Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.2 Lima abr./jun. 2021
http://dx.doi.org/10.31403/rpgo.v67i2322
Case report
Buschke-Löwenstein tumor in a girl. A case report
1. National Institute of Child Health, Lima, Peru
Buschke-Löwenstein tumor is a benign giant condyloma acuminatum, whose clinical lesions are larger than 10 cm, so the treatment of choice should always be surgical. We present the case of a one-year-old girl with giant condyloma of the vulva, a rapidly evolving Buschke-Löwenstein tumor, who underwent successful surgical resection. The literature was reviewed regarding its diagnosis and treatment.
Key words: Vulvar neoplasms; Buschke-Löwenstein tumor
Introduction
Giant condyloma or Buschke-Lowenstein tumor is a benign epithelial tumor of viral origin that is sexually transmitted and can rarely become malignant. Giant condylomas in children have been little studied. Rapidly evolving, it consists of an exo- and endophytic hyperpapillomatosis of viral origin (human papillomavirus (HPV) types 6 and 11)1,2, which is located in the perineoano-rectal region, but also on the oral mucosa and the penis.
In 1986, Abraham Buschke described condyloma acuminatum in Neisser's Stereoskopischer Atlas1,2. It is more frequent in men than in women, with a 3:1 ratio, and there are few publications in women, with a higher incidence during pregnancy, in smokers and if they have had previous cervical lesions or genital warts3,4.
Histologically, the lesion shows proliferative masses and cavities, as well as papillomatosis, acanthosis, hyperkeratosis, variable cellular paraker atosis and infiltration of inflammatory cells of the underlying tissues5,6.
There are different treatments for the tumor, the most effective being radical surgical resection to avoid recurrence, malignancy and mortality3,5. Mortality is estimated at 20%.
Case report
A girl, 1 year and 8 months old, from Chiclayo, started the disease one month before the first consultation, with warty lesions on labia minora, labia majora and inguinal region, which progressively evolved in number and extension in the vulvar and perineal regions. She went to a local health center where she was evaluated and the lesion was biopsied and the patient referred to the Instituto Nacional de Salud del Niño, in Lima, Peru.
As personal history, she was born vaginally at 32 weeks of gestation, the product of a twin pregnancy. The birth weight was 3 000 g, with Apgar 9-9, spontaneous crying, and she suffered from diaper rash. The mother presented genital wart before gestation, without specifying the location; no gynecological examination was performed at the time of consultation with the daughter.
Physical examination showed regular general condition, nutrition and hydration, with mammary and vulvar Tanner I development. There was evidence of increased volume and vegetative, non-infiltrating, arborizing lesions extending from the perianal region to the vulvar region and both inguinal regions, involving the labia minora and labia majora in all their extension (Figure 1). No signs of sexual abuse were found on examination.
Tests for HIV, hepatitis B and C and RPR were negative. Vulvar biopsy showed findings consistent with condylomatosis and detection and differentiation of 28 genotypes of human papillomavirus was performed. Genotype 6 was found by polymerase chain reaction.
The result of CD3 T lymphocytes by flow cytometry was 61 %, CD3+ CD4+ T lymphocytes 27.9 %, CD3+CD8+ T lymphocytes 29.1 %, CD19+ B lymphocytes 1,395 and CD56/16 NK lymphocytes 569, all with values within normality.
The surgical interventionunder general anesthesia consisted in removing the hyperpigmented, warty, exophytic condylomatous lesions occupying the vulvar and perineal area in an extension of 12 x 12 cm. The resection was total, using a monopolar electroscalpel in cutting and coagulation mode. The patient tolerated the surgical procedure satisfactorily and had a favorable evolution, remaining hospitalized for 24 hours.
The pathology results confirmed the diagnosis of condyloma acuminatum due to human papillomavirus. Macroscopically, multiple irregular fragments of tissue measuring 7 x 6 x 1.3 cm, surface with exophytic lesions of warty appearance, brownish color and fibroelastic consistency were observed (Figure 1).
Microscopically, the epidermis showed acanthosis, papillomatosis, hyperkeratosis and sparse parakeratosis, presence of cells with nuclei with discrete hyperchromasia and clear perinuclear halo corresponding to koilocytes. In the dermis, lymphoplasmacytic infiltrate, neovascularization and vascular congestion were observed (Figure 2).
