Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.4 Lima Oct./Dec. 2021
http://dx.doi.org/10.31403/rpgo.v67i2368
Systematic Review
Micronutrient intake during pregnancy and lactation
1. Faculty of Medicine, La Universidad del Zulia, Maracaibo, Zulia, Venezuela
2. Obstetrics and Gynecology Service, Hospital Central "Dr. Urquinaona, Maracaibo, Zulia, Venezuela
Adequate nutritional status of women before, during and after pregnancy is essential to avoid obstetric and perinatal complications. Micronutrients are essential for maternal and fetal development. Pregnancy has a special metabolic demand for high quality nutrients. In addition, adequate micronutrient intake can directly improve the quality of breast milk. Supplements can meet the increased demand for these elements during pregnancy and lactation, reducing the risk of fetal congenital anomalies, obstetric pathologies and development of chronic diseases in adulthood. However, there is conflicting information on the efficacy and safety of nutritional supplements during pregnancy. It is important that medical personnel can provide accurate and appropriate evidence-based advice on supplementation during pregnancy, as not all pregnant women need to use supplements on a regular basis, but it is necessary to identify pregnant women at risk for deficiency. The objective of this review was to analyze the effects of micronutrient intake in pregnancy and lactation.
Key words: Vitamins; Minerals; Micronutrients; Pregnancy; Lactation
Introduction
Pregnancy changes the nutrient and food requirements consumed by the mother, which has potential health impacts. Any nutritional alteration can negatively affect fetal growth, leading to pathologies such as placental insufficiency, preterm delivery and fetal malformations. Therefore, the diet of the pregnant woman should be balanced and varied, with individualized supplementation of micronutrients at optimal doses to achieve maternal health and proper fetal growth1,2. Not only should energy needs be met during pregnancy, but also energy reserves should be created to be used during lactation3.
In previous decades there have been no unified guidelines on nutrient intake during pregnancy. The insufficient number of experimental studies due to ethical controversies contributed to this fact4. There are myths about the nutrition of pregnant women that circulate in social settings, regardless of socioeconomic and educational level5,6.
The energy demand of pregnant women changes in relation to the preconception period. The increase in body weight (fetal, placental and maternal development) is accompanied by an increase in basal metabolism3,7. The energy demand for each trimester of pregnancy is shown in Table 1. The additional energy expenditure during the first trimester is negligible. During the second trimester, energy demand is associated with the growth of maternal tissues (plasma volume, increased volume of reproductive organs and mammary glands, accumulation of adipose tissue) and in the third trimester it is marked by fetal development8-10. The World Health Organization estimated that the additional energy expenditure during the second and third trimester of pregnancy would be around 300 kcal/day3.
Table 1 energy demand of pregnanT women.
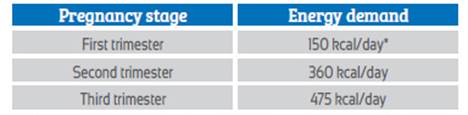
* If the pregnant woman is underweight (body mass index < 18.5 kg/m2), it is necessary to increase energy intake during the first trimester of pregnancy.
Nutritional deficiencies, even in pregnant women with adequate and varied diets, can appear selectively, due to low dietary protein content and individual capacity for absorption and metabolism of nutrients. The main deficiencies that may appear are: vitamins (folic acid, vitamin D, vitamin A and E), minerals (iron and iodine), macroelements (magnesium and calcium) and polyunsaturated fatty acids4,9. Nutritional studies have shown that the diet of pregnant women generally lacks sufficient amounts of folic acid, polyunsaturated fatty acids, iron, iodine, vitamin D and other minerals - vitamins essential for maternal health and fetal development11,12. The objective of this review was to analyze the effects of micronutrient intake in pregnancy and lactation.
Methodology of the InforMatIon search
Between July and December 2020, electronic databases of biomedical scientific literature (UpToDATE, OVIDSP, ScienceDirect, SciELO and PUBMED) were examined to investigate eligible articles in the last 21 years (2000 - 2021). The indexes of the main world and national journals were also searched. The search terms used in the databases were: "Consumption", "Vitamins", "Micronutrients", "Minerals", "Pregnancy" and "Lactation", in English and Spanish, and human studies. From a total of 35 published articles, 5 were eliminated as duplicates. Of the remaining 30, 2 were subsequently excluded for providing insufficient data. This review included the most relevant current contributions on the effects of vitamin and mineral intake during pregnancy and lactation.
