Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.2 Lima abr./jun. 2021
http://dx.doi.org/10.31403/rpgo.v67i2323
Case Report
Vulvar Fournier's gangrene
1Especialista en Ginecología y Obstetricia, Servicio de Obstetricia y Ginecología, Hospital Central “Dr. Urquinaona”, Maracaibo, Estado Zulia, Venezuela.
Fournier's gangrene is a rare and potentially fatal infectious disease characterized by rapidly progressive necrotic fasciitis of the genital, perineal and/or perianal region. It affects any age and gender. Vulvar Fournier's gangrene has a low incidence in women, but a high mortality rate, due to differences in female genital anatomy. Clinical suspicion is essential for diagnosis, due to the low frequency of presentation. Treatment should be aggressive, with prompt administration of broad-spectrum antibiotics and early interdisciplinary approach by multiple medical specialties. Thus, a complete understanding of the pathophysiology of the condition is necessary to increase the patient's survival rate. A case of vulvar Fournier's gangrene is presented.
Key words: Vulvar diseases, Fournier gangrene; Fascitis, necrotizing
Introduction
Fournier's gangrene is an idiopathic necrotizing fasciitis of sudden onset involving the genital, perineal and / or perianal region, with high mortality1. It is characterized by rapid progression of soft tissue infection, caused by the synergistic action of several organisms and may spread along fascial planes, causing necrosis and subfacial destruction. The most common predisposing factors are diabetes mellitus, steroid use, chronic alcoholism and advanced age. Its characteristic clinical manifestation is the abrupt onset of edema, pain and rapid progression to gangrene2.
Fournier's gangrene is a very rare condition in women. The reported frequency is 1.6 cases / 100,000 of the male population and the ratio of male to female cases exceeds 10:13. Cases occurring in vulva are commonly underdiagnosed, which usually leads to misdiagnosis and treatment failure during the acute phase, so the high mortality rate is higher compared to that of men2. A case of vulvar Fournier gangrene is presented.
Clinical Case
A 40-year-old woman came to the emergency room with painful and extensive swelling of the right vulvar area, extending to the pubic region, with drainage of foul-smelling purulent fluid of approximately 6 days of evolution, accompanied by unquantified fever and urinary retention. She reported a history of non-insulin-dependent diabetes for 5 years, treated irregularly. She denied a history of local trauma, abdominal pain, changes in bowel habits and vaginal or rectal bleeding.
On admission, the patient presented moderate cutaneous-mucosal pallor, temperature 39.1° C, respiratory rate 24 per minute, oxygen saturation 97%, heart rate 110 beats per minute and blood pressure of 100/60 mmHg, with difficulty walking. Physical examination revealed a tumor deforming the right labium majus, approximately 10 centimeters in diameter, phlegmonous and fluctuant, extending to the pubic region (Figure 1). In addition, there were large areas of edematous perineal skin with purplish-red indurations with soft tissue necrosis of the perineum and perianal region together with purulent discharge, with intense pain and pruritus, without crepitus or hemorrhagic blisters. Rectal examination was extremely painful and revealed no alterations. Necrotic tissue and venous blood were taken for cultures.
Laboratory tests showed hemoglobin of 6.5 g / dL, white blood cell count of 21,000 cells / mL with 85% neutrophils. Serum glycemia values were within normal limits. Pelvic radiography revealed some gas bubbles in the perineal soft tissues. Abdominopelvic tomography images showed extensive inflammation, edema, and subcutaneous emphysema extending from the right genito-perineal area to the insertion of the rectus abdominis muscle at the pubic symphysis, which was compatible with a diagnosis of vulvar Fournier’s gangrene.