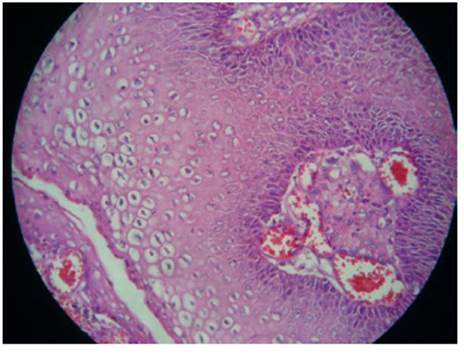
Figure 2 Squamous epithelium; in the intermediate and superficial layer there are ovoid or round cells with clear perinuclear halo, pyknotic or retracted nuclei (koilocytes). On the surface, parakeratotic cells.
A control was performed one month and two months after surgery, observing adequate evolution and wound closure, with absence of bleeding and infection. Vaccination against human papillomavirus (HPV) was indicated. During the control showed adequate consolidation of the scar, without tumor recurrence and with good esthetic result (Figures 3 and 4).
Discussion
Buschke-Löwenstein tumor is a rare entity, with an incidence of 0.1% in the general population. It predominantly affects men, with few reports in women, being more frequent during pregnancy and with few publications of cases in girls or adolescents. It presents rates of up to 56% of evolution to squamous carcinoma, 66% of recurrence and 20% of mortality2,3,6. In the present case no malignant behavior was found.
It has been established that transmission is sexual, more frequent in males (3:1 ratio), between the fifth and sixth decade of life, associated with infection by HPV types 6 and 11, highly contagious1-5. Valdés reported the case of a 10-yearold girl with no history to explain transmission7. Ambriz et al. indicate that, in the pediatric age group, possible transmission through sexual abuse should be considered8. And Aydogdu reports that it is estimated that 50% of cases in children are due to abuse; however, he publishes 3 pediatric cases without evidence of abuse8.
In the case presented there was no evidence of sexual abuse and it is presumed that the infection was acquired during vaginal delivery, unlike the second twin who was born by cesarean section and did not present the disease. In girls, vertical transmission of HPV occurs in about 20% of cases, including peripartum transmission, and there is no relationship with age. This is shown in the case of Perez-Elizondo et al, who report a 3-year-old girl with a history of repeated sexual abuse6-9.
Buschke-Löwenstein tumor has poorly understood clinical and imaging characteristics and its management is not agreed upon3,4. Risk factors include being a carrier of immunosuppression (HIV infection, use of corticosteroids, immunomodulators, diabetes mellitus), sexual promiscuity and having smaller condylomas. The most frequent locations in women are the vulva (90%) and the perineum, as in the present case. The associated adenopathies are rather reactive to the lesion or due to superinfection; very rarely they correspond to metastases. The age range of the patients is between 19 and 53 years, with no clear age preference in other studies3. In the present case, the patient was a one-year-old girl.
Regarding the imaging study, its role is to determine the extent of the lesion and the involvement of neighboring structures, in order to establish the possibility of surgical resection. Immunological studies showed that innate immunity was normal, cellular response was not compromised, with a decrease in CD4 and CD8 lymphocytes5. In cases of perianal condylomas, the involvement of the anal sphincter must be established in order to determine a local resection or low abdomino-perineal resection (Miles operation)3.
Treatment is eminently surgical, with no established guidelines. Although local treatments with podophyllin, cryotherapy, electrocoagulation, fluorouracil, CO2 laser and even radiotherapy have been described, its usual management is resection of the lesion with wide margins or more invasive procedures, depending on the degree of local invasion of the tumor. The adjuvant use of chemotherapy (bleomycin, methotrexate) has been described. None of these approaches has achieved a lower recurrence of the lesion. Our patient was managed with surgical excision, with no recurrence to date2,7,9-11.
Among the limitations in the presentation of the present case, papillomavirus screening was not performed in the mother and it has not been possible to document an updated photograph of the case, due to access limitations, since the patient comes from the interior of the country.
In our patient, clinical controls were planned every three months for one year, then every six months for one year and finally annually. However, the patient did not attend her check-ups as frequently as suggested, due to geographical distance limitations.
It is concluded that giant condyloma (Buschke-Löwenstein tumor) is a voluminous lesion with a cauliflower-like appearance, infrequent in girls and adolescents9, which is associated with compromised immune system. The treatment of choice should always be surgical, taking into account the need for follow-up and verifying the possibility of sexual abuse12,13.
