Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.4 Lima oct./dic 2021
http://dx.doi.org/10.31403/rpgo.v67i2363
Case Report
Pseudoangiomatous stromal hyperplasia (PASH) in a 14-year-old girl: a case report
1 Department of Surgical Specialties, Instituto Nacional de Salud del Niño San Borja, Lima, Peru
Pseudoangiomatous stromal hyperplasia (PASH) occurs between 12 and 75 years of age, being prevalent in the reproductive age. Its etiology is unknown. They are characterized by being large, deforming, unilateral and are diagnosed by ultrasound and histology. In adolescents, early surveillance, diagnosis and management is important in order to avoid radical surgeries that cause large scars, deformity and breast asymmetry, which have repercussions on the behavior and emotional state of the patients. Breast tumors are generally benign in adolescence, but their diagnosis in this age group is worrisome for the family and the patient. We present the case of a 14-year-old adolescent who underwent a submammary approach, preserving breast symmetry.
Key words: Breast neoplasms; Adolescent; Ultrasonography; mammary; Mastectomy; segmental
INTRODUCCIÓN
Pseudoangiomatous stromal hyperplasia, commonly known as PASH, is a rare benign disease and its etiology is currently unknown1. It was first described in 1986 by Vuitch et al2, and appears frequently between the ages of 12 to 75 years3. It presents as a large, solitary, firm, painless, circumscribed, delimited and mobile nodular mass of variable size between 2 and 13 cm. Frequently unilateral, there are reports of bilaterality4. In some cases, it is diagnosed in the biopsy. PASH can also arise in the axillary tail of the breast and very rarely involves the nipple-areola complex and the axillary accessory breast tissue1. The most important differential diagnosis is with angiosarcoma5.
Excisional biopsy is the treatment and the final diagnosis is histologic6. Diagnosis, management and esthetic outcome are very important in this age group. These large tumors are deforming and require early surveillance, diagnosis and management in order to avoid radical surgeries that cause large scars, deformity and asymmetry, and may have repercussions on the behavior and emotional state of the adolescent.
Among the most common benign breast tumors in adolescence are juvenile fibroadenoma, juvenile hypertrophy (virginal) and pseudoangiomatous stromal hyperplasia. Phyllodes tumors, lymphomas, angiosarcomas are extremely rare7-10).
We present the case of a patient who underwent a submammary approach that preserved breast symmetry and esthetics.
PRESENTATION OF THE CLINICAL CASE
An adolescent girl aged 14 years and 3 months reported that she noticed a progressive increase in the size of her right breast over 6 months, with asymmetry of the breasts and no pain. Her 42-year-old mother was a housewife and her 43-year-old father was a businessman, both apparently healthy. The teenager was born with a normal delivery, weighing 3,200 g, had complete vaccinations, menarche at 11 years of age, catamenial regimen 4/30, without dysmenorrhea.
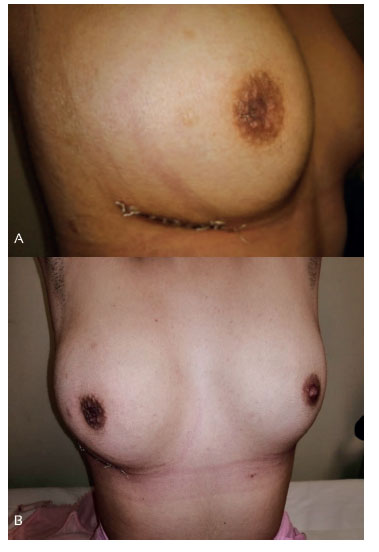
At the admission examination she weighed 53 kg, height 1.54 m, body mass index 22.3, cooperative during the evaluation. General, nutritional and hydration status was regular. The right breast, Tanner stage 4, was occupied by a single mass with defined borders of 9 x 6 cm in radius 6 to radius 12, mobile, non-painful, of hard consistency and deforming the nipple and areola. The left breast, Tanner stage 4, showed no alterations. Biochemistry, hematological and urine tests were normal. Right breast ultrasound showed a circumscribed oval mass with acoustic shadow, measuring 9 x 6 cm in radius 11 and 12 (Figure 1).
