Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.2 Lima abr./jun. 2021
http://dx.doi.org/10.31403/rpgo.v67i2324
Case report
Hysteroscopic resection of cervical ectopic pregnancy following in vitro fertilization
1. Ginecologist Obstetrician, Assistant Physician Departament of Gynecology and Obstetrics, Hospital Regional Docente de Trujillo, Peru
2. Centro de Reproducción Asistida FERTÍLITA - Genética y Reproducción In Vitro, Trujillo, Peru
Cervical ectopic pregnancy is a low frequency pathology, which presents a high risk of hemorrhage and loss of fertility due to the need for hysterectomy. We present a case of cervical ectopic pregnancy after in vitro fertilization successfully treated with hysteroscopic resection.
Key words: Ectopic pregnancy; Hysteroscopy; Fertilization in vitro
Introduction
The blastocyst, after transit through the fallopian tubes, normally implants in the endometrial lining of the uterine cavity. Implantation elsewhere is considered ectopic and accounts for 0.5 to 1.5% of all first trimester pregnancies. This small proportion represents 3% of all pregnancy-related deaths. About 95% of ectopic pregnancies implant in the various segments of the fallopian tube. The ampulla (70%) is the most frequent site, followed by isthmic (12%), fimbrial (11%) and interstitial (2%) pregnancies. The remaining 5 percent of ectopic pregnancies are implanted in the ovary, the peritoneal cavity, the scar of a previous cesarean section and the cervix1,2.
Cervical ectopic pregnancy (CEP) accounts for less than 1% of all pregnancies, with an estimated incidence of one in 2,500 to one in 18,000 pregnancies. The blastocyst implants in the endocervical canal1.
The CEP is associated with massive hemorrhage, and the most common treatment is hysterectomy. However, measurement of β-subunit chorionic gonadotropin (β-hCG) and improved ultrasound resolution have induced the development of multiple conservative treatments that limit morbidity and mortality and preserve fertility. Given the rarity of the disease, the most effective form of treatment continues to be investigated1.
We report a case of CEP after in vitro fertilization (IVF) successfully treated by hysteroscopic resection.
Case report
A 34-year-old female patient G 2 P 0020 was seen for follow-up 14 days after an in vitro fertilization procedure with her own egg and delayed embryo transfer on day 5. She was asymptom atic and had an β-hCG result of 409.4 mIU/mL.
Physical examination was normal. One week later, transvaginal ultrasound showed a 16 mm gestational sac at the cervical isthmic level containing an embryo with a craniocaudal length of 4.9 mm (6 weeks 2 days) and cardiac activity present (Figure 1).
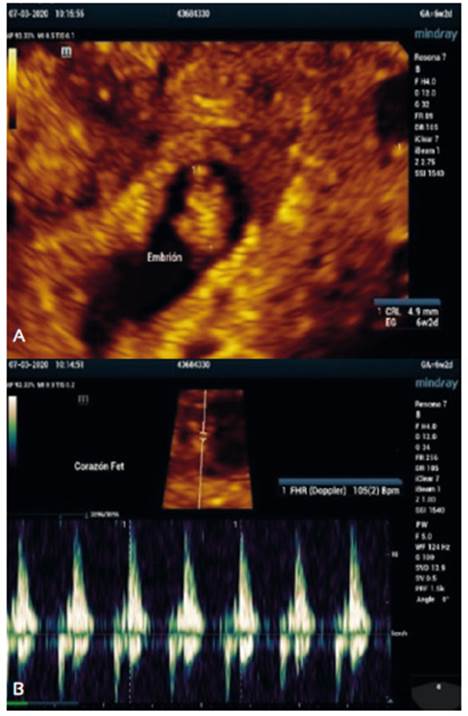
Figure 1. A: Intracervical gestational sac shows a 6-week embryo with cardiac activity present. B: Embryo cephalo-caudal length 4.9 mm.
The patient had a history of polycystic ovarian syndrome, a 5-year history of infertility and hysteroscopic polypectomy for endometrial polyps.