Vitamin and mineral intake in pregnant women
The consumption of micronutrients increases the possibility of good obstetric outcome and reduction of the risk of complications13-16. Nutritional studies show that about a quarter of pregnant women admit to using different supplements during pregnancy, despite the lack of medical recommendations for their consumption11. Multivitamin supplements are widely available and can be purchased without prescription in commercial establishments, in the belief that they are harmless. Uncontrolled consumption of multi-ingredient preparations - beyond the period appropriate to clinical needs - is associated with risk of overdose and interactions with other prescribed drugs12. For this reason, it is advisable to consult the attending physician before starting their consumption, since it is necessary to consider the characteristics of the diet, dietary habits and individual nutrient needs of the pregnant woman (for example, chronic diseases). The greatest risk of adverse effects is associated with excessive consumption of vitamin A, beta-carotene, calcium, copper, fluoride, iron and zinc11.
Iron
It is an essential micronutrient in the process of tissue respiration, hemoglobin formation, DNA synthesis and regulation of the immune system. It also improves liver metabolism and regulates cholesterol concentration. Iron deficiency in pregnant women is common, mainly due to low dietary content of easily digestible iron and malabsorption. This deficiency leads to iron deficiency anemia, immune disorders, mental and cardiac pathologies. Anemia during pregnancy increases the risk of preterm delivery and low birth weight3.
The richest food sources of iron include: red meat (especially liver), legume seeds, eggs, pumpkin and sunflower seeds, dried apricots, 2 Rev Peru spinach and kale. Heme iron in animal products is better absorbed than non-heme iron found in plant foods. Coadministration of vitamin C and the acid pH of the gastrointestinal tract facilitate absorption, while foods rich in phytates (cereals and legumes), tannins (tea, coffee and herbal infusions) and dietary fiber hinder its uptake3.
The recommended doses are 27 mg/day during pregnancy and 20 mg/day during lactation, which should be increased in cases of gastrointestinal diseases or in women with vegan and vegetarian di-ets1. So far, there are no reports of food poisoning. Symptoms of supplement overdose include nausea, diarrhea, vomiting, central nervous system, kidney, liver and cardiovascular system disorders.
In pregnant women with known anemia (hemoglobin concentrations less than 11 mg/dL) it is necessary to start supplementation with oral iron preparations at doses of 30 mg/day, increasing to 60 and 120 mg/day, after the eighth week of pregnancy. Iron salts have good clinical effects when used as oral extended-release tablets. In addition, they have fewer gastrointestinal side effects, high bioavailability of elemental iron, and greater acceptance of treatment by women17. Pregnant women at risk of developing anemia should initiate supplementation at dos-es of 20 mg/day prior to conception.
Folic acid
It is present in foods in 150 different forms of folate (folic acid salts). It is responsible for the regulation of cell growth and division, especially in the digestive, nervous and hematopoietic systems. Its absorption occurs in the small intestine and it subsequently binds to plasma proteins and is converted into a coenzyme involved in the synthesis of nucleic acids. Folic acid from supplements and drugs is a stable synthetic form that must be reduced to tetrahydrofolate in cells in order to be biologically active18.
Folic acid is essential in the preconception period, during pregnancy and lactation. It is associated with a decreased risk of neural tube defects, fetal congenital heart and urinary disorders. It also reduces the risk of miscarriage and maternal thrombosis. Supplementation during the second and third trimester of pregnancy prevents megaloblastic anemia secondary to vitamin B12 and folate deficiency18.
The recommended dose of folic acid is 0.4 mg/day and its consumption should be initiated 6 weeks before conception11. In case of a history of nervous system defects in previous pregnancies, megaloblastic anemia, hyperhomocysteinemia, use of drugs that reduce folic acid absorption (for example, oral contraceptives and antiepileptic drugs), obesity, history of smoking or alcohol consumption, the dose can be increased to 5 mg/day1. Co-administration with other vitamins (B6 and B12) and vitamin C facilitates its absorption. Overdose, although rare, can be harmful during early pregnancy and in-creases the risk of obstetric complications11.
