Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.4 Lima Oct./Dec. 2021
http://dx.doi.org/10.31403/rpgo.v67i2361
Case Report
Vaginal vault leiomyoma after hysterectomy. Case report
21. Obstetrics and Gynecology Service, Hospital Central "Dr. Urquinaona , Maracaibo, Zulia, Venezuela
Leiomyomas are benign, mesenchymal tumors that usually arise from uterine smooth muscle cells, but can also occur in atypical sites such as the vagina, lungs and vascular structures. Post-hysterectomy vaginal vault leiomyomas are very rare and their etiology has not been determined. Transvaginal ultrasound, computed tomography and magnetic resonance imaging are useful tools for the diagnosis and follow-up of these patients. The definitive treatment is total removal of the tumor to avoid dissemination or inadvertent spillage of occult malignant neoplastic cells. Administration of gonadotropin-releasing hormone analogs or intravascular embolization may be alternative methods to reduce intraoperative blood loss. A case of vaginal vault leiomyoma following hysterectomy is presented.
Key words: Vagina; Leiomyoma; Hysterectomy
Introduction
Leiomyomas represent benign clonal proliferation of smooth muscle cells. They are the most common benign mesenchymal tumors of the uterus and can occur in any tissue containing smooth muscle cells, such as soft tissues of the skin, lungs, intravascular space, retroperitoneal area, bowel, eye, heart, lung, breast and bladder1.
The appearance of a leiomyoma in the vaginal vault long after hysterectomy is an extremely rare condition with symptoms that, depending on the size and anatomical location, can produce dyspareunia, dysuria and local pain. These must be surgically removed, due to possibility of malignancy and other complications2. A case of vaginal vault leiomyoma following hysterectomy is presented.
Clinical case
This was a 61-year-old menopausal patient, gestation 2, para 2, who consulted for presenting pain in the hypogastrium and left iliac fossa of 3 months of evolution, accompanied by dark brown vaginal discharge. She reported a history of vaginal hysterectomy with preservation of both adnexa due to metrorrhagia and uterine leiomyomas 15 years ago. The deliveries had been spontaneous, vaginally and without complications. The patient denied the use of hormone replacement therapy during menopause, smoking, alcohol consumption, illicit drugs, as well as personal or family history of neoplasms.
On physical examination, the abdomen was flat, depressible and there was a palpable tumor of pelvic origin, hard, solid, with irregular edges and immobile, approximately 9 centimeters, apparently adhered to the vaginal vault. Rectal examination showed that the tumor was located in the area corresponding to the right utero-sacral ligament. Speculoscopy exposed super-anterior deviation of the vaginal vault, with the presence of a brown vaginal discharge, not foul-smelling, in scant to moderate quantity. No erosions or macroscopic lesions were observed.
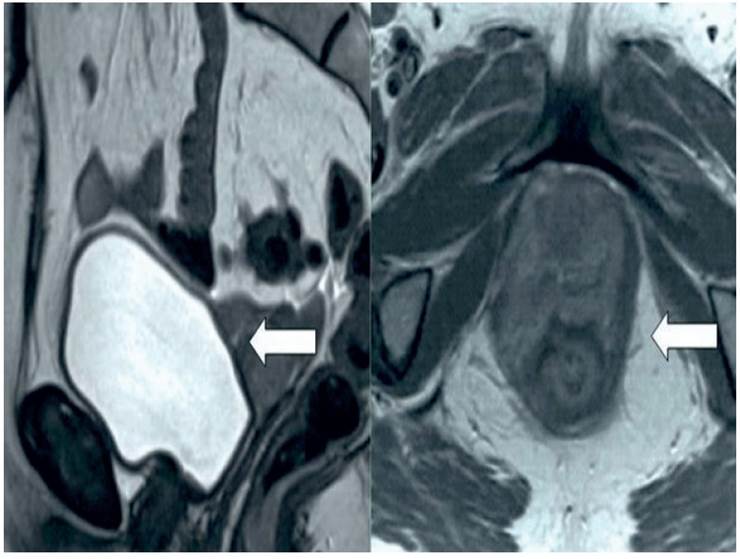
The results of complete hematology, electrolytes, liver and renal function, urine and coagulation tests were normal. Values of tumor markers CA-125, CA 19-9 and carcinoembryonic antigen were within normal ranges. Transvaginal ultrasound showed a solid tumor in the pelvic area, 9 centimeters in diameter, with high vascularization and evidence of neovascularization on Doppler evaluation. Magnetic resonance imaging showed the presence of a single smooth-walled tumor in the vaginal vault, measuring approximately 10 x 8 centimeters, with homogeneous signals on T1- and T2-weighted images (Figure 1). No intra-abdominal neoplasms or lymphadenopathies were observed. In view of the findings, it was decided to plan surgery to exclude the possibility of malignant pelvic neoplasia.
