Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.4 Lima oct./dic 2021
http://dx.doi.org/10.31403/rpgo.v67i2369
Short Communication
Male breast cancer in a Hispanic population sample. Descriptive study
1. Mastologist Clínica Medellín. Master of Sciences Epidemiology and Public Health Valencia International University. IDC Cancer Research Group. UniRemington Biomedical Research Group, Medellin, Colombia.
Introduction:
Breast cancer in men is a rare disease, accounting for only 0.2 - 1.5% of all malignant tumors in men.
Objective
: To describe the sociodemographic data, clinical and paraclinical manifestations, treatment, and recurrence in a sample of patients diagnosed with male breast cancer at a private institution.
Methods
: Descriptive, retrospective study of an institutional database, in the period 1 January 2017 to 31 December 2020. Demographic, clinical and paraclinical data were collected from the medical records and analyzed using descriptive statistics.
Results
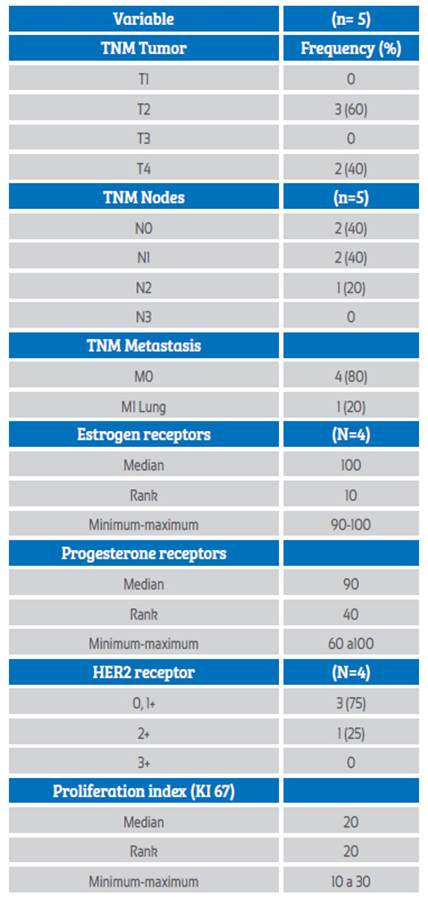
: The prevalence of breast cancer in men in the sample was 0.44%, median age 73 years. The most frequent symptom was breast mass (n = 5; 100%), median tumor size 2.5 cm (range 1.6 to 5 cm) and ductal histological type (n = 5; 100%). All 5 cases had hormone receptor expression, without HER2 overexpression; stage was locally advanced in 60% (n = 3) (stage IIB-IIIA / B) and metastatic in one case. Mastectomy was performed in 80% of cases (n = 4). The median follow-up was 23 months and relapse was found in 20% (n = 1), with an average time to relapse of 184 months.
Conclusions
: In the sample studied, breast cancer in men presented in the seventh decade of life as advanced stage mass, with high hormonal sensitivity. Mastectomy was the main treatment, and most required chemotherapy.
Key words: Breast neoplasms; male; Carcinoma; Mammography
Introduction
Breast cancer in men is a rare disease, with a very low proportion, between 0.2 and 1.5% of all malignant tumors in men, and is responsible for 0.1% of deaths1. In Colombia, the annual incidence is estimated at 0.1 cases per 100,0002. The series reviewed show a prevalence of breast cancer in men of 0.2%3.
The risk factors most implicated in male breast cancer are elevated estradiol levels due to testicular abnormalities and genetic alterations such as mutation of the BRCA 1-2 gene or aneuploidies such as Klinefelter syndrome4. Other factors described include alcoholism, liver disease, obesity and estrogen exposure. However, the relationship is inconsistent, although it may be cumulative5. Among all the proposed factors, the only ones with a proven association are genetic. It is estimated that 15-20% of men with breast cancer have a family history of breast or ovarian cancer, and 10% of all tumors have a genetic predisposition6.
The BRCA2 mutation in men is more prevalent (4 to 40%) than the BRCA1 mutation (0 to 4%). Men who inherit the BRCA2 mutation have a cumulative risk of 6.8% of presenting this type of cancer at the age of 70 years, in contrast to those with the BRCA1 mutation, in whom the risk is less than 1.2%. This risk is 80-100 times higher than in the general population7.