Approximately 50% of the female population may present alterations in the activity of the enzyme methyltetrahydrofolate reductase, which limit the absorption of folic acid, despite its adequate supply. These women, in addition to the daily dose, need simultaneous supplementation of active forms of folate in the form of calcium salt15,19.
Calcium
It is the basic component of teeth and bones. It participates in neuromuscular conduction, blood coagulation, regulation of cardiac function and blood vessels. Together with magnesium, it is responsible for blood pressure control. Calcium from vegetable products is much less absorbed due to the simultaneous presence of phytates and oxalates, but simultaneous supplementation with vitamin D and consumption of lactose increases bioavailability and facilitates its absorption4.
Calcium deficiency increases nervous excitability and the risk of coagulation disorders and may lead to arterial hypertension. Chronic deficiencies lead to childhood rickets and osteomalacia, along with increased risk of osteoporosis in adulthood. Hypercalcemia may be associated with elevated vitamin D concentrations and high calcium supplements. The richest food sources of calcium are milk, cheese, yogurt, fish from which the bones can be eaten (sardines, ancho vies) and shellfish (shrimps, prawns)20. To date, there are no reports of cases of hypercalcemia with an adequate diet.
Daily requirements vary between 800 and 1,000 mg/day in women older than 19 years and 1,100 to 1,300 mg/day in women younger than 19 years; in case of insufficient dietary calcium intake, requirements may increase up to 1,200 mg/day. However, supplementation up to 1,000 mg/day is possible, depending on the individual needs of each case20.
There is insufficient evidence of the effectiveness of food fortification or calcium supplementation during preconception or early pregnancy for the prevention of maternal and perinatal complications. Although published studies have shown some beneficial effects, they present methodological deficiencies (small sample groups and co-administration of other supplements and antioxidants)21.
Vitamin D
It regulates plasma calcium and phosphate concentrations, affects maternal-fetal bone mineralization, modulates the functions of the hematopoietic and immune systems, facilitating adaptation for the maintenance of pregnancy6. In addition, it has antiproliferative properties, so it may be useful in the prevention of gastrointestinal and breast cancer. It also has beneficial effects in decreasing the risk of conditions such as preeclampsia, gestational diabetes, bacterial vaginosis, autoimmune diseases and cardiovascular diseases22,23.
80% of vitamin D comes from cutaneous synthesis after exposure to sunlight and the remaining 20% is absorbed through the gastrointestinal tract. In countries with four distinct seasons, effective synthesis is only possible in the months with the most sunlight (part of spring, autumn and throughout the summer). To achieve optimal concentrations, exposure time to sunlight should be longer than 30 minutes, without the use of protective creams with ultraviolet filters, and 20% of the body surface should be exposed to light (e.g., face and forearms). Deficiency leads to alterations in bone mineralization (osteopenia or osteoporosis), immune disorders and increased risk of neonatal and infant pathologies such as symptomatic fetal rickets, low birth weight and height and reduced physical and mental development during the first year of life22. The recommended dose is 2,000 IU/day during the preconception period, pregnancy and lactation1.
Omega-3 polyunsaturated fatty acids
Polyunsaturated fatty acids are basic components of the double lipid cell membrane. They have fundamental functions in the transmission of electrical impulses in peripheral nerves and the retina. In addition, they regulate low-density lipoprotein and triglyceride concentrations, reducing the risk of atherosclerosis and hypertension24.
Among the omega-3 polyunsaturated fatty acids, docosahexaenoic acid is the most important for pregnancy and lactation. Different studies have shown that they have beneficial effects on the resulting obstetric-perinatal outcome: increased newborn weight (without increasing the risk of macrosomia), reduced risk of preterm birth and correct psychomotor devel opment of children in the first years of life25. Adequate intake in the maternal diet reduces the risk of alterations in oxidative stress and in flammatory markers26.
