Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.2 Lima abr./jun. 2021
http://dx.doi.org/10.31403/rpgo.v67i2331
Case report
Autoimmune polyuria - polydipsia syndrome in the postpartum period in a 27-year-old woman
1. Hospital Nacional Edgardo Rebagliati Martins, Essalud, Lima, Perú
2. Universidad Nacional Mayor de San Marcos, Lima, Perú
Autoimmune hypophysitis is a condition characterized by lymphocytic infiltration of the pituitary resulting in deficiency of one or more hormones of both the adenohypophysis and the neurohypophysis. For diagnosis, a high index of suspicion is necessary, even more so considering the temporal relationship with pregnancy or childbirth. Clinical and imaging features are suggestive of the diagnosis. Although the definitive diagnosis is by biopsy, this is not usually performed because of the potential adverse effects of the procedure. We present a case describing the form of manifestation of the disease and the typical imaging features on magnetic resonance imaging.
Key words: Polyuria; Polydipsia; Diabetes Insipidus; Autoimmune hypophysitis; Postpartum period
Introduction
Polyuria is defined as an abnormally high excretion of dilute urine (more than 3 liters in 24 hours), associated with various pathologies, which in summary are called polyuria-polydipsia syndrome1. Central diabetes insipidus (CID) is caused by a variety of acquired or congenital disorders, the less frequent of inflammatory or autoimmune origin and known by the term hypophysitis, a condition characterized by lymphocytic infiltration of the pituitary gland2. Although its definitive diagnosis is by biopsy, this is not usually performed due to the potential adverse effects; nevertheless, the clinical and imaging characteristics suggest the diagnosis3,4. A case is presented describing the form of occurrence of the disease and the typical features on pituitary magnetic resonance imaging (MRI).
Case report
The patient was a 27-year-old woman, gravida 2 para 1, who had gestational diabetes mellitus in her first pregnancy treated with diet; this pregnancy ended in January 2018 with cesarean section at 32 weeks due to severe oligohydramnios. Since April 2018, she presented with moderate intensity headache and polydipsia (±10 liters of water/day), polyuria (±10 liters/day). She received antibiotic treatment for 7 days for suspected urinary tract infection, without improvement. She was emergency treated in Pisco, Peru, for moderate dehydration, being referred to our hospital in June 2018 for study of polydipsia-polyuria syndrome.
On physical examination, the patient had apparent regular general condition, with signs of dehydration, weight 68 kg, body mass index 29, normal blood pressure, dry mucous membranes. During her stay, polyuria (11 liters/day) was observed. Evaluation of pituitary function confirmed the presence of partial hypopituitarism: thyrotrophin 1.2 IUI/mL, free thyroxine 0.9 ng/dL, negative antithyroid antibodies, prolactin 23.1 ng/mL, luteinizing hormone 15.6 mIU/mL, follicle-stimulating hormone 6.15 mIU/mL, estradiol 299 pg/mL, corticotrophin 24.1 pg/mL, cortisol 8 am 8.9 ug/dL, somatomedin C 64.2 ng/mL, creatinine 0.6 mg/dL, glycemia 84 mg/ dL, serum calcium 9.4 mg/dL and urine calcium 140 mg/dL, serum sodium (Na+) 143 mEq/L.
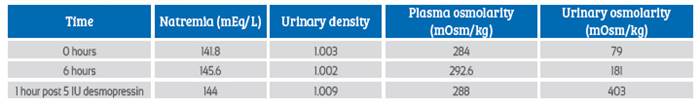
The water restriction test confirmed the presence of central diabetes insipidus. The results are shown in Table 1.
Table 1 Results of the water restriction test, where the increase of more than 50% of the basal urinary osmolarity after administration of desmopressin is verified.
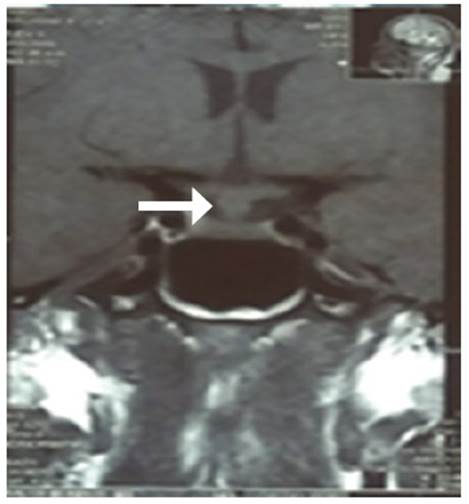
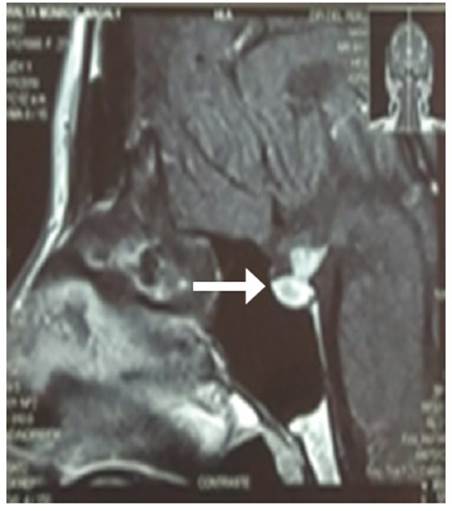
Pituitary MRI showed thickening of the pituitary stalk up to 8 mm (Figure 1), with an increased pituitary volume of 15 x 12 x 7 mm, absence of the brightness corresponding to the neurohypophysis in T1 (Figure 2) and hyper uptake of gadolinium in the infundibulum and the whole pituitary gland (Figure 3).
