Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.2 Lima abr./jun. 2021
http://dx.doi.org/10.31403/rpgo.v67i2329
Case Report
Diagnosis of fetal meconium peritonitis: Case report and review of the literature
1Alberto Sabogal Sologuren National Hospital, Social Health Insurance System - EsSalud, Lima, Peru.
We report the prenatal ultrasonographic diagnosis of a case of meconium peritonitis in a 33-week fetus, who was born preterm and the diagnosis was confirmed with ultrasound, radiography and postnatal surgery. The neonate underwent exploratory laparotomy, in which a meconium pseudocyst was debrided, the perforated intestinal area was resected and end-to-end anastomosis was performed. The initial evolution was torpid, but he was finally discharged with good intestinal function.
Key words: Peritonitis; Meconium; Meconium ileus; Intestinal perforation; Ultrasonography; prenatal; Fetal therapies
Introduction
Meconium peritonitis is an intrauterine process of aseptic inflammation resulting from meconium leakage into the peritoneal cavity of a fetus due to intestinal perforation. Since its first description by Morgagni in 1761, in "De Sedibus et Causis Morborum", meconium peritonitis was considered to have a high mortality rate, reaching 90% in the 1950s. However, in recent years, it has been estimated at 10% in the United States, although it can still be 80% in developing countries1.
We report the case of a fetus with meconium peritonitis secondary to complex ileus, due to the rarity of its occurrence and the fact that prenatal diagnosis can be achieved. An updated review of the subject is made and key data is provided to achieve the ultrasound diagnosis, emphasizing its value in predicting the need for postpartum surgery. It also provides some guidelines on its management.
Case Report
Patient G.D.R., 36 years old, married, from Lima, G2 P0101 and with a history of cesarean section at 33 weeks of gestation due to acute fetal distress, was admitted for uterine contractions to the emergency room of the Alberto Sabogal Sologuren National Hospital, Lima, Peru, on February 20, 2020, at 31 weeks of pregnancy. On ultrasound evaluation, the amniotic fluid index was 40 cm (normal maximum value 25 cm), with a fetal weight of 2,260 g (96% percentile). She was hospitalized for threatened preterm labor. She received tocolysis and fetal lung maturation with dexamethasone. On February 25, percutaneous amnio-drainage was performed without complications (no sample was sent for karyotyping due to the suspension of this type of analysis in the laboratory, because to the COVID-19 pandemic).
Although the admission ultrasonography suspected a liver tumor, the morphological ultrasonography showed mild ascites, peritoneal calcifications, extraluminal meconium delimited by a calcified wall, dilatation of the intestinal loops with echogenic walls, and polyhydramnios. The report concluded: Peritonitis with meconium pseudocyst. Zangheri grade 3 (Figure 1). The sagittal section confirmed its independence from the liver (Figure 2A), and the irrigation of the cystic tumor by branches of the superior mesenteric artery corroborated its intestinal dependence (Figure 2B).

Figure 1 Axial view of the fetal abdomen. ascites (white arrow); peritoneal calcifications (thick light blue arrow); intestinal dilatation with hyperechogenic wall (orange arrow) and meconium pseudocyst with calcified areas on its wall (green arrow) are seen.
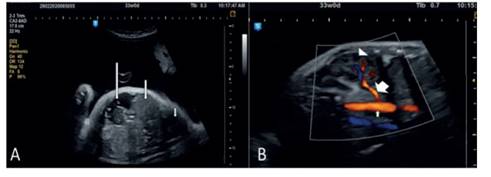
Figure 2 A) Sagittal view with visualization of the thorax (small arrow), liver (medium arrow), and peritoneal pseudocyst (large arrow). b) view of the superior mesenteric artery (large arrow) from its origin in the aorta (small arrow) supplying the area of the peritoneal pseudocyst (arrowhead).
Neurosonography and echocardiography were normal. A TORCH study was performed on maternal blood, the results were negative. On February 29, she presented premature rupture of the membranes, which was managed with observation and antibiotic prophylaxis consisting of ampicillin, amoxicillin, and erythromycin. She went into labor on March 2 and a cesarean section was performed due to dysfunctional labor, resulting in a female newborn of 2,370 g, with Apgar 8/9, regular condition, heart rate 160 beats / minute, 60 breaths / minute; temperature 36.8 ° C, blood pressure of 95/65 mmHg. An orogastric tube was placed (because the abdomen was distended, not very depressible, painful on palpation, with scarce hydroaerial sounds), obtaining a bilious gastric residue. The hemogram showed 11,470 leukocytes (segmented 15.4 %, without band neutrophils). Neonatal ultrasonography showed normal liver, signs of pneumoperitoneum, edema and hyperechogenicity of intestinal loops and free fluid in the cavity. The abdominal X-ray report indicated distension of the loops, veiling in the lower abdomen and presence of calcifications (Figure 3).