Foods rich in polyunsaturated fatty acids are fish and other seafood (tuna, herring, and sardines), nuts and seeds (flaxseed and chia) and plant oils (flaxseed, and soybean). The recommended dose is 600 mg/day (preferably before 20 weeks of pregnancy and during lactation). In case of in sufficient intake from natural sources, diet low in unsaturated fatty acids or high risk of preterm delivery, it can be increased to 1,000 mg/day1. To date, there are no reports of symptomatology related to omega-3 fatty acid overdose.
Iodine
It is an essential element for the functioning of the thyroid gland. Thyroxine and triiodothyronine regulate the development and functioning of the nervous, muscular, cardiac and renal systems. Insufficient iodine intake by pregnant women can lead to the development of maternal goiter and mental retardation in the newborn4,14. In pregnant women with hypothyroidism, there is an increased risk of spontaneous abortion, intrauterine fetal death, preterm delivery and infant hypothyroidism27. Requirements during pregnancy are 160 μg/day and during lactation 210 μg/day11.
Magnesium
It is an important intracellular macroelement since, together with potassium, it is necessary for the function of more than 300 enzymes. It is involved in protein synthesis, conduction of neuromuscular stimuli, thermoregulation, blood pressure control and bone mineral homeostasis3. Deficiency causes apathy, weakness and depression. In pregnant women, it may manifest with muscle cramps, an indication for supplementation28. Dietary sources rich in magnesium are cereals, legumes, nuts, cocoa, fish and potatoes.
Daily requirements vary from 300 mg/day (pregnancy) and 265 mg/day (lactation) in women older than 19 years to 335 mg/day (pregnancy) and 300 mg/day (lactation) in women younger than 19 years. However, it can be supplemented up to 1,000 mg/day depending on the individual needs of each case3.
Vitamin E
It is a powerful antioxidant that protects against oxidative stress and cell membrane damage. Its properties lead to the strengthening of blood vessels, it intervenes in the synthesis of coagulation factors and decreases platelet aggregation. It also regulates the function of musculoskeletal tissue. Its main deposition sites are adipose tissue and adrenal glands4,29.
Vitamin E is most commonly present in products of vegetable origin (vegetable oils, olives, nuts, almonds, sunflower, pumpkin, sesame seeds and legumes). The requirement of pregnant women is 10 to 19 mg/day29. The symptomatology of excess concentrations consists of fatigue, muscle weakness and impaired mental abilities. Deficiency is rare and supplementation is indicated in cases of gastrointestinal tract diseases and diets poor in polyunsaturated fatty acids4.
Vitamin A
It is a substance with anti-inflammatory, antioxidant and antiproliferative properties that is stored in adipose tissue. It contributes to the regulation of the reception of light stimuli in the retina, responsible for the integrity of cell membranes and the biosynthesis of melanin - collagen, affecting the condition of skin, hair and nails. Its anti-inflammatory and antiproliferative effects contribute to the prevention of colon, breast, prostate and lung cancer30.
Vitamin A (retinol) deficiency is rare and its manifestations are blurred vision, dry skin, brittle hair and nails. Excess is toxic and can cause fetal birth defects (neurological and cardiovascular disorders). The richest food sources include fish oil, liver, milk, dairy products, egg yolk. The requirement for pregnant women is 770 µg/day and should be supplemented only in very specific cases of digestive tract diseases, immunodeficiency, chronic stress or fat-deficient diet30.
Conclusions
Adequate micronutrient intake in pregnant women should be based on individual characteristics, as it does not replace the effects of a varied and balanced diet. An inadequate diet can negatively affect the maternal-perinatal outcome. Specific supplementation for each deficiency should be initiated in the preconception period to reduce the risk of obstetric complications and perinatal anomalies.