REFERENCES
1. Steffen C. The men behind the eponym--Abraham Buschke and Ludwig Löwenstein: giant condyloma (Buschke-Loewenstein). Am J Dermatopathol. 2006 Dec;28(6):526-36. doi: 10.1097/01.dad.0000211528.87928.a8 [ Links ]
2. Qarro A, Ait Ali A, Choho A, Alkandry S, Borki K. Tumeur de Buschke- Löwenstein à localisation anorectale. (A propos de trois cas). Ann Chir. 2005 Feb;130(2):96-100. French. doi: 10.1016/j.anchir.2004.06.005 [ Links ]
3. Montaña N, Labra A, Schiappacasse G. Condiloma acuminado gigante (Tumor de Buschke Löwenstein). Serie de 7 casos clínicos y revisión de la literatura. Rev Chilena Radiol. 2014;20(2);57-63. http://dx.doi.org/10.4067/S0717-93082014000200005 [ Links ]
4. Moukit M, Saghir S, Ait Bouhou R, Kouach J, Moussaoui Rahali D, Dehayni M. Buschke-Löwenstein tumors in a 12-yearold girl. Sex Transm Dis. 2018 Mar;45(3):e12. doi: 10.1097/OLQ.0000000000000749. PMID: 29420453 [ Links ]
5. Ríos M, Hernández M, Aguilar F, Aguilar K, Amigó M, Silveira M y col. Condiloma gigante (tumor de Buschke-Löwenstein) de la vulva. Rev Cubana Obstet Ginecol [Internet]. 2014 Jun;40(2):258-64. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0138-600X2014000200012&lng= es [ Links ]
6. Santa María C, Castillo C. Tumor de Buschke Löwenstein en adolescente embarazada de término. Rev Cient Cienc Med [Internet]. 2019;22(1):75-6. http://www.scielo.org.bo/scielo.php?script=sci_arttext&pid=S1817-74332019000100014&lng=es [ Links ]
7. Pe´rez-Elizondo A, Cha´vez-Enri´quez P. Tumor de Buschke- Lo¨wenstein: a propo´sito de un caso infantil, Arch Investig Materno Infantil. Mayo-agosto 2019;10(2):74-6. https://dx.doi.org/10.35366/93508 [ Links ]
8. Aydogdu I, Uzun E, Mirapoglu SL, Kilincaslan H, Yildiz P. Buschke-Löwenstein tumor: Three pediatric cases. Pediatr Int. 2016 Aug;58(8):769-72. doi: 10.1111/ped.12960 [ Links ]
9. Rivera R, Lazo LA, Ordóñez L. Buschke-Löwenstein tumor. Case report. Rev inf cient. 2018 Ago;97(4):851- 9. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1028-99332018000400851&lng=es [ Links ]
10. Valde´s J, Solis U, Valde´s E, Muñoz M. Condiloma gigante o tumor de Buschke-Lo¨wenstein Giant condyloma or Buschke- Lowenstein tumor. Rev Cubana Pediat. 2017;89(1). [ Links ]
11. Machado-Cordero I, Castillo-Oliva A, Ochoa-Ochoa C, García-Gómez R, Lamar-Morales Y. Condiloma gigante de Buschke y Löwenstein, a propósito de un caso. Dermatol Peru. 2006;16(1):74-6. http://www.dermatologiaperuana.pe/assets/uploads/revista_71Ou_a11.pdf [ Links ]
12. Ambriz-González G, Escobedo-Zavala LC, Carrillo F, Ortiz-Arriaga A, Cordero-Zamora A, Corona-Nakamura A, López M, Velázquez GA. Buschke-Lowenstein tumor in childhood: a case report. Rev Cir Ped. 2005;40:E25-E27. doi: 10.1016/j.jpedsurg.2005.05.070 [ Links ]
13. Elfatoiki FZ, Hali F, Baghad B, Marnissi F, Chiheb S. Giant perianal condyloma acuminatum in an infant without sexual abuse, Arch pediatr. 2019 Nov;26(8):473-4. doi: 10.1016/j.arcped.2019.09.003 [ Links ]
Received: September 28, 2020; Accepted: March 14, 2021











 texto en
texto en 