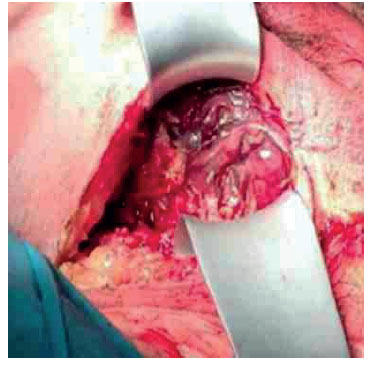
Empirical treatment with broad-spectrum antibiotics was started immediately and surgery was scheduled for surgical debridement. A long incision was made in the perineal area, draining approximately 300 mL of purulent brownish-greyish and foul-smelling fluid. A cavity was found with extensive areas of necrotic tissue at its base, partially affecting the perianal area (Figure 2). The necrotic soft tissue portions were extensively excised with subsequent irrigation and coverage with antibiotic dressings.
The anatomopathological evaluation of the samples from the surgical region was compatible with necrotizing fasciitis. The microbial culture showed polymicrobial growth of Escherichia coli, Acinetobacter and Enterococcus, while the blood culture result was negative.
After several local dressings with two new debridements and broad-spectrum antibiotic therapy, the patient evolved favorably with no evidence of fever or systemic involvement. The wound was free of infection on the fifth postoperative day and granulation tissue appeared. Complete wound closure was achieved without complications or fistula formation by partial thickness skin grafting two weeks after surgery. She was discharged 21 days after hospitalization after presenting no problems with ambulation. No wound healing problems were observed during the 3-month follow-up period.
Discussion
Fournier's gangrene is a well-defined clinical entity of synergistic and polymicrobial necrotizing fasciitis of the perineum. It is characterized by obliterating endarteritis of the subcutaneous arteries leading to gangrene of the subcutaneous tissue and overlying skin(4). Necrosis is caused by the dissemination of microorganisms into the subcutaneous space (platelet aggregation favored by aerobes and heparinase produced by anaerobes). Together with local edema, hypoxia appears due to local alterations in blood supply, which favors the development of anaerobic microorganisms that produce hydrogen and nitrogen, which accumulate in the tissues, causing crepitus5. This condition is rare in women, but progresses rapidly with high mortality6. Approximately 25% of cases have unknown etiology, although there are known risk factors that include diabetes mellitus, alcohol abuse, renal and hepatic hypertension, obesity, smoking, immunodeficiency diseases and pre-existing lesions2.
There are differences in characteristics of Fournier's gangrene between men and women, due to anatomical differences6. The vagina allows drainage of pelvic contents and secretion, which contributes to the low incidence7. However, when the disease occurs, it progresses with a more severe and potentially fatal course. The mortality rate in women is up to 50%(6). It usually originates from microorganisms of the genitourinary and anorectal tract or the skin of the genital area8. The most common etiological agent is Escherichia coli, although in about 60% of cases the infection is polymicrobial, generally commensal bacteria that become pathogenic. This forces the initial use of schemes with combinations of broad-spectrum antibiotics9.
The clinical diagnosis of vulvar Fournier's gangrene is difficult due to its variable clinical presentation. The most common manifestations are edema, erythema, pain, local swelling and fever2. Gas production by anaerobic germs that accumulates in the subcutaneous cellular tissue is clinically evident by the presence of crepitus. However, crepitus and hemorrhagic blisters are present in 20% to 50% of cases4. The extent of infection can be dramatic and lethal, both in nature and clinical course. There may be a delay of 2 to 7 days between the first symptoms and medical attention, which negatively influences the prognosis of patients6.
Fournier's gangrene has four clinical phases. The first phase lasts 14 to 48 hours and is characterized by an insidious and nonspecific course with hardening of the affected area, accompanied by pruritus, edema and erythema. In the invasive phase (second phase), regional inflammatory manifestations appear, such as perineal pain, erythema, and fever. The third phase (necrotic phase) presents with systemic manifestations and worsening of the general condition. Half of the cases may progress to sepsis. Locally, there is tension, hemorrhagic phlyctens that evolve to necrosis and may extend to anatomical regions of continuity between the fasciae of the perineum and abdomen in the most severe cases. The fourth phase of spontaneous restoration is characterized by repair of the necrotic tissues, with slow healing, initial deep granulation with subsequent epithelialization for several months1.
