Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.2 Lima Apr./Jun. 2021
http://dx.doi.org/10.31403/rpgo.v67i2328
Case report
Postpartum ovarian vein thrombosis
1. Specialist in Gynecology and Obstetrics, Obstetrics and Gynecology Service, Hospital Central “Dr. Urquinaona”, Maracaibo, Estado Zulia, Venezuela
Ovarian vein thrombosis is a rare but serious condition that causes abdominal pain and fever and is most commonly seen during the immediate postpartum period. It may also be associated with pelvic inflammatory disease, neoplasms and pelvic surgical procedures. In the differential diagnosis of acute abdomen, consider it in a febrile puerperal patient with abdominal pain without apparent focus or response to antibiotic therapy. A high index of suspicion is necessary for timely diagnosis and management, especially in cases that simulate an acute abdomen. Complications can be significant and diagnosis is based on careful examination of radiographic findings. The diagnostic test of choice, with high sensitivity and specificity, is contrast computed tomography, Thromboprophylaxis and broad-spectrum antibiotics are effective as initial treatment in cases without pulmonary embolism or extensive involvement of the thrombus in the inferior vena cava. A case of postpartum ovarian vein thrombosis is presented.
Key words: Ovary; Venous thrombosis; Postpartum period
Introduction
Ovarian vein thrombosis is a serious but relatively rare of the immediate postpartum period, complicating approximately 0.05% - 0.18% of vaginal deliveries and 2% of cesarean deliveries1. It also is associated with abdominal and pelvic gynecological surgery, gynecological neoplasms, pelvic-intestinal inflammatory disease and other conditions that cancause thrombus formation2.
Symptomatology is vague and not very specific, but the most common symptoms are fever and abdominal pain during the puerperium. Be-cause of this, the use of imaging studies is necessary to establish the diagnosis and avoid potentially fatal complications. Therefore, early recognition and timely treatment are essential in this condition3. A case of postpartum ovarian vein thrombosis is presented.
Clinical case
This is a 43-year-old patient, gestations 2, para 2, who came to the emergency room with moderate to severe abdominal pain in the left lower quadrant, with two days of evolution, radiating to the lumbar region; it was accompanied by fever, chills, nausea, vomiting, but without alteration of bowel habits. The patient had a history of uncomplicated vaginal delivery 7 days before the onset of symptoms. The pregnancy had passed without complications or evidence of thrombophilia in prenatal controls. She denied smoking, significant medical and surgical history, and family history of cardiovascular disease, hematological disorders or hypercoagulability.
Physical examination showed that she was febrile (39.4 degrees C), with a heart rate of 105 beats per minute, respiratory rate 19 breaths per minute, blood pressure of 110/75 mmHg and oxygen saturation of 97% on room air. Clinical examination showed audible vesicular murmur in both lung fields, without aggregates. The abdomen was soft, depressible, with severe pain on palpation of the left hypochondrium and iliac fossa without evidence of defense. On gynecological examination, the uterus was well involuted, with severe pain on palpation of the anterior vaginal wall and during mobilization of the uterus. The lochia were normal, with no evidence of vaginal discharge, fetid discharge or abnormal genital bleeding.
Laboratory tests showed leukocytosis of 10,880 cells / mL with neutrophilia (87%), hemoglobin 10.6 g / dL, hematocrit of 34.4% and platelets 267,000 / mL. The C-reactive protein concentration was 5.0 mg / L. The values of the hepatic and kidney functional profile, electrolytes, coagulation profile and urine examination were within normal limits. Urine and blood culture results were negative.
Pelvic ultrasound evaluation showed a puerperal uterus, heterogeneous endometrium of 10-millimeter, normal adnexa and absence of free fluid in the abdominal cavity. No evidence of pelvic abscesses or presence of ovulation debris was found. Abdominopelvic computed tomography with intravenous contrast showed fluid along the anterior aspect of the kidney and left psoas muscle, extending to the left side of the uterus and the region of the left renal vein, with evidence of thrombosis of the left ovarian vein up to the junction with the inferior vena cava (Figure 1). The cecal appendix was normal.