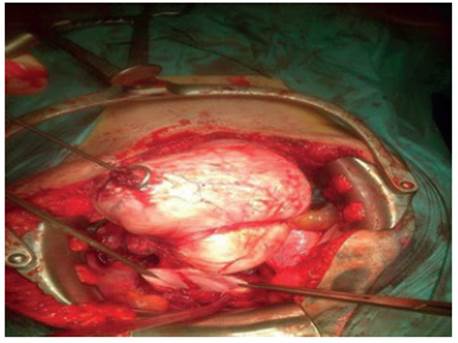
During exploratory laparotomy, a solid, well-circumscribed tumor measuring approximately 15 x 10 centimeters was found firmly attached to the vaginal vault, extending to the bilateral pararectal areas (Figure 2). Tumor was excised in its entirety along with both adnexa. There were no signs of abdominal or pelvic neoplastic disease.
Macroscopic evaluation by pathology showed that the tumor was rounded, firm and well circumscribed, approximately 14 x 10 centimeters. Microscopic examination found epithelioid cells with characteristic spindle-shaped, blunt-tipped nuclei and ample eosinophilic cytoplasm, without evidence of cellular atypia, with high isomorphism and cellular mitoses with low mitotic activity (0-1 / 10 high resolution fields) (Figure 3). Immunohistochemistry was positive for vimentin and smooth muscle actin. Both ovaries and fallopian tubes were normal. The final diagnosis was vaginal vault leiomyoma.
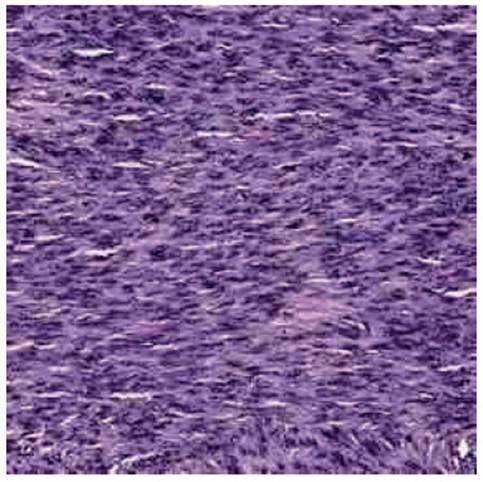
Figure 3 Microscopic image of vaginal leiomyoma with epithelioid cells with characteristic blunt-tipped spindle-shaped nuclei and large eosinophilic cytoplasm.
The patient had no postoperative complications and was discharged on the third day. During the 18-month follow-up she has had no symptoms or evidence of recurrence of leiomyomas in any location.
Discussion
Myomas are the most common pelvic tumors in women. Despite its high frequency in the general population, vaginal leiomyoma is an uncommon entity3. The occurrence of these tumors following hysterectomy is extremely rare and there are only reports of less than 10 cases and all patients had a history of uterine myomatosis. The clinical manifestation interval ranges from 1 to 25 years4.
The etiology of post-hysterectomy vaginal vault leiomyoma is unknown. Some hypotheses pro-pose hematogenous expulsion of uterine leiomyoma cells to adjacent organs, which would lead to the appearance of the tumor. Another theory proposes that it may arise from vaginal smooth muscle layer, from structures in the submucosal planes, from the round ligament or from the differentiation of mesenchymal stem cells2. This process seems to be enhanced by polygenic hereditary predisposition to develop leiomyomatosis, probably due to ethnic predisposition. It is also important to highlight that the use of exogenous estrogen or in supraphysiologic quantity can be a predisposing factor for this condition5.