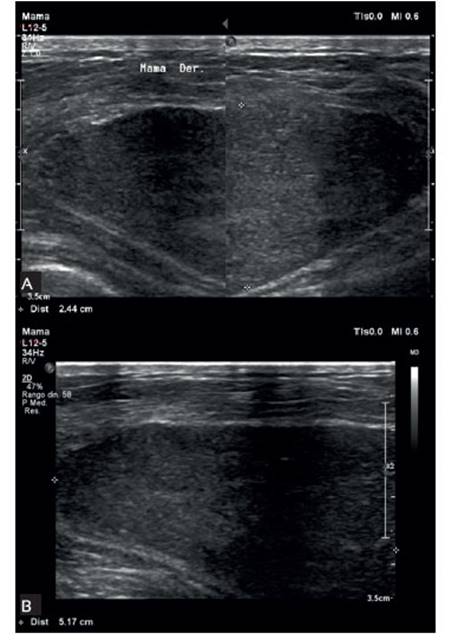
Figure 1 (a, b). in the breast ultrasound before surgery, the findings are variable, but in most cases a solid, circumscribed, oval or rounded mass is observed, as in the case presented.
Surgical treatment consisted of excision of the tumor (Figure 2) through a submammary approach (Figure 3). No complications were evidenced during the postoperative period, and she was discharged after 1 day of hospitalization, with analgesics, antibiotics and breast bandage. She went to the control 72 hours after de postoperative period for removal of the bandage. After one week the sutures were removed. On physical examination, the operative wound was closed and without phlogosis.

Figure 2 Operative specimen: a solid mass with defined borders, grayish brown, 11 x 7.7 x 5.5 cm, is observed.
The histological report was: Grayish-brown tumor of 11 x 7.7 x 5.5 cm in size. Final diagnosis:
Pseudoangiomatous stromal hyperplasia (PASH) (Figure 4). Currently, the patient continues to be monitored and with favorable follow-up. In the last control in 2021, there was no evidence of another tumor growth.

Figure 4 histological description: (a) histological study confirms pseudoangiomatous stromal hyperplasia: histological sections show mammary parenchyma with numerous stromal clefts. these clefts are lined by myofibroblasts. the spaces produced by the clefts are empty, simulating complex anastomosed blood vessels. (b) clefts surround lobules of normal appearance and involve both the interlobular and the intralobular stroma.
DISCUSSION
We report the first case of PASH in our institution, being important to make known this pathology, frequent between the ages of 12 to 75 years and more prevalent in women of reproductive age. In adolescence, they are usually benign. The etiology of PASH is unknown.
A complete medical history, general physical examination and breast examination should be performed in any gynecologic check-up of an adolescent girl. In these cases, the patient will come for consultation with a well-demarcated, hard, non-painful, deforming and rapidly growing lump.
The differential diagnosis of breast tumors is fundamental for management of fibroadenomas, gigantojuvenile fibroadenomas, phyllodes tumor, lymphoma. Among the diagnostic tests, breast ultrasound11-13,16 in this type of tumor is non-specific, generally finding a solid, circumscribed, oval or round mass. The diagnosis is anatomopathological; a breast parenchyma with numerous stromal clefts is described. These clefts are lined by myofibroblasts15. The spaces produced by the clefts are empty, simulating complex anastomosed blood vessels. The clefts are present in both the interlobular and intralobular stroma.
In this age group, the surgical approach should be conservative and adequate. Patients should be followed up, because recurrence occurs in around 15 and 22% of cases8,14,16.
In conclusion, pseudoangiomatous stromal hyperplasia is a lesion that is generally seen in women of reproductive age or as an incidental finding as a result of a biopsy. However, it has also been described in girls and adolescents as a palpable, unilateral, firm, non-painful, mobile mass. Diagnosis is by imaging and histology. Differential diagnosis with gigantojuvenile fibroadenomas and lymphomas is essential. Surgical treatment should be conservative in this age group.