Figure 3 neonatal radiography shows distention of the loops, veiling of the lower abdomen and the appearance of soap bubbles (neuhauser sign).
Due to the findings, an exploratory laparotomy was performed, in which a blind tumor was found and debrided, with 30 mL of meconium content, necrotic areas and internal and wall calcifications, adjacent to a 3 cm perforation in the anti-mesenteric border of the distal ileum, located 15 cm from the ileocecal valve. Eight cm of this intestinal region was resected (Figure 4), and a termino-terminal anastomosis was performed.
The patient presented with postoperative ileus; she developed sepsis, received meropenem and vancomycin, and was discharged in satisfactory condition on April 17, 2020.
Discussion
We report the case of a fetus with meconium peritonitis, as part of a complex meconium ileus, diagnosed by ultrasonography in the prenatal stage, which allowed timely clinical management.
Meconium peritonitis is defined as the inflammation of the peritoneum, intestinal loops and mesenteries due to an aseptic chemical reaction, localized or generalized, due to the entry of meconium into the peritoneal cavity of the fetus, as a consequence of intestinal perforation1. It is usually secondary to a complex meconium ileus.
Meconium ileus is a type of intestinal obstruction in the fetus or neonate, produced by the impaction of dense and sticky meconium (produced by abnormal glands that secrete mucus with a very high protein content, with an abnormal mucoprotein, responsible for its thickening), which occludes the intestinal lumen, generally at the level of the terminal ileum. If it only produces obstruction and proximal dilation, it is called simple meconium ileus; the distal intestine contains dry pellets of feces ("rabbit feces"). Complex or complicated ileus is associated with volvulus, atresia or when there is intestinal perforation. If there is perforation, sterile meconium leaks into the fetal peritoneal cavity, producing chemical peritonitis (activated by lipases and bile salts poured into the abdomen).
Meconium peritonitis is fortunately very rare (1/30,000 live births), although this figure may be underestimated due to the spontaneous closure of the perforation before delivery. The evolution of this perforation has three possibilities: 1) spontaneous closure (in these cases, generally, only peritoneal calcifications will be seen on a postnatal radiograph performed for other indications); 2) digestion and reabsorption of the damaged intestinal segment, degenerating into atresia; or, 3) the extravasated meconium agglomerates adjacent to the perforation, thickens further and calcifies in certain areas, being delimited by the omentum, resulting in a cavity with calcified walls and predominantly liquid contents, which is known as meconium pseudocyst (Figure 5)1-4).
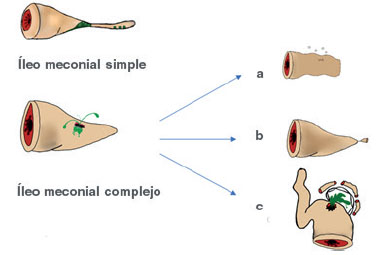
Figure 5 types of meconium ileus. in simple meconium ileus there is only obstruction. in the complex type, there is meconium leakage, which produces meconium peritonitis. it can evolve to spontaneous closure, in which only calcifications are observed in the radiography (a), to an atresia (b), or to the formation of a meconium pseudocyst (c).
Meconium ileus accounts for 9 % to 33 % of all neonatal intestinal obstructions, with an incidence of 1:2,500 live births in Caucasians. It is the third most common cause of neonatal small bowel obstruction, after ileal and duodeno-jejunal atresia and malrotation. It occurs in 10 %-20 % of infants with cystic fibrosis (among Caucasians, 75 % of meconium ileus is associated with cystic fibrosis). It affects both sexes equally, and its association with congenital anomalies is rare3,4).
The main symptoms in the neonate include abdominal distention (96 %), bilious vomiting (50 %), and delayed passage of meconium (36 %)3).
Prenatal diagnosis is of vital importance because, together with neonatal intensive care, it has reduced the mortality rate to less than 10 %. Furthermore, those operated between 36 and 48 hours of life have a mortality rate four times higher than those operated during the first 24 hours; while after 48 hours, mortality rates vary between 80 % and 91 %1).