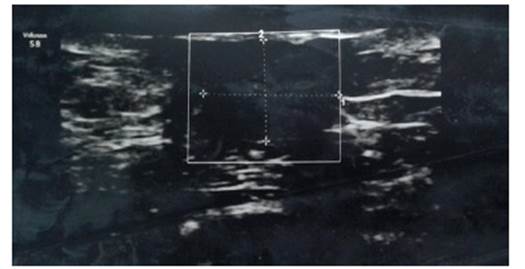
The clinical diagnosis is made when a mammary nodule is found, being subareolar in 70-90% of cases (Figure 1). The average diameter of the mass can range from 0.5-12 cm (mean: 3-3.5 cm). Other clinical signs include nipple retraction (738%), skin ulceration (14-22%) and telorrhage (415%)8 (Figure 2). In many cases there is a delay in diagnosis, due to the lack of knowledge that this disease can affect men; therefore, it is most frequently found in locally advanced stages9,10.
Author source
Figure 1 Ultrasound of male breast, showing retroareolar circumscribed hypoechoic nodule.
The objective of this study was to make a retrospective review of the clinical aspects, diagnosis and treatment of patients who attended the mastology consultation in an oncology unit in the city of Medellin (Colombia).
Methods
This is a retrospective descriptive study of users attended in the mastology consultation at the Medellín clinic (Colombia) by a surgeon, in the period January 1, 2017 and December 31, 2020.
From a total of 1 124 users attended, medical records were searched with ICD code 10 (C509) Malignant tumor of the breast, unspecified part and male sex. Five records were identified, creating an independent database for this cohort of patients. No cases were excluded, as all met the diagnostic criteria, and analysis of the subgroup of 5 cases with a diagnosis of breast carcinoma in men was performed, obtaining demographic data and clinical and pathological characteristics. Data on age, reason for consultation, physical examination, affected side, ultrasound and mammography findings, types of treatment, follow-up and recurrence were included. The exclusive diagnostic criterion was the histopathological study by sharp needle biopsy or study of the surgical specimen.
Descriptive analysis of sociodemographic and clinical variables was performed. Absolute frequencies and percentages, median and ranges were calculated, according to the nature and nonparametric distribution of the variables. The normal distribution was validated using the Shapiro Wilk goodness-of-fit test. SPSS statistics software version 23 was used.
Regarding ethical aspects, the present study is considered a risk-free study, according to the classification established in Article 11 of Resolution No. 008430 of 1993 (issued by the Colombian Ministry of Health) and complies with international standards, the Helsinki declaration, and the ethical guidelines for biomedical research prepared by the Council for International Organizations of Medical Sciences -CIOMS-. This work was approved by the Research Ethics Committee of Clínica Medellín.
Results
Medical records on the experience of a surgeon with male breast cancer at Clínica Medellín from 01/09/2016 to 31/12/2020 were reviewed. A total of 1 124 patients had diagnosis of breast cancer ICD10 code (c509). Filter of ICD10 and male sex was performed, finding 5 patients who met the inclusion criteria, with a prevalence of 0.44%, one of them with bilateral breast cancer.
The median age was 73 years (RIC 17.2). Regarding family history of cancer, one patient had a history in third degree of consanguinity, and in no case was there a report of genetic studies, having been requested in 3 cases. Regarding laterality, 3 cases (60%) were in the right breast, 1 in the left breast (20%), and 1 bilateral (20%). In 60% of the cases (n= 3), the location was retroareolar and in 40% (n= 2) in the upper external quadrant, in all cases as a single lesion (unifocal).
The clinical and histopathological features are presented in Table 1. There were delays in seeking medical attention (patient time), and the time to diagnosis was up to 165 days, while the time to treatment varied ranged from 23 to 60 days.