REFERENCES
1. Singh KA, Lewis MM, Runge RL, Carlson GW. Pseudoangiomatous stromal hyperplasia. A case for bilateral mastectomy in a 12-year-old girl. Breast J. 2007 Nov-Dec;13(6):603-6. doi: 10.1111/j.1524-4741.2007.00499.x [ Links ]
2. Vuitch MF, Rosen PP, Erlandson RA. Pseudoangiomatous hyperplasia of mammary stroma. Hum Pathol. 1986 Feb;17(2):185-91. doi: 10.1016/s0046-8177(86)80292-1 [ Links ]
3. Ferreira M, Albarracin CT, Resetkova E. Pseudoangiomatous stromal hyperplasia tumor: a clinical, radiologic and pathologic study of 26 cases. Mod Pathol. 2008 Feb;21(2):201-7. doi: 10.1038/modpathol.3801003 [ Links ]
4. Tumeh RA, Sabino Neto M, Cunha AL, Silva MM de A, de Paula HR, Ferreira LM. Hiperplasia estromal pseudoangiomatosa: caso raro em menina de 11 anos. Rev bras cir plast. 2017;32(2):295-8. [ Links ]
5. Virk RK, Khan A. Pseudoangiomatous stromal hyperplasia: an overview. Arch Pathol Lab Med. 2010 Jul;134(7):1070-4. doi: 10.1043/2008-0686-RS.1 [ Links ]
6. Pohlodek K, Minarovjech V, Gál V, Meciarová I. Tumorous form of pseudoangiomatous stromal hyperplasia of the breast in a young female and a young male. Am J Surg. 2018;35(3):105-9. doi:10.1177/0748806818764152 [ Links ]
7. Khokher S, Shahzad R, Shahbaz S. Pseudoangiomatous hyperplasia of breast: Report of two cases presenting with giant tumors and literature review. Qual Prim Care. 2016;24(3):111-3. [ Links ]
8. Jaunoo SS, Thrush S, Dunn P. Pseudoangiomatous stromal hyperplasia (PASH): a brief review. Int J Surg. 2011;9(1):20-2. doi: 10.1016/j.ijsu.2010.09.005 [ Links ]
9. Baker M, Chen H, Latchaw L, Memoli V, Ornvold K. Pseudoangiomatous stromal hyperplasia of the breast in a 10-yearold girl. J Pediatr Surg. 2011 Aug;46(8):e27-31. doi: 10.1016/j.jpedsurg.2011.04.063 [ Links ]
10. Weinstein SP, Conant EF, Orel SG, Zuckerman JA, Bellah R. Spectrum of US findings in pediatric and adolescent patients with palpable breast masses. Radiographics. 2000 Nov-Dec;20(6):1613-21. doi: 10.1148/radiographics.20.6.g00nv091613 [ Links ]
11. Chung EM, Cube R, Hall GJ, González C, Stocker JT, Glassman LM. From the archives of the AFIP: breast masses in children and adolescents: radiologic-pathologic correlation. Radiographics. 2009 May-Jun;29(3):907-31. doi: 10.1148/rg.293095010 [ Links ]
12. Kaneda HJ, Mack J, Kasales CJ, Schetter S. Pediatric and adolescent breast masses: a review of pathophysiology, imaging, diagnosis, and treatment. AJR Am J Roentgenol. 2013 Feb;200(2):W204-12. doi: 10.2214/AJR.12.9560 [ Links ]
13. Goel NB, Knight TE, Pandey S, Riddick-Young M, de Paredes ES, Trivedi A. Fibrous lesions of the breast: imaging-pathologic correlation. Radiographics. 2005 NovDec;25(6):1547-59. doi: 10.1148/rg.256045183 [ Links ]
14. Irshad A, Ackerman SJ, Pope TL, Moses CK, Rumboldt T, Panzegrau B. Rare breast lesions: correlation of imaging and histologic features with WHO classification. Radiographics. 2008 Sep-Oct;28(5):1399-414. doi: 10.1148/rg.285075743 [ Links ]
15. Hoda SA, Rosen PP. Observations on the pathologic diagnosis of selected unusual lesions in needle core biopsies of breast. Breast J. 2004 Nov-Dec;10(6):522-7. https://doi.org/10.1111/j.1075-122X.2004.21412.x [ Links ]
16. Jones KN, Glazebrook KN, Reynolds C. Pseudoangiomatous stromal hyperplasia: imaging findings with pathologic and clinical correlation. Am J Roentgenol. 2010 Oct;195(4):103642. doi: 10.2214/AJR.09.3284 [ Links ]
Received: January 19, 2021; Accepted: May 07, 2021











 texto en
texto en