Therefore, according to the pathophysiology, the ultrasound findings will vary: 1) when it is a simple meconium ileus, we will observe a dilated proximal small bowel and a thinned colon, due to its poor function (Figure 5); 2) peritoneal calcifications (seen as echogenic dots or lines or as calcified masses in the abdomen, fetal pelvis and / or scrotum in male fetuses) should lead us to think of a complex ileus (Figure 1), making the ultrasound diagnosis of atresia or volvulus difficult, however, ascites and meconium pseudocysts can be detected. The latter appear as hypoechoic images of heterogeneous content, delimited by a wall with calcified areas (Figures 1 and 5). Polyhydramnios and intestinal hyperechogenicity are frequently found in both cases3,5).
When calcifications are found, the differential diagnosis includes testicular neoplasms (calcifications in the scrotal sac), teratomas, gonadoblastomas and intra-abdominal neuroblastomas, and intra-abdominal calcifications have also been described in cases of ileal stenosis and total colonic aganglionosis11).
To predict the need for urgent surgery in fetuses with an ultrasound diagnosis of meconium peritonitis, Zangheri created a classification, based on a review of 69 fetuses with this pathology:
Grade 0: isolated intra-abdominal calcifications.
Grade 1: intra-abdominal calcifications and one of the following: ascites, pseudocyst or intestinal dilation.
Grade 2: intra-abdominal calcification and two of the following: ascites, pseudocyst, or intestinal dilation.
Grade 3: all the above.
She observed that, while those with a score of 0 can be delivered at term without any complications, 52 % (13/25) of those fetuses with grade 1, 80 % (16/20) with grade 2 and 100% (6/6) with grade 3 required surgical intervention, respectively (p <0.001)(6). In our case, we found a grade 3 score; once the postnatal examinations were performed, the surgery was scheduled. Therefore, if ultrasound markers are found that indicate the need for postnatal surgery, delivery should take place in a tertiary center7).
These observations have been confirmed in a systematic review with 244 cases, whose meta-analysis shows that the strongest predictor of neonatal surgery was the finding of meconium pseudocyst (OR [95% CI] 6.75 [2.53-18.01]), followed by intestinal dilation (OR [95% CI] 4.17 [1.93-9.05]) and ascites (OR [95% CI] 2.57 [1.07- 5.24]); with small bowel atresia being the most associated with intestinal perforation and meconium peritonitis (52.2 % of cases)8).
However, there are studies that disagree with these findings, such as that of Feng et al.9), in which only polyhydramnios is indicated as a significant predictor of postnatal surgery.
On the other hand, MRI is also a technique that helps in diagnosis. Lu10 published the results of a retrospective cohort of 35 fetuses diagnosed with meconium peritonitis. All fetuses with MRI showing intestinal dilatation (14/26, p = 0.048) and microcolon (13/26, p = 0.013) required surgery. They, surprisingly, found no significant difference with the presence of meconium pseudocysts between the two groups. In this study, although both methods were not directly compared, the arrest of intestinal dilatation and ascites were similar to ultrasonography, with an advantage of MRI for the visualization of the microcolon.
Postnatally, the supine plain abdominal radiograph usually shows numerous air-filled bowel loops without the characteristic hydroaerial levels due to meconium and abnormal mucous gland secretion (although their presence does not exclude it). In some cases, the mixture of meconium and intestinal gas gives the appearance of soap bubbles (Neuhauser's sign) (Figure 3). This is not pathognomonic of meconium ileus and can also be seen in ileal atresia, colonic atresia, Hirschsprung's disease, meconium plug syndrome; it is due to the dense mixture of meconium with air. The presence of calcification, free air, or multiple hydroaerial levels suggests complex ileus. In addition, for differential diagnosis, adrenal and hepatic calcifications can also be identified with cytomegalovirus, parvovirus, or hepatoblastoma3-5).
Regarding management, the ultrasound finding of signs of meconium peritonitis in a fetus is not an indication for immediate delivery (due to the possibility of spontaneous intrauterine closure). However, the suggested optimal time of delivery is 35 weeks, to avoid progression of the disease and to start early treatment1. In the neonatal period, with a stable patient and a suspicion of simple meconium ileus, a nonionic contrast enema examination may be useful to differentiate it from meconium plug syndrome, in which a normal or dilated colon is observed. If a meconium pseudocyst is found, as in this case, surgical management involves debridement of necrotic tissue, excision of the cystic membrane, exploration of the bowel loops from the angle of Treitz to the rectum, to rule out perforations, adhesions, necrotic areas and despulid areas at high risk of perforation. When perforation is evident, resection should be done and, depending on the state of the intestinal loops, end-to-end anastomosis or shunts (preferably ileostomy or Bishop-Koop, Santulli) should be performed. There may be postoperative complications such as ileus, dehiscence of anastomotic, intestinal obstruction due to flanges and adhesions, neonatal sepsis, among others5).