Vaginal vault leiomyomas after hysterectomy may be asymptomatic or produce symptoms such as dyspareunia, dysuria, pollakiuria, lumbar pain, constipation, genital discharge due to erosion and pressure in the genital region. The severity of the symptomatology depends on the site and size of the lesion, since they are closely related to the compression of other nearby organs6,7.
Imaging diagnosis of vaginal vault leiomyoma can be difficult, because it could extend beyond the area of origin and simulate a malignant neoplasm. The most commonly used diagnostic techniques are transvaginal ultrasound and magnetic resonance imaging. Ultrasonography has a diagnostic sensitivity and specificity of 96% and 95%, respectively8. The lesion is sol-id, with a spiral appearance and sometimes hypoechoic. It usually presents acoustic shadows with scattering to the surrounding tissues. On Doppler evaluation, it appears with circumferential vascularization and high velocity flow along with low resistance index, indicative of neovascularization9.
Magnetic resonance imaging is useful to show the extension and its relationship with neighboring structures. Leiomyoma may appear as a single smooth tumor with low and homogeneous signal intensity on T1- and T2-weighted images. However, those tumors of cellular and vascular type may show hyperintensity in T2-weighted references images and marked contrast enhancement10. Nevertheless, it is always necessary to consider the possibility of malignancy, so histopathological confirmation is the diagnostic standard to rule out the presence of malignant neoplastic components6.
The definitive treatment of post-hysterectomy vaginal vault leiomyoma is total resection to prevent inadvertent spread or spillage of occult malignant neoplasms. Surgical excision can be performed vaginally, laparoscopically or abdominally, depending on size, location and accessibility of tumor. Transvaginal myomectomy by transluminal endoscopy through natural orifices is also a feasible alternative. These fibroids are usually easily dissected without severe blood loss. In those cases with large tumors, administration of gonadotropin-releasing hormone analogs or intravascular embolization may be effective methods to avoid intraoperative bleeding11. Although recurrence is uncommon, there is one report of a recurrent giant vaginal leiomyoma12.
Leiomyomas are hormone-dependent tumors that generally increase in size in premenopausal women and decrease at menopause. It has been proposed that the increase in volume depends on the complex relationship between hormones and locally active factors13. The presence of receptors for estrogen, progesterone, and epidermal growth factor has been documented1. Several investigators have proposed that there is evidence of recurrence of benign lesions when adnexa are preserved during hysterectomy. These findings would indicate that tumor growth could be controlled with bilateral oophorectomy2. Long-acting gonadotropin-releasing hormone analogs suppress endogenous gonadotropin secretion and gonadal steroid production, so they may be useful in treatment in certain cases14. There are also reports indicating that progesterone may be effective in specific cases15.
In conclusion, although rare, vaginal vault leiomyomas can appear sometime after hysterectomy. This condition should be considered as a differential diagnosis of pelvic mass in patients with a history of hysterectomy with or without adnexal preservation, as they can develop up to 25 years after surgery. Surgical removal is the definitive treatment.