Blood cultures -positive in a quarter of the casesand laboratory tests can help to guide antibiotic therapy, establish prognostic indices and evaluate the evolution of the treatment. Imaging studies are of relative importance, since they make it possible to observe abscesses in the area. The presence of subcutaneous gas can be detected by radiography, ultrasound, computed tomography and magnetic resonance imaging. Ultrasonography is the most useful method, since it allows differential diagnosis with other less intense pathological processes, such as edema or cellulitis3.
Early appropriate management is crucial in patients with vulvar Fournier's gangrene. Drainage and broad-spectrum antibiotic therapy against aerobic and anaerobic microorganisms, regardless of Gram stain and culture results, should be indicated immediately after diagnosis(4.5). The definitive treatment is early and active radical debridement, with several repeated procedures before the infection is considered resolved, with or without colostomies. Different studies have described that the rate of propagation of tissue destruction is as close to 2 or 3 centimeters / hour1. The aim of the procedure is to remove all non-viable tissue, stop the progression of infection and avoid systemic complications. Colostomy is a controversial therapeutic option in cases with perineal involvement. Although it was considered fundamental in preventing fecal contamination and improving wound healing conditions, its performance is associated with higher mortality10. There is evidence that cleaning the perineal wound improves healing, avoiding colostomy9,11.
Despite appropriate treatment, the associated mortality is high, so aggressive and multidisciplinary management is necessary, even with the possibility of admission to the intensive care unit. Mortality is directly linked to the severity of gangrene. Factors associated with higher mortality are anorectal origin, extensive disease commonly secondary to late diagnosis, advanced age, and clinical conditions at presentation, including sepsis with multiorgan dysfunction7.
Genital reconstruction in cases of Fournier's gangrene in women is a different problem than in men and must be focused on the anatomical characteristics of the vagina and vulva12,13. Surgery is a challenge, since the female genitalia have complex functional characteristics. The vagina must maintain its cylindrical shape to allow sexual intercourse, while the vulva must act as the gateway. In addition, the vulva protects both the vagina and the urethra from direct exposure and contributes to sexual activity14. Therefore, the female genitalia must be reconstructed to maintain the patient's quality of life. Covering only the defect would result in a vulva without volume, leading to the appearance of ectropion, direct exposure of the vagina, irregular direction of urination and sexual dissatisfaction. Skin grafts or flaps from the thigh area are used to reconstruct the female genitalia, but produce severe postoperative complications15.
In conclusion, vulvar Fournier's gangrene is a progressive and potentially fatal condition, which makes it a true surgical emergency. Its clinical characteristics should be considered in order to establish the most appropriate treatment. Delay in both diagnosis and surgery is responsible for the high mortality. Aggressive treatment, including early surgical intervention, broad-spectrum antibiotic therapy and adequate postoperative care, leads to improved prognosis.