REFERENCES
1. Jouanne M, Oddoux S, Noël A, Voisin-Chiret AS. Nutrient requirements during pregnancy and lactation. Nutrients. 2021;13(2):692. doi: 10.3390/nu13020692 [ Links ]
2. Persson PB, Persson AB. Foetal programming. Acta Physiol (Oxf). 2019;227(4):e13403. doi: 10.1111/apha.13403 [ Links ]
3. Simeoni U, Armengaud JB, Siddeek B, Tolsa JF. Perinatal origins of adult disease. Neonatology. 2018;113(4):393-9. doi: 10.1159/000487618 [ Links ]
4. Kot K, Kosik-Bogacka D, Lanocha-Arendarczyk N, Malinowski W, Szymanski S, Mularczyk M, et al. Interactions between 14 elements in the human placenta, fetal membrane and umbilical cord. Int J Environ Res Public Health. 2019;16(9):1615. doi: 10.3390/ijerph16091615 [ Links ]
5. Grieger JA, Hutchesson MJ, Cooray SD, Bahri Khomami M, Zaman S, Segan L, et al. A review of maternal overweight and obesity and its impact on cardiometabolic outcomes during pregnancy and postpartum. Ther Adv Reprod Health. 2021;15:2633494120986544. doi: 10.1177/2633494120986544 [ Links ]
6. Parisi F, di Bartolo I, Savasi VM, Cetin I. Micronutrient supplementation in pregnancy: Who, what and how much? Obstet Med. 2019;12(1):5-13. doi: 10.1177/1753495X18769213 [ Links ]
7. Wendolowicz A, Stefanska E, Ostrowska L. Influence of selected dietary components on the functioning of the human nervous system. Rocz Panstw Zakl Hig. 2018;69(1):15-21. [ Links ]
8. Brown HL, Smith GN. Pregnancy complications, cardiovascular risk factors, and future heart disease. Obstet Gynecol Clin North Am. 2020;47(3):487-95. doi: 10.1016/j.ogc.2020.04.009 [ Links ]
9. Jun S, Gahche JJ, Potischman N, Dwyer JT, Guenther PM, Sauder KA, et al. Dietary supplement use and its micronutrient contribution during pregnancy and lactation in the United States. Obstet Gynecol. 2020;135(3):623-33. doi: 10.1097/AOG.0000000000003657 [ Links ]
10. Lackovic M, Filimonovic D, Mihajlovic S, Milicic B, Filipovic I, Rovcanin M, et al. The influence of increased prepregnancy body mass index and excessive gestational weight gain on pregnancy course and fetal and maternal perinatal outcomes. Healthcare (Basel). 2020;8(4):362. doi: 10.3390/healthcare8040362 [ Links ]
11. Bailey RL, Pac SG, Fulgoni VL, Reidy KC, Catalano PM. Estimation of total usual dietary intakes of pregnant women in the United States. JAMA Netw Open. 2019;2(6):e195967. doi: 10.1001/jamanetworkopen.2019.5967 [ Links ]
12. Diab L, Krebs NF. Vitamin excess and deficiency. Pediatr Rev. 2018 Apr;39(4):161-79. doi: 10.1542/pir.2016-0068 [ Links ]
13. Kinshella MW, Omar S, Scherbinsky K, Vidler M, Magee LA, von Dadelszen P, et al. Effects of maternal nutritional supplements and dietary interventions on placental complications: An umbrella review, meta-analysis and evidence map. Nutrients. 2021;13(2):472. doi: 10.3390/nu13020472 [ Links ]
14. Ramakrishnan U, Grant FK, Goldenberg T, Bui V, Imdad A, Bhutta ZA. Effect of multiple micronutrient supplementation on pregnancy and infant outcomes: a systematic review. Paediatr Perinat Epidemiol. 2012;26 Suppl 1:153-67. doi: 10.1111/j.1365-3016.2012.01276.x [ Links ]
15. Zhang Y, Zhou H, Perkins A, Wang Y, Sun J. Maternal dietary nutrient intake and its association with preterm birth: A case-control study in Beijing, China. Nutrients. 2017;9(3):221. doi: 10.3390/nu9030221 [ Links ]
16. Moreno-Fernandez J, Ochoa JJ, Lopez-Frias M, Diaz-Castro J. Impact of early nutrition, physical activity and sleep on the fetal programming of disease in the pregnancy: A narrative review. Nutrients. 2020;12(12):3900. doi: 10.3390/nu12123900 [ Links ]