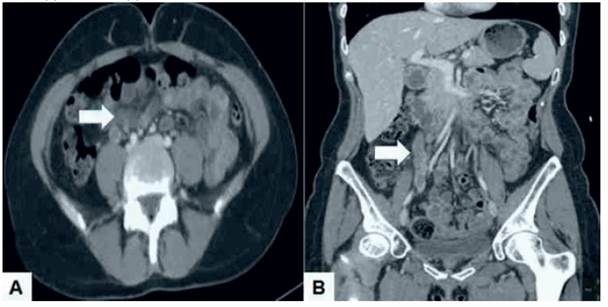
Figure 1 (A) Transverse and (B) sagitta l computed tomography images. The arrow indicat es thrombosis of the left ovarian vein.
In view of the findings, it was decided to rule out deep vein thrombosis. Both chest computed tomography and lower extremity Doppler ultrasound showed no evidence of concomitant venous thrombosis. Ultrasonography showed that both kidneys were normal. Basic hemostasis tests and hypercoagulability studies, which in cluded prothrombin and partial thromboplastin time, factor V Leiden, lupus anticoagulant and cardiolipin antibody, were within normal limits.
The patient was hospitalized for anticoagulation with intravenous heparin and intravenous antibiotic therapy (cefuroxime, metronidazole, and gentamicin). At 24 hours, treatment with low molecular weight heparin was started. The patient responded adequately to treatment, with resolution of leukocytosis, pain and fever after 48 hours of treatment. She was discharged 5 days later, in good general condition; heparin treatment was suspended and oral warfarin was started, controlling by international normalized index.
During follow-up, she has not experienced recurrence of symptomatology, while continuing with therapeutic anticoagulation. After 6 months, resolution of the thrombus and complete recanalization was shown by abdominal computed tomography, and anticoagulant treatment was discontinued.
Discussion
Postpartum ovarian vein thrombosis is a complication due to the appearance of an intraluminal thrombus in any part of the vein during the puerperium2. Asymptomatic cases are the most common and its evolution is generally benign, with a 30% incidence of thrombosis of the veins (iliac and ovarian)4. This condition is classically a process associated with pregnancy, but it can also arise in non-puerperal contexts, such as endometritis, pelvic inflammatory disease, malignant neoplasms, thrombophilia, inflammatory bowel disease, and pelvic and gynecological surgeries4-6. Risk factors for this condition are multiparity, smoking, obesity, puerperal bacteremia and thrombophilia, both inherited and acquired. Anaerobic bacteria can contribute to the pathology by generating endothelial lesions. Anaerobic bacteria that are present in the lower genital tract can reach the ovarian veins through the uterine and vaginal veins3.
Pregnancy is a hypercoagulable state characterized by increased platelet adhesion and decreased fibrinolysis. Erythrocyte mass increases by approximately 30%, while plasma volume in-creases by 50%6. Hypercoagulability, venous stasis and endothelial injury (Virchow's triad) are the most frequent causes of ovarian vein thrombosis and pregnancy is an example of this triad7. First, the uterus increases in size, with increased blood flow and increased stasis of the pelvic and lower extremities veins; these vascular changes remain until 72 hours after delivery. Secondly, during pregnancy and the puerperium there is a state of hypercoagulability. Finally, endothelial trauma can occur during delivery or due to local inflammation. As a result, pregnant women are five times more likely to develop deep vein thrombosis compared to non-pregnant subjects8.
The right ovarian vein drains directly, and at an acute angle, into the inferior vena cava, while the left vein drains, usually at a right angle, into the renal vein. In addition, anterograde blood flow in the right ovarian vein favors bacterial infection, in contrast to retrograde blood flow in the left ovarian vein. These differences make the right ovarian vein more susceptible to compression, since 70% to 90% of cases occur due to involvement of the right ovarian vein. The left ovarian vein, as in the present case, and both ovarian veins are affected in 6% and 14% of cases, respectively9. Other factors that may contribute to this is the greater length, lack of competent valves of the right ovarian vein, together with the greater risk of compression during physiological dextrorotation of the pregnant uterus leading to compression of the nearby venous system1,7.
Postpartum ovarian vein thrombosis has a vague and variable presentation. It should be suspected during the puerperium, especially in those patients with nonspecific symptoms that do not respond to conventional treatment and is usually found when looking for other causes of abdominal pain. The most common symptoms are pelvic or lower back pain, fever, tachycardia, leukocytosis, and palpable pelvic tumor up to 4 weeks after delivery. However, 90% of cases appear in the first ten days10. Complications, although rare, can be fatal and include septic thrombophlebitis, acute ureteral obstruction, extension of the thrombus to the inferior vena cava or left renal vein (25% to 30%), and pulmonary embolism. The incidence of pulmonary embolism varies widely between 0.15% and 0.33% in untreated patients with a mortality close to 4%. The risk of developing complications is asso ciated with the etiology of the condition2.