Two weeks later, she was still asymptomatic and had β-hCG of 10,267 mIU/mL. Ultrasound showed thickened endometrial echo, decidualized, barrel-shaped cervix, distended endocervical canal due to the presence of a 27 mm gestational sac and embryo with CSF of 16.3 mm and cardiac activity (Figure 2).
Due to genetic desire, treatment was attempted with methotrexate at a single dose of 1 mg/kg body weight, intramuscularly. Four days later, the β-hCG control was 13,251 mIU/mL and the ultrasound showed a viable fetus with cardiac activity present. Due to the findings, it was decided to perform hysteroscopic resection of the cervical ectopic pregnancy in order to preserve the uterus.
On evaluation under regional anesthesia, the cervix was found to be soft, enlarged and the external cervical os partially open, with scant bleeding. Diagnostic hysteroscopy was initially performed to determine the exact location of the gestational sac. It was entered through the endocervical canal, finding the gestational sac with implantation site on the right lateral side of the lower half of the canal. Then, without the need for cervical dilatation, a 26 Fr bipolar resectoscope was inserted, using 0.9% sodium chloride as distension medium. For the excision of the gestational sac, the loop type cutting electrode (40 watts) was used until the extraction of the entire gestational product was achieved (Figure 3). Hemostasis was performed using the barrel and ball electrodes (60 watts). Upon digital evaluation of the implantation site, a large cavity was found, so an intracervical tamponade consisting of the balloon of an 18 French Foley catheter inflated with 25 mL of sodium chloride was placed (Figure 4).
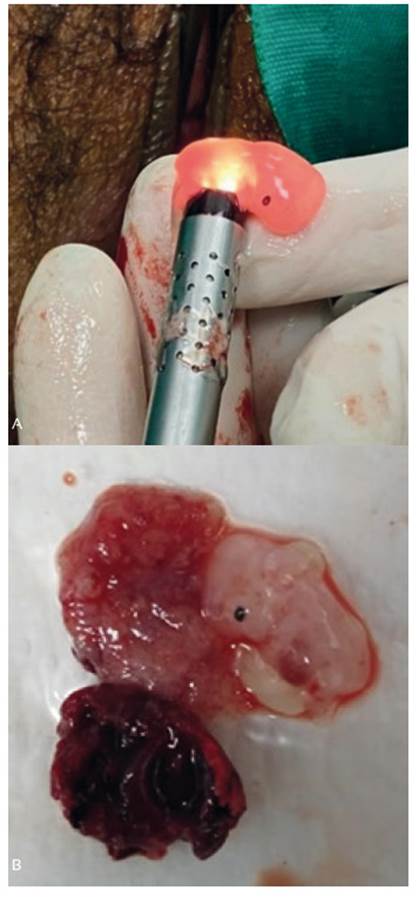
Figure 3. A. Embryo extracted by resectoscope. B: Products of pregnancy: embryo and chorionic villi.
Blood loss during the operation was estimated at 80 mL. Surgical time was 20 minutes. The resected tissue was sent to pathology. The patient was discharged from the hospital 48 hours after surgery; there was no need for blood transfusion. The catheter was removed after three days and, on ultrasound, the endocervical canal was found to be dilated and the wall of the endocervical canal appeared heterogeneous. The β-hCG control was 97 mIU/mL at 7 days after surgery and at two weeks the value was less than 5 mIU/ mL.
Discussion
ECP is produced by the implantation of the blastocyst in the endocervical canal. Its etiology is unknown. Previous cervical or uterine surgery, such as history of curettage or cesarean section, play an associated role. Another theory involves rapid transport of the blastocyst to the endocervical canal before there is a receptive endometrium. Other predisposing factors are endometritis, leiomyomatosis, intrauterine devices and in-vitro fertilization3.
Until a few years ago, the diagnosis was made when evacuation of a suspected miscarriage was performed. Curettage often resulted in uncontrollable bleeding requiring hysterectomy.
Treatment options for CEP include five categories: tamponade, reduction of blood supply, removal of trophoblastic tissue, intraamniotic injection of feticidal fluid, and systemic chemotherapy. The choice of treatment depends on the gestational age, the clinical picture, and the desire to maintain fertility4. However; there are no evidence-based recommendations.