In conclusion, we report a case of meconium peritonitis secondary to complex meconium ileus, diagnosed in the prenatal period, which allowed timely planning and surgical treatment, demonstrating its importance in the first step of perinatal therapy. The timing of delivery and surgical intervention should be discussed with a multidisciplinary team of gynecologists, anesthesiologists, neonatologists and pediatric surgeons, requiring, therefore, to be performed in a tertiary level care center.
Acknowledgments
To Sophye Tipiani Quijano for the design and elaboration of figure 5
REFERENCES
1. Peiró JL. Aydin E. Meconium peritonitis. In: Puri P, editor. Pediatric Surgery. Berlin: Springer-Verlag GmbH Germany; 2020:993-1002. Doi: https://doi.org/10.1007/978-3-662-43588-5_72 [ Links ]
2. Corbett P, Saxena A. Meconium ileus. In: Lima M, Reinberg O, editors. Neonatal Surgery. Switzerland: Springer Nature; 2019:265-77. Doi: https://doi.org/10.1007/978-3-319-93534-8_19 [ Links ]
3. Ciprandi G, Rivosecchi M. Meconium Ileus. In: Puri P, Höllwarth M, editors. Pediatric surgery. 2da edition. Berlín: Taylor & Francys Group; 2019:213-20. Doi: https://doi. org/10.1007/978-3-662-56282-6_27 [ Links ]
4. Al-Salem A. Meconium ileus. In: Springer C, editor. Atlas of Pediatric Surgery. Switzerland: Springer Nature Switzerland AG. 2020:503-14. Doi: https://doi.org/10.1007/978-3-03029211-9_53 [ Links ]
5. Omogiade U. Meconium ileus. In: Shehata S, editor. Pediatric Surgery. London: IntechOpen; 2019:71-84. Doi: http://dx.doi.org/10.5772/intechopen.85548 [ Links ]
6. Zangheri G, Andreani M, Ciriello E, Urban G, Incerti M, Vergani P. Fetal intra-abdominal calcifications from meconium peritonitis: Sonographic predictors of postnatal surgery. Prenatal Diagnosis. 2007;27(10):960-3. Doi: https://doi.org/10.1002/pd.1812 [ Links ]
7. Zerhouni S, Mayer C, Skarsgard E. Can we select fetuses with intra-abdominal calcification for delivery in neonatal surgical centres? J pediatric surg. 2013;48(5):946-50. Doi: https://doi.org/10.1016/j.jpedsurg.2013.02.006 [ Links ]
8. Shinar S, Agrawal S, Ryu M, Mieghem T, Daneman A, Ryan G, et al. Fetal meconium peritonitis prenatal findings and postnatal outcome: a case series, systematic review, and meta-analysis. Ultraschall in Med. 2020 Jun. DOI: https://doi.org/10.1055/a-1194-4363 [ Links ]
9. Feng Y, Zheng H, Zhang G, Zhong W, Guo K, Tang H, et al. Predicting poor outcomes and the need for surgical treatment in neonates with meconium peritonitis. Prenatal Diagnosis. 2020;40:351-7. Doi: https://doi.org/10.1002/pd.5608 [ Links ]
10. Lu Y, Ai B, Zhang W, Liu H. Fetal magnetic resonance imaging contributes to the diagnosis and treatment of meconium peritonitis. BMC Med Imaging. 2020;20(55). DOI: https://doi.org/10.1186/s12880-020-00453-8 [ Links ]
11. Sosa A, Inaudy E. Ultrasonografía y clínica: Embrio-fetal. 2a edición. Valencia, Venezuela: Tatum; 2002:326-7. [ Links ]
Cite as: Tipiani Rodríguez O, Arrunátegui Alejandría RA, Berrocal Anaya WH, Rodríguez Miranda JH, Escalante Jibaja R, Jaramillo Ventura JM, Quiñones Pereyra CF, Del Águila Calderón KP. Prenatal diagnosis of fetal meconium peritonitis: Case report and review of the literature. Rev Peru Gincol Obstet. 2021;67(2). DOI: https://doi.org/10.31403/rpgo.v67i2329
Received: November 04, 2020; Accepted: December 29, 2020











 texto en
texto en 