REFERENCES
1. Kranz J, Schlager D, Anheuser P, Mühlstädt S, Brücher B, Frank T, et al. Desperate need for better management of Fournier's gangrene. Cent European J Urol. 2018;71(3):3605. doi: 10.5173/ceju.2018.1740 [ Links ]
2. Ioannidis O, Kitsikosta L, Tatsis D, Skandalos I, Cheva A, Gkioti A, et al. Fournier's Gangrene: lessons learned from multimodal and multidisciplinary management of perineal necrotizing fasciitis. Front Surg. 2017;4:36. doi: 10.3389/fsurg.2017.00036 [ Links ]
3. Ballard DH, Mazaheri P, Raptis CA, Lubner MG, Menias CO, Pickhardt PJ, et al. Fournier gangrene in men and women: Appearance on CT, ultrasound, and MRI and what the surgeon wants to know. Can Assoc Radiol J. 2020;71(1):30-9. doi: 10.1177/0846537119888396 [ Links ]
4. Singh A, Ahmed K, Aydin A, Khan MS, Dasgupta P. Fournier's gangrene. A clinical review. Arch Ital Urol Androl. 2016;88(3):157-64. doi: 10.4081/aiua.2016.3.157 [ Links ]
5. George J, Raja A, Chun Hei Li D, Joshi H. Fournier's gangrene: diagnosis and management aided by repeated clinical examination and ultrasound. BMJ Case Rep. 2017;2017:bcr2016217409. doi: 10.1136/bcr-2016-217409 [ Links ]
6. Czymek R, Frank P, Limmer S, Schmidt A, Jungbluth T, Roblick U, et al. Fournier's gangrene: is the female gender a risk factor? Langenbecks Arch Surg. 2010;395(2):173-80. doi: 10.1007/s00423-008-0461-9 [ Links ]
7. Hong KS, Yi HJ, Lee RA, Kim KH, Chung SS. Prognostic factors and treatment outcomes for patients with Fournier's gangrene: a retrospective study. Int Wound J. 2017;14(6):1352-8. doi: 10.1111/iwj.12812 [ Links ]
8. Roghmann F, von Bodman C, Tian Z, Brock M, Löppenberg B, Braun K, et al. Outcome prediction in patients with Fournier's gangrene. Urologe A. 2013;52(10):1422-9. doi: 10.1007/s00120-013-3173-x [ Links ]
9. Malik AM, Sheikh S, Pathan R, Khan A, Sheikh U. The spectrum of presentation and management of Fournier's gangrene--an experience of 73 cases. J Pak Med Assoc. 2010;60(8):617-9. [ Links ]
10. Lin HC, Chen ZQ, Chen HX, He QL, Liu ZM, Zhou ZY, et al. Outcomes in patients with Fournier's gangrene originating from the anorectal region with a particular focus on those without perineal involvement. Gastroenterol Rep (Oxf). 2019;7(3):212-7. doi: 10.1093/gastro/goy041 [ Links ]
11. Taken K, Oncu MR, Ergun M, Eryilmaz R, Demir CY, Demir M, et al. Fournier's gangrene: Causes, presentation and survival of sixty-five patients. Pak J Med Sci. 2016;32(3):746-50. doi: 10.12669/pjms.323.9798 [ Links ]
12. Hunter CL, Skinner EC, Lee GK. Reconstruction with pedicled anterolateral thigh flap after wide local excision of extramammary Paget's disease: A case report and comprehensive literature review. Eplasty. 2015;15:e26. [ Links ]
13. Chen YC, Scaglioni MF, Kuo YR. Profunda artery perforator-based V-Y rotation advancement flap for total vulvectomy defect reconstruction--A case report and literature review. Microsurgery. 2015;35(8):668-71. doi: 10.1002/micr.22498 [ Links ]
14. Nappi RE, Particco M, Biglia N, Cagnacci A, Di Carlo C, Luisi S, et al. Attitudes and perceptions towards vulvar and vaginal atrophy in Italian post-menopausal women: Evidence from the European REVIVE survey. Maturitas. 2016;91:74-80. doi: 10.1016/j.maturitas.2016.06.009 [ Links ]
15. Di Donato V, Bracchi C, Cigna E, Domenici L, Musella A, Giannini A, et al. Vulvo-vaginal reconstruction after radical excision for treatment of vulvar cancer: Evaluation of feasibility and morbidity of different surgical techniques. Surg Oncol. 2017;26(4):511-21. doi: 10.1016/j.suronc.2017.10.002n [ Links ]
Ethical responsibilities: Protection of people. The authors declare that the procedures followed were in accordance with the ethical standards of responsible human experimentation committee and in accordance with World Medical Association and Declaration of Helsinki.
Confidentiality of data: The authors declare that we have followed the protocols of the Central Hospital “Dr. Urquinaona” on the publication of patient data.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and / or subjects referred to in the article. This document is in the possession of the corresponding author.
Financing: The authors certify that we have not received financial support, equipment, work personnel or in kind from people, public and / or private institutions to carry out the study.
Received: October 12, 2020; Accepted: November 15, 2020











 texto en
texto en