17. Garzon S, Cacciato PM, Certelli C, Salvaggio C, Magliarditi M, Rizzo G. Iron deficiency anemia in pregnancy: novel approaches for an old problem. Oman Med J. 2020;35(5):e166. doi: 10.5001/omj.2020.108 [ Links ]
18. Heseker H. Folic acid and other potential measures in the prevention of neural tube defects. Ann Nutr Metab. 2011;59(1):41-5. doi: 10.1159/000332126 [ Links ]
19. Li WX, Dai SX, Zheng JJ, Liu JQ, Huang JF. Homocysteine metabolism gene polymorphisms (MTHFR C677T, MTHFR A1298C, MTR A2756G and MTRR A66G) jointly elevate the risk of folate deficiency. Nutrients. 2015;7(8):6670-87. doi: 10.3390/nu7085303 [ Links ]
20. Singh RB, Mishra S, Kumar S, Tiwari AM, De Meester F, Goyal RK, Kartikey K, Singh M. Micronutrient formulations for prevention of complications of pregnancy. Front Biosci (Schol Ed). 2018;10:175-84. doi: 10.2741/s507 [ Links ]
21. Hofmeyr GJ, Manyame S. Calcium supplementation commencing before or early in pregnancy, or food fortification with calcium, for preventing hypertensive disorders of pregnancy. Cochrane Database Syst Rev. 2017;9(9):CD011192. doi: 10.1002/14651858.CD011192.pub2 [ Links ]
22. Palacios C, Kostiuk LK, Peña-Rosas JP. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst Rev. 2019;7(7):CD008873. doi: 10.1002/14651858.CD008873.pub4 [ Links ]
23. Ramasamy I. Vitamin D Metabolism and guidelines for vitamin D supplementation. Clin Biochem Rev. 2020;41(3):103- 26. doi: 10.33176/AACB-20-00006 [ Links ]
24. Harris MA, Reece MS, McGregor JA, Wilson JW, Burke SM, Wheeler M, et al. The Effect of Omega-3 docosahexaenoic acid supplementation on gestational length: randomized trial of supplementation compared to nutrition education for increasing n-3 intake from foods. Biomed Res Int. 2015;2015:123078. doi: 10.1155/2015/123078 [ Links ]
25. Makrides M. ω-3 fatty acids in pregnancy: Time for action. J Nutr. 2019;149(4):549-50. doi: 10.1093/jn/nxy309 [ Links ]
26. Sley EG, Rosen EM, van't Erve TJ, Sathyanarayana S, Barrett ES, Nguyen RHN, et al. Omega-3 fatty acid supplement use and oxidative stress levels in pregnancy. PLoS One. 2020;15(10):e0240244. doi: 10.1371/journal.pone.0240244 [ Links ]
27. Henjum S, Aakre I, Lilleengen AM, Garnweidner-Holme L, Borthne S, Pajalic Z, et al. Suboptimal iodine status among pregnant women in the Oslo Area, Norway. Nutrients. 2018;10(3):280. doi: 10.3390/nu10030280 [ Links ]
28. Makrides M, Crosby DD, Bain E, Crowther CA. Magnesium supplementation in pregnancy. Cochrane Database Syst Rev. 2014;2014(4):CD000937. doi: 10.1002/14651858.CD000937.pub2 [ Links ]
29. Azzi A. Many tocopherols, one vitamin E. Mol Aspects Med. 2018;61:92-103. doi: 10.1016/j.mam.2017.06.004 [ Links ]
30. Gannon BM, Jones C, Mehta S. Vitamin A requirements in pregnancy and lactation. Curr Dev Nutr. 2020;4(10):nzaa142. doi: 10.1093/cdn/nzaa142 [ Links ]
Ethical responsibilities: Protection of persons. The authors declare that the procedures followed conformed to the ethical standards of the committee on responsible human experimentation and in accordance with the World Medical Association and the Helsinki Declaration of 1975 in its most current version
Funding: The authors certify that we have not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the realization of the study
Right of article publication: The authors declare that the publication rights of the manuscript will be assigned exclusively to the journal in case of publication. We also authorize the electronic dissemination of the article
Received: March 18, 2021; Accepted: June 11, 2021











 text in
text in 