REFERENCES
1. Yarci A, Bayramov V, Sükür YE, Yüce T, Berker B. Vaginal vault leiomyoma: 25 years after total abdominal hysterectomy. J Minim Invasive Gynecol. 2010;17(1):116-7. doi: 10.1016/j.jmig.2009.10.004 [ Links ]
2. Yanamandra SR, Redman CW, Coomarasamy A, Varma R. Leiomyoma appearing in the vaginal vault following hysterectomy. J Obstet Gynaecol. 2007;27(1):91-2. doi: 10.1080/01443610601076176 [ Links ]
3. Patil RR, Vijay NR, Joshi S. An unusual presentation of vaginal leiomyoma. J Midlife Health. 2019;10(4):204-5. doi: 10.4103/jmh.JMH_40_19 [ Links ]
4. Agostini A, Banet J, Bretelle F, Cravello L, Blanc B. Leiomyoma remaining after vaginal hysterectomy for symptomatic leiomyomas. A case report. J Reprod Med. 2003;48(2):119- 20. [ Links ]
5. Xiao J, Zhang R, Teng Y, Liu B. Disseminated peritoneal leiomyomatosis following laparoscopic myomectomy: a case report. J Int Med Res. 2019;47(10):5301-6. doi: 10.1177/0300060519859137 [ Links ]
6. Kyriakopoulos K, Domali E, Stavrou S, Rodolakis A, Loutradis D, Drakakis P. Recurrent benign leiomyomas after total abdominal hysterectomy. Rich or poor estrogenic environment may lead to their recurrence? Int J Surg Case Rep. 2018;44:191-3. doi: 10.1016/j.ijscr.2018.02.029 [ Links ]
7. Tanaka Y, Nagasaka M, Takahashi M, Kobayashi M. Rare epithelioid leiomyoma of the vagina exhibiting a pelvic mass. Case Rep Obstet Gynecol. 2017;2017:2190135. doi: 10.1155/2017/2190135 [ Links ]
8. Sharma K, Bora MK, Venkatesh BP, Barman P, Roy SK, Jayagurunathan U, et al. Role of 3D ultrasound and Doppler in differentiating clinically suspected cases of leiomyoma and adenomyosis of uterus. J Clin Diagn Res. 2015;9(4):QC08-12. doi: 10.7860/JCDR/2015/12240.5846 [ Links ]
9. Keizer AL, Nieuwenhuis LL, Twisk JWR, Huirne JAF, Hehenkamp WJK, Brölmann HAM. Role of 3-dimensional sonography in the assessment of submucous fibroids: a pilot study. J Ultrasound Med. 2018;37(1):191-9. doi: 10.1002/jum.14331 [ Links ]
10. Egbe TO, Kobenge FM, Metogo JAM, Manka'a Wankie E, Tolefac PN, Belley-Priso E. Vaginal leiomyoma: medical imaging and diagnosis in a resource low tertiary hospital: case report. BMC Womens Health. 2020;20(1):12. doi: 10.1186/s12905-020-0883-2 [ Links ]
11. Bapuraj JR, Ojili V, Singh SK, Prasad GR, Khandelwal N, Suri S. Preoperative embolization of a large vaginal leiomyoma: report of a case and review of the literature. Australas Radiol. 2006;50(2):179-82. doi: 10.1111/j.1440-1673.2006.01550.x [ Links ]
12. Dhaliwal LK, Das I, Gopalan S. Recurrent leiomyoma of the vagina. Int J Gynaecol Obstet. 1992;37(4):281-3. doi: 10.1016/0020-7292(92)90330-l [ Links ]
13. Maruo T, Ohara N, Wang J, Matsuo H. Sex steroidal regulation of uterine leiomyoma growth and apoptosis. Hum Reprod Update. 2004;10(3):207-20. doi: 10.1093/humupd/dmh019 [ Links ]
14. Wei WT, Chen PC. Benign metastasizing leiomyoma of the lung: A case report and literature review. Oncol Lett. 2015;10(1):307-12. doi: 10.3892/ol.2015.3224 [ Links ]
15. Jautzke G, Müller-Ruchholtz E, Thalmann U. Immunohistological detection of estrogen and progesterone receptors in multiple and well differentiated leiomyomatous lung tumors in women with uterine leiomyomas (so-called benign metastasizing leiomyomas). A report on 5 cases. Pathol Res Pract. 1996;192(3):215-23. doi: 10.1016/S0344-0338(96)80224-X [ Links ]
Declaration of ethical aspects
Ethical responsibilities: Protection of persons. We the authors declare that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Confidentiality of data: The authors declare that we have followed the protocols of the Hospital Central "Dr. Urquinaona" on the publication of patient data.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Financing: The authors certify that we have not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the study.
Received: January 11, 2021; Accepted: March 14, 2021











 text in
text in