The main symptom manifested by the 5 patients was the presence of mass. The histologic type in all cases was infiltrating ductal; histologic grade 1 occurred in one case (20%), grade 2 in 3 cases (60 %) and grade 3 in one case (20%). Tumor size averaged 2.5 cm (± 3.4 cm). The most common clinical lymph node stage in the axilla was N1-0 followed by N2; most cases (n: 4; 80%) were in a locally advanced clinical stage: 2 cases at stage IIIB, one bilateral case IIIC- IIB and one patient stage IV due to pulmonary involvement.
The most frequent ultrasound finding was a spiculated nodule in 2 cases (40%), a lobulated nodule in 2 cases and a rounded nodule in 1 case (20%). Mammography was performed in only one case (20%); there were no associated microcalcifications.
Histopathological diagnosis was made by ultrasound-guided cutting biopsy (80%), in one case by excisional biopsy (20%). All patients had an infiltrative component. Regarding hormone receptors, all 5 cases (100%) were positive. HER2 evaluation by immunohistochemistry, in 3 cases was negative and in one case indeterminate, where FISH was negative.
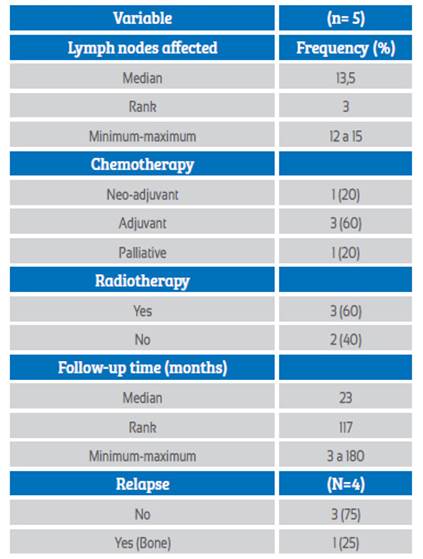
Table 2 summarizes the treatment and follow-up. In the neoadjuvant setting, chemotherapy was used in one patient, and another patient in metastatic stage had palliative treatment, in all cases with doxorubicin, cyclophosphamide, paclitaxel (AC-T). Three patients received adjuvant radiotherapy (60%). The percentage of patients who underwent surgery was 80% (n= 4), the surgical technique used in all cases was total mastectomy. Axillary emptying was performed in 3 cases, and sentinel lymph node biopsy was performed in one patient. Positive margins in 2 cases (50%) required margin enlargement, being finally negative.
The median follow-up of the patients was 23 months. At the end of the follow-up period, 3 (60%) patients were alive, 2 (40%) died of cancer. One patient presented locoregional relapse, receiving management with chemotherapy and hormone therapy.
Discussion
Breast cancer is the most common cancer in women in the world, while in men it is considered a rare disease, and few studies address this disease. Traditionally it has been approached analogously to women, however it presents clinical and immuno-phenotypic differences11.
This study found a prevalence of 0.4% of men with breast cancer among the cohort of women with the same diagnosis, and an annual incidence of 1.25 men with the diagnosis per year. Similar findings have been found in the worldliterature, which reports a prevalence between 0.2-1.5%1, In the Latin American literature there are some case reports, and among the descriptive studies, prevalences have been found to be between 0.2-0.8%12-14, with an incidence of 1.8 men per year15. Additionally, a case of bilateral cancer was found.
Some studies have shown that there are significant differences between both sexes. A study of 459,846 women and 2,665 men diagnosed with breast cancer showed that the average age at diagnosis in women was 61.7, while in men it was 69.616, similar to what was found in the present study where the median age was 73 years.
The risk factor for male breast cancer with proven association are genetic, the diagnosis merits the request of BRCA 1-2 gene study, and between 15% to 20% of those affected have a family history of breast and ovarian cancer17; in this study 20% (n = 1) had a family history of breast cancer.
The study found that 80% (n=4) of the cases were diagnosed at a locally advanced and metastatic stage, which is higher than reported in the North American literature18, but similar to what was found in Latin America, up to 89%15. A possible hypothesis is that the diagnosis is made late18. In the present study, delays were found in patient time, the period between the onset of the symptom and the first consultation, and the time to diagnosis when the histologic diagnosis is obtained.