Some authors3,4 suggest that systemic methotrexate can be indicated in clinically stable patients if the gestational age by ultrasound is less than or equal to 8 weeks and cardiac activity is not visualized. If gestational age is 9 weeks or more, with presence of cardiac activity, intraamniotic addition of potassium chloride is required. CEP greater than 12 weeks justifies hysterectomy. In contrast, in patients with hemorrhage, treatment options are Foley catheter balloon tamponade, large vessel ligation, or angiographic embolization. Hysterectomy is recommended for massive incoercible bleeding and hemodynamic instability5.
Reports of the use of systemic chemotherapy with methotrexate are controversial. Frequently more than one method is used to terminate CEP. Troncoso et al.6 described two cases of CEP; both cases corresponded to gestations of less than seven weeks. They were initially treated with systemic methotrexate, but due to the presence of heavy bleeding, cervical curettage and McDonald type cerclage were performed.
In the present case, due to the desire for fertility, it was initially decided to apply systemic methotrexate. However, when no favorable response was found, it was decided to surgically remove the trophoblastic tissue by hysteroscopic resection combined with cervical tamponade using the Foley catheter balloon.
Hysteroscopic evaluation of CEP was described in 1922 by Roussis et al.7. They used hysteroscopy to visualize CEP following failure of systemic treatment with methotrexate. Hysteroscopy confirmed minimal vascularization in the endocervical canal, so they performed tissue aspiration. Ash and Farrell8 published the first successful case of hysteroscopic resection of a 7-week cervical gestation with cardiac activity. Sardo et al.9 reported a successfully treated cervical-isthmic pregnancy with bipolar resectoscopy after failure of systemic and local methotrexate administration. As in our case, surgical time was short, recovery was rapid and blood transfusion was not required. Igbokwe et al.10 reported the case of a 6-week cervical gestation in a hemodynamically stable nullipara who underwent hysteroscopic resection combined with cervical curettage under ultrasound guidance and systemic injection of methotrexate. Kim et al.11 published 10 cases of CEP successfully treated by hysteroscopic resection after irrigation of the uterine cavity with a 3.5% hydrogen peroxide (H2O2). Jozwiak et al.12 also had success with hysteroscopic resection of a cervical heterotopic pregnancy achieved by intracytoplasmic sperm injection. The intrauterine pregnancy continued and they obtained a term newborn.
There are several successful studies when hysteroscopic resection of CEP is used as the sole treatment. Alanís et al.13 report a case of CEP treated successfully by ablation with bipolar surgical hysteroscope. The most extensive study found in the literature is by Tanos et al.14, who conclude that surgical hysteroscopy can be used as sole treatment in CEP less than 8 weeks old.
Another work where hysteroscopic resection of CEP was chosen as the only treatment is the one described by Salazar and Vargas15, who publish 7 cases of CEP submitted to hysteroscopic resection using bipolar energy; bleeding fluctuated between 30 to 380 mL; the authors were able to conserve the uterus, and 4 of the patients even managed to become pregnant spontaneously or with assisted reproduction techniques. Recently, the two-step technique of the hysteroscopic approach to the CEP was described, in which initially they entered with a 5 mm diagnostic hysteroscope and then with a 10 mm resectoscope, managing to remove the CEP safely and with minimal bleeding16.
There is a lack of scientific evidence on the conservative treatment of CEP; there is only isolated information. This leads to a lack of standardization in treatment protocols.
Mortality rates in the case of CEP have ostensibly decreased. However, the different conservative therapeutic options, especially chemotherapy, are not always satisfactory and often result in mutilating surgeries with the consequent loss of fertility.
Nowadays, thanks to technological advances in the area of gynecological endoscopy, effective, safe and reproducible surgery can be performed, optimizing hospital resources and with minimal complications. The hysteroscope allows direct visualization and complete resection of the CEP, obtaining adequate hemostasis and rapid resolution, thus avoiding longer hospital stay and prolonged follow-up8,12,14.
Based on the literature review on cervical pregnancy, hysteroscopic resection is oriented as the treatment of choice, due to its efficacy, safety, and, above all, for preserving future conception.
