. 2017 Oct. DOI: 10.1016/j.jpag.2017.09.013 [ Links ]
9. Boria Alegre F, Lucas Ramos J, Álvarez-López C, Poza Cordón J. Síndrome de Herlyn-Werner-Wünderlich y diagnóstico tardío: a propósito de un caso. Rev Peru Ginecol Obstet. 2019;65(3):337-40. DOI: 10.31403/rpgo.v66i2191 [ Links ]
10. Meneses AD, Filho WMNE, Raulino DMR, Martins EBL, Vieira SC. Herlyn-Werner-Wunderlich Syndrome with ureteric remnant abscess managed laparoscopically: A case report. Oman Med J. 2017 Mar ;32(2):157-60. DOI: 10.5001/omj.2017.28 [ Links ]
Received: January 27, 2021; Accepted: February 22, 2021











 texto en
texto en