The multidisciplinary medical board proposed to perform a diagnostic biopsy, which was not accepted by the patient, so methylprednisolone pulses 1 g/day intravenous for 3 days were indicated. Likewise, desmopressin nasal spray 1 puff bid was started, decreasing the urinary volume to 1 500 mL/day, with Na+ control 137 mEq/L.
Discussion
Autoimmune hypophysitis (AIH) is an inflammatory disease affecting the pituitary gland and can be associated with neurological, ophthalmoogical and endocrinological manifestations. The clinical presentation is variable. Symptoms have been classified into four categories: a) compressive (frequency 50 to 70%), b) hypopituitarism (66 to 97%), c) diabetes insipidus (27%), and d) hyperprolactinemia (rare)5.
The association with pregnancy (particularly in the third trimester or early postpartum) pro-vides evidence to support the diagnosis6. In most cases, the clinical history and the characteristics of the pituitary MRI image (thickening of the pituitary stalk, absence of neurohypophysis signal in T1) suggest the diagnosis7, data that were evidenced in the patient.
The diagnosis and management of CDI associated with hypophysitis consists of confirmation of hypotonic polyuria, water restriction test and hormone replacement according to current recommendations8,9. The main goals of treatment are to control hormonal deficiencies and to reduce the pituitary inflammatory process and, consequently, the consequences related to mass effect. The primary treatment of hypophysitis falls into four categories, including surgery, anti-inflammatory medical therapy, conservative treatment and radiotherapy10. There are limited reports of spontaneous resolution of hypophysitis. In cases without significant mass effect or headache, follow-up of hypophysitis may be chosen in addition to replacement of hormone deficiencies11.
Glucocorticoid therapy constitutes the cornerstone of medical treatment, despite its controversial role, with studies in small populations and contradictory results. Good initial response is reported, but with high recurrence rates12. In this case, complementary treatment with methylprednisolone was decided, showing resolution of the symptomatology up to the present. Periodic follow-up with MRI and hormone every 6 months is fundamental in the management of the patient.
Acknowledgments
To the patient for her consent to present her case. And to the colleagues of the hormone laboratory, diagnostic imaging, endocrinology and neurosurgery specialties for their support in the study and management of this patient.
REFERENCES
1. Robertson GL. Antidiuretic hormone. Normal and disordered function. Endocrinol Metab Clin North Am. 2001;30(3):671-vii. doi:10.1016/s0889-8529(05)70207-3 [ Links ]
2. Leporati P, Landek-Salgado MA, Lupi I, Chiovato L, Caturegli P. IgG4-related hypophysitis: a new addition to the hypophysitis spectrum. J Clin Endocrinol Metab. 2011;96(7):1971-80. doi:10.1210/jc.2010-2970 [ Links ]
3. Caturegli P, Newschaffer C, Olivi A, Pomper MG, Burger PC, Rose NR. Autoimmune hypophysitis. Endocr Rev. 2005;26(5):599-614. doi:10.1210/er.2004-0011 [ Links ]
4. Abe T. Lymphocytic infundibulo-neurohypophysitis and infundibulo-panhypophysitis regarded as lymphocytic hypophysitis variant. Brain Tumor Pathol. 2008;25(2):59-66. Doi:10.1007/s10014-008-0234-8 [ Links ]
5. Faje, A. Hypophysitis: Evaluation and management. Clin Diabetes Endocrinol 2016;(2):15. doi: https://doi.org/10.1186/s40842-016-0034-8 [ Links ]
6. Joshi MN, Whitelaw BC, Carroll PV. Mechanisms in Endocrinology. Hypophysitis: diagnosis and treatment. Eur J Endocrinol. 2018;179(3):R151-R163. doi:10.1530/EJE-17-0009 [ Links ]
7. Tartaglione T, Chiloiro S, Laino ME. Neuro-radiological features can predict hypopituitarism in primary autoimmune hypophysitis. Pituitary. 2018;21(4):414-24. doi:10.1007/s11102-018-0892-4 [ Links ]
8. Paz-Ibarra J, Sáenz S, Quintana O. Pruebas diagnósticas en endocrinología. 2017. Editorial Académica Española. ISBN 13: 978-3-639-78336-0. [ Links ]
9. Fleseriu M, Hashim IA, Karavitaki N. Hormonal replacement in hypopituitarism in adults: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101(11):3888-921. doi:10.1210/jc.2016-2118 [ Links ]
10. Sugihara H. Review on recent topics in hypophysitis. J Nippon Med Sch. 2017;84(5):201-8. doi:10.1272/jnms.84.201 [ Links ]
11. Honegger J, Buchfelder M, Schlaffer S. Treatment of primary hypophysitis in Germany. J Clin Endocrinol Metab. 2015;100(9):3460-9. doi:10.1210/jc.2015-2146 [ Links ]
12. Khare S, Jagtap VS, Budyal SR. Primary (autoimmune) hypophysitis: a single centre experience. Pituitary. 2015;18(1):16-22. doi:10.1007/s11102-013-0550-9 [ Links ]
Declaration of ethical aspects
Ethical responsibilities: Protection of persons: The authors declare that the procedures followed conform to the ethical standards of the World Medical Association and the Declaration of Helsinki.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Financing: The authors certify that we have not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the study.
Received: March 08, 2020; Accepted: December 10, 2020











 texto en
texto en