Imaging studies are essential to establish the diagnosis. Ultrasound is the initial imaging study of choice, since it is inexpensive, widely available and does not require radiation or contrast. Findings of tubular-shaped, hypoechoic tumor in the adnexa and / or iliac fossa are nonspecific for this pathology. Among its disadvantages, it has a relatively low sensitivity, which depends on the operator’s experience, and overlying intestinal gas can limit visualization. Doppler ultrasound improves sensitivity by clearly identifying the ovarian veins and documenting resolution of the condition11. Both helical computed tomography angiography and conventional venography were considered the standard methods for diagnosis. However, CT and MRI images are equally sensitive for detecting postpartum ovarian vein thrombosis. Contrast-enhanced computed tomography has high sensitivity (63% to 100%) and specificity (78% to 90%). The diagnosis is based on the presence of the Zerhouni criteria:enlarged vein, low density venous lumen and well-defined vascular wall with perivascular inflammatory strands. However, differentiation of the thrombosed ovarian vein from the appendix can be difficult. Magnetic resonance imaging offers better sensitivity and specificity (92% to 100% and 100%, respectively) and allows visual ization of the entire course of the ovarian veins in patients with inconclusive tomography or ultrasound images12.
The differential diagnosis of postpartum ovarian vein thrombosis can be any of the conditions that cause abdominal pain located in the lower hemiabdomen. Among the most common conditions that need to be differentiated are acute appendicitis, intestinal volvulus, broad ligament hematoma, adnexal torsion, pedunculated uterine fibromyoma torsion, pelvic abscess, pyelonephritis, retroperitoneal lymphadenopathy, and puerperal endometritis1,8.
There is no clear consensus on the optimal treat ment of postpartum ovarian vein thrombosis. Because of the increased risk of potentially lethal pulmonary embolism, most reviews support anticoagulant therapy as the mainstay of treatment. The application of deep vein thrombosis guidelines is reasonable, as most experts consider that rare thromboses should be treated as deep vein thrombosis of the lower extremities13. The drugs traditionally used are heparin and warfarin. Most authors suggest the use of low molecular weight heparin, but there is no agreement on the initiation, dose and duration of treatment. Resolution of thrombosis occurs between 7 to 14 days of treatment14. However, thrombosis may not resolve with brief anticoagulant treatment and they recommend prophylactic anticoagulation for 3 to 6 months, until resolution of the thrombus or calcification can be confirmed radiologically on follow-up imaging2.
Broad-spectrum antibiotics are used for 7 to 10 days as empirical treatment for postpartum endometritis when fever and abdominal pain are present14. Although surgery in the initial treatment of postpartum ovarian vein thrombosis is controversial, some prefer surgery for complicated cases associated with recurrent pulmonary embolism despite medical treatment and when there is contraindication to the use of anticoagulants15. In some cases with high risk of pulmonary embolism it may be necessary to perform endovascular or surgical procedures, such as thrombectomy, inferior vena cava filters or ovarian vein ligation. Secondary prevention is based on the administration of low molecular weight heparin after delivery in patients with risk factors1,3.
The mortality rate in cases of postpartum ovarian vein thrombosis can exceed 50% in untreated cases. However, with the use of anticoagulants, mortality decreases to below 5%5. Recurrence is low in subsequent pregnancies, but for patients with underlying coagulation disorders, throm boprophylaxis is recommended.
In conclusion, postpartum ovarian vein thrombosis is an uncommon complication. The clinical presentation is nonspecific and should always be considered in the differential diagnosis of abdominal pain during the puerperium. Imaging techniques help to identify the vessel occluded by a thrombus. Medical treatment with anticoagulants and broad-spectrum antibiotics is effective in cases without associated complications. However, the duration of treatment is controversial.
