Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.4 Lima Oct./Dec. 2021
http://dx.doi.org/10.31403/rpgo.v67i2373
Case Report
Vulvar syringomas: case report
1. Obstetrician-Gynecologist, Hospital Nacional Dos de Mayo, Lima, Peru
2. Obstetrician-Gynecologist, Hospital Nacional Dos de Mayo, Lima, Peru
Syringomas are benign adnexal tumors rarely reported at the vulvar area. A case is reported and a literature review is performed for the presentation of a 33-yearold woman with multiple papular lesions in labia majora, of long standing, with anatomopathologic diagnosis and treatment by surgical excision under sedation and CO2 laser vaporization.
Key words: Vulva; Vulvar diseases; Syringoma; Laser therapy
Introduction
Syringomas are benign adnexal tumors, derived from the ductal portion of the eccrine sweat glands; however, they are frequently located in areas rich in apocrine glands (lower eyelids, axillae, abdomen) and are rarely found in the genital area1,2. They manifest in adolescence or during the third and fourth decades of life and present clinically as multiple firm papules 1 to 3 mm in diameter, skin-colored or with a slight yellowish tinge, symmetrical and bilateral arrangement3,4.
We report a case of vulvar syringomas, due to its infrequent location and the diagnostic challenge with other vulvar pathologies.
Case report
We report the case of a 33-year-old woman, G2 P2002, who had undergone cesarean section twice, who presented multiple vulvar lesions since she was 11 years old, increasing in number from the age of 20 and in volume during the two periods of pregnancy. Previous evaluations had suggested the diagnosis of condyloma acuminata, with no indication for treatment.
Throughout the evolution, there was no association with dermatosis or vulvar pruritus and there was no clinical history of relevance to the case. Both cervical cytology and molecular test for human papillomavirus were negative.
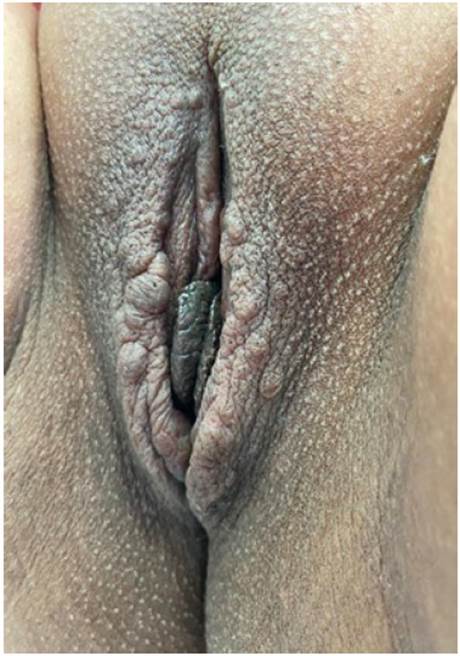