In this study, the histologic type in the series was ductal, all were hormone receptor positive and none had HER2 overexpression. Other studies have also found that luminal intrinsic luminal intrinsic subtypes A and B are more frequent, and in smaller proportion HER2-positive and basal-like tumors, suggesting a better prognosis19,20. In all cases (100%) they received adjuvant hormonal treatment, similar to that reported by Giordano et al.21, who describe that 80% of cases with estrogen receptor expression received adjuvant tamoxifen. The current recommendation for adjuvant hormonal therapy is tamoxifen in all hormone receptor-positive patients17.
Regarding surgical treatment, in this study all patients with non-metastatic tumors were treated with mastectomy, and in one case sentinel node biopsy was performed. In other Latin American studies, such as that of Ibañez et al.14 and Angel et al.15, mastectomy was performed in 100% of patients, with no cases of conservative surgery.
Regarding the management of the axilla, there are only retrospective series on the use of sentinel nodes in men. These have shown adequate diagnostic performance, and additionally the same benefits by avoiding the morbidity of mandatory lymph node dissection22, radiotherapy and chemotherapy, using the same criteria than in women.
With respect to breast cancer prognosis by sex, Anderson et al.16 found that men had lower 5-year survival than women (0.72 vs. 1.27). However, after adjusting for age, year of diagnosis, stage and treatment, men had longer survival than women (0.78 vs. 0.62).
We consider as limitations that the study is of the respective nature of one surgeon's data-base, with a small number of cases and short follow-up, and therefore does not allow inferences to be made in other scenarios.
In conclusion, breast cancer in men is an infrequent disease, with age of presentation in the seventh decade of life, clinical symptoms of breast mass in all cases and breast ultrasound as the most used diagnostic method and complement in the guide for cutting biopsy. Diagnosis tends to be delayed due to late consultation, and most cases present in advanced stage, with immunophenotyping of A - B luminal predominance. The most commonly used surgical treatment is mastectomy, and adjuvant treatment tends to be homologous to that used in women.
REFERENCES
1. Onami S, Ozaki M, Mortimer JE, Pal SK. Male breast cancer: an update in diagnosis, treatment and molecular profiling. Maturitas. 2010 Apr;65(4):308-14. doi: 10.1016/j.maturitas.2010.01.012 [ Links ]
2. Instituto Nacional de Cancerología. Anuario Estadístico 2010. Instituto Nacional de Cancerología Colombia [consultado 4 septiembre 2012]. Disponible en: URL: http://www.cancer.gov.co/documentos/Anuario%20Estaditico/2010/Anuario%20Impreso 2010.pdf [ Links ]
3. Abad JFR, Mallarino JJC, Suárez RdA. Análisis de sobrevida en una cohorte de 1328 pacientes con carcinoma de seno. Rev Col Cirugia. 2005;20(1):4-20. [ Links ]
4. Gui G. Male breast cancer: aetiology and clinical features. Trends in Urology and Men´s Health. 2012;3(3):29-31. [ Links ]
5. Ewertz M, Holmberg L, Tretli S, Pedersen BV, Kristensen A. Risk factors for male breast cancer--a case-control study from Scandinavia. Acta Oncol. 2001;40(4):467-71. doi: 10.1080/028418601750288181 [ Links ]
6. Deb S, Jene N; Kconfab Investigators, Fox SB. Genotypic and phenotypic analysis of familial male breast cancer shows under representation of the HER2 and basal subtypes in BRCA-associated carcinomas. BMC Cancer. 2012 Nov 9;12:510. doi: 10.1186/1471-2407-12-510 [ Links ]