REFERENCES
1. Lerouge J, Sanguin S, Gondry J, Sergent F. Management of postpartum ovarian vein thrombosis. The experience of Amiens university hospital. Gynecol Obstet Fertil. 2016;44(2):88-95. doi: 10.1016/j.gyobfe.2015.11.010 [ Links ]
2. Rottenstreich A, Da'as N, Kleinstern G, Spectre G, Amsalem H, Kalish Y. Pregnancy and non-pregnancy related ovarian vein thrombosis: Clinical course and outcome. Thromb Res. 2016;146:84-8. doi: 10.1016/j.thromres.2016.09.001 [ Links ]
3. Hoffmann J, Amaya B, Grothoff M, Schrock C, Lampe D. Ovarian vein thrombosis as a rare cause of postpartal abdominal pain: a case report. Arch Gynecol Obstet. 2012;286(5):1331-2. doi: 10.1007/s00404-012-2408-1 [ Links ]
4. Kodali N, Veytsman I, Martyr S, Lu K. Diagnosis and management of ovarian vein thrombosis in a healthy individual: a case report and a literature review. J Thromb Haemost. 2017;15(2):242-5. doi: 10.1111/jth.13584 [ Links ]
5. Jenayah AA, Saoudi S, Boudaya F, Bouriel I, Sfar E, Chelli D. Ovarian vein thrombosis. Pan Afr Med J. 2015;21:251. doi: 10.11604/pamj.2015.21.251.6908 [ Links ]
6. Brenner B, Arya R, Beyer-Westendorf J, Douketis J, Hull R, Elalamy I, et al. Evaluation of unmet clinical needs in prophylaxis and treatment of venous thromboembolism in atrisk patient groups: pregnancy, elderly and obese patients. Thromb J. 2019;17:24. doi: 10.1186/s12959-019-0214-8 [ Links ]
7. Parino E, Mulinaris E, Saccomano E, Gallo JC, Kohan G. Postpartum ovarian vein thrombophlebitis with staphylococcal bacteremia. Case Rep Infect Dis. 2015;2015:589436. doi: 10.1155/2015/589436 [ Links ]
8. Girolami A, Treleani M, Bonamigo E, Tasinato V, Girolami B. Venous thrombosis in rare or unusual sites: a diagnostic challenge. Semin Thromb Hemost. 2014;40(1):81-7. doi: 10.1055/s-0033-1363471 [ Links ]
9. Basili G, Romano N, Bimbi M, Lorenzetti L, Pietrasanta D, Goletti O. Postpartum ovarian vein thrombosis. JSLS. 2011;15(2):268-71. doi: 10.4293/108680811X13071180406673 [ Links ]
10. Salomon O, Dulitzky M, Apter S. New observations in postpartum ovarian vein thrombosis: experience of single center. Blood Coagul Fibrinolysis. 2010;21(1):16-9. doi: 10.1097/MBC.0b013e32832f2ada [ Links ]
11. Abdalla G, Fawzi Matuk R, Venugopal V, Verde F, Magnuson TH, Schweitzer MA, et al. The diagnostic accuracy of magnetic resonance venography in the detection of deep venous thrombosis: a systematic review and meta-analysis. Clin Radiol. 2015;70(8):858-71. doi: 10.1016/j.crad.2015.04.007 [ Links ]
12. Dessole S, Capobianco G, Arru A, Demurtas P, Ambrosini G. Postpartum ovarian vein thrombosis: an unpredictable event: two case reports and review of the literature. Arch Gynecol Obstet. 2003;267(4):242-6. doi: 10.1007/s00404-002-0318-3 [ Links ]
13. Plastini T, Henry D, Dunleavy K. Ovarian vein thrombus: to treat or not to treat? Blood Adv. 2017;1(15):1120-3. doi: 10.1182/bloodadvances.2017006577 [ Links ]
14. Bannow BTS, Skeith L. Diagnosis and management of postpartum ovarian vein thrombosis. Hematology Am Soc Hematol Educ Program. 2017;2017(1):168-71. doi: 10.1182/asheducation-2017.1.168 [ Links ]
15. Ishaaya E, Tapson VF. Advances in the diagnosis of acute pulmonary embolism. F1000Res. 2020;9:F1000 Faculty Rev- 44. doi: 10.12688/f1000research.21347.1 [ Links ]
Declaration of ethical aspects
Ethical responsibilities: Protection of people. The authors declare that the procedures followed were in accordance with the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Confidentiality of data: The authors declare that we have followed the protocols of the Central Hospital "Dr. Urquinaona" on the publication of patient data.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and / or subjects referred to in the article. This document is in the possession of the corresponding author.
Financing: The authors certify that we have not received financial support, equipment, work personnel or in-kind from people, public and / or private institutions to carry out the study.
Received: August 10, 2020; Accepted: November 15, 2020











 text in
text in 