Acknowledgements
Special thanks to the assisted reproduction center FERTÍLITA - Genética y Reproducción In Vitro.
REFERENCES
1. Cunningham FG, Leveno KJ, Bloom S L, Dashe JS, Hoffman BL, Casey BM, Spong CY. Williams Obstetrics. 25° ed., 2018. Mc Graw-Hill Education, New York, USA. [ Links ]
2. Bouyer J, Coste J, Fernández H, Pouly JL, Job SN. Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Hum Reprod. 2002;17:3224. doi:10.1093/humrep/17.12.3224 [ Links ]
3. Singh S. Diagnosis and management of cervical ectopic. J Hum Reprod Sci. 2013;6:273-6. doi:10.4103/0974-1208.126312 [ Links ]
4. Leeman L, Wendland C. Cervical ectopic pregnancy. Arch Fam Med. 2000;9:72-7, doi:10.1001/archfami.9.1.72 [ Links ]
5. Bueno G, Martínez-Gómez E, Pascual A, Martínez-Cabañero R, García-Garrido C, Tello A, González de Merlo G. Surgical treatment by hysterectomy of a cervical ectopic pregnancy. Clin Invest Gin Obst. 2008;35:144-8. [ Links ]
6. Troncoso F, Cardone X, Rondini C, Troncoso C. Embarazo ectópico cervical. Diagnóstico y tratamiento conservador con cerclaje cervical. Rev Chil Obstet Ginecol. 2005, 70: 257- 60. doi:10.4067/S0717-75262005000400010 [ Links ]
7. Roussis P, Fleischer A, Herbert C. Cervical pregnancy. A case report. J Reprod Med. 1992;37:479-81. [ Links ]
8. Ash S, Farrell S. Hysteroscopic resection of a cervical ectopic pregnancy. Fertil Steril. 1996;66:842-4. doi:10.1016/S0015-0282(16)58649-X [ Links ]
9. Sardo A, Alviggi C, Zizolfi B, Spinelli M, De Rosa P, De Placido G, Nappi C. Cervico-isthmic pregnancy successfully treated with bipolar resection following methotrexate administration: case report and literature review. Reprod Biomed Online. 2013;26:99-103. doi:10.1016/j.rbmo.2012.10.005 [ Links ]
10. Igbokwe N, Jeyanesan D, Mehta A. Management of live cervical ectopic pregnancy. Ann Clin Lab Sci. 2020;8:1-3. doi:10.36648/2386-5180.8.1.310 [ Links ]
11. Kim J, Nam K, Kim T, Lee H, Lee K. Hysteroscopic management of cervical pregnancy with Intrauterine irrigation with H2O2. J Minim Invasive Gynecol. 2008;15:627-30. doi:10.1016/j.jmig.2008.06.006 [ Links ]
12. Jozwiak E, Ulug U, Akman M, Bahceci M. Successful resection of a heterotopic cervical pregnancy resulting from intracytoplasmic sperm injection. Fertil Steril. 2003;79:428-30. doi:10.1016/s0015-0282(02)04662-9 [ Links ]
13. Alanís J, Brindis A, Martínez M. Embarazo ectópico cervical. Tratamiento histeroscópico, presentación de un caso. Gynecol Obstet Mex. 2015;83:302-7. [ Links ]
14. Tanos V, ElAkhras S, Kaya B. Hysteroscopic management of cervical pregnancy: Case series and review of the literature. J Gynecol Obstet Hum. 2019;48:247-53. doi:10.1016/j.jogoh.2018.05.001 [ Links ]
15. Salazar C, Vargas V. Conservative endoscopic treatment of cervical ectopic pregnancy by operative hysteroscopy. Rev Enf Trac Gen Inf. 2014;8:6-13. [ Links ]
16. Mangino FP, Romano F, Di Lorenzo G, De Santo D, Scrimin F, Ricci G. Total hysteroscojpic treatment of cervical pregnancy: the 2-step technique. J Minim Invasive Gynecol. 2019;26:1011-2. doi:10.1016/j.jmig.2019.01.009 [ Links ]
Received: January 01, 2021; Accepted: February 15, 2021











 texto en
texto en 