7. Ottini L, Palli D, Rizzo S, Federico M, Bazan V, Russo A. Male breast cancer. Crit Rev Oncol Hematol. 2010 Feb;73(2):141- 55. doi: 10.1016/j.critrevonc.2009.04.003 [ Links ]
8. Burstein HJ, Harris JR, Morrow M. Malignant tumors of the breast. In: De Vita VT, Lawrence TS, Rosenberg SA. Cancer. Principles and Practice of Oncology. 9 ed. Philadelphia: Lippincott Williams and Wilkins; 2011:1401-46. [ Links ]
9. Johansen Taber KA, Morisy LR, Osbahr AJ 3rd, Dickinson BD. Male breast cancer: risk factors, diagnosis, and management (Review). Oncol Rep. 2010 Nov;24(5):1115-20. doi: 10.3892/or_00000962 [ Links ]
10. Iuanow E, Kettler M, Slanetz PJ. Spectrum of disease in the male breast. AJR Am J Roentgenol. 2011 Mar;196(3):W247-59. doi: 10.2214/AJR.09.3994 [ Links ]
11. Anderson WF, Althuis MD, Brinton LA, Devesa SS. Is male breast cancer similar or different than female breast cancer? Breast Cancer Res Treat. 2004 Jan;83(1):77-86. doi: 10.1023/B:BREA.0000010701.08825.2d [ Links ]
12. Martínez-Tlahuel JL, Arce CL, Lara UF. Cáncer de mama en el hombre. Cancerología. 2006;4:201-10. [ Links ]
13. Robledo Abad JF, Caicedo Mallarino JJ, Suárez de Antonio R. Análisis de sobrevida en una cohorte de 1.328 pacientes con carcinoma de seno. Patología. 2005;4:5. [ Links ]
14. Ibañez R Gladys, Calderón G Maria Elsa, Márquez Z Domingo. Cáncer de mama en hombres: Situación actual a nivel mundial y nacional. Rev Chil Cir (Internet). 2011 Feb [citado 2021 Abr 11]; 63( 1 ): 95-101. [ Links ]
15. Angel J, Ibarra J, Diaz S, Lehmann C, Garcia M, Guzman L, Lopez D. Comportamiento clínico de cáncer de mama en hombres en una población latinoamericana. Rev Colomb Cancerol. 2015;19(3):150-5. doi:10.1016/j.rccan.2015.05.001 [ Links ]
16. Anderson WF, Jatoi I, Tse J, Rosenberg PS. Male breast cancer: a population-based comparison with female breast cancer. J Clin Oncol. 2010 Jan 10;28(2):232-9. doi: 10.1200/JCO.2009.23.8162 [ Links ]
17. Korde LA, Zujewski JA, Kamin L, Giordano S, Domchek S, Anderson WF, Bartlett JM, Gelmon K, Nahleh Z, Bergh J, Cutuli B, Pruneri G, McCaskill-Stevens W, Gralow J, Hortobagyi G, Cardoso F. Multidisciplinary meeting on male breast cancer: summary and research recommendations. J Clin Oncol. 2010 Apr 20;28(12):2114-22. doi: 10.1200/JCO.2009.25.5729 [ Links ]
18. Giordano SH, Buzdar AU, Hortobagyi GN. Breast cancer in men. Ann Intern Med 2002; 137(8):678-87. [ Links ]
19. Kornegoor R, Verschuur-Maes AH, Buerger H, Hogenes MC, de Bruin PC, Oudejans JJ, van der Groep P, Hinrichs B, van Diest PJ. Molecular subtyping of male breast cancer by immunohistochemistry. Mod Pathol. 2012 Mar;25(3):398-404. doi: 10.1038/modpathol.2011.174 [ Links ]
20. Yu XF, Feng WL, Miao LL, Chen B, Yang HJ. The prognostic significance of molecular subtype for male breast cancer: a 10-year retrospective study. Breast. 2013 Oct;22(5):824-7. doi: 10.1016/j.breast.2013.02.005 [ Links ]
21. Giordano SH, Perkins GH, Broglio K, Garcia SG, Middleton LP, Buzdar AU, Hortobagyi GN. Adjuvant systemic therapy for male breast carcinoma. Cancer. 2005 Dec 1;104(11):2359- 64. doi: 10.1002/cncr.21526 [ Links ]
22. De Cicco C, Baio SM, Veronesi P, Trifirò G, Ciprian A, Vento A, Rososchansky J, Viale G, Paganelli G. Sentinel node biopsy in male breast cancer. Nucl Med Commun. 2004 Feb;25(2):139- 43. doi: 10.1097/00006231-200402000-00008 [ Links ]
Received: April 25, 2021; Accepted: July 16, 2021











 texto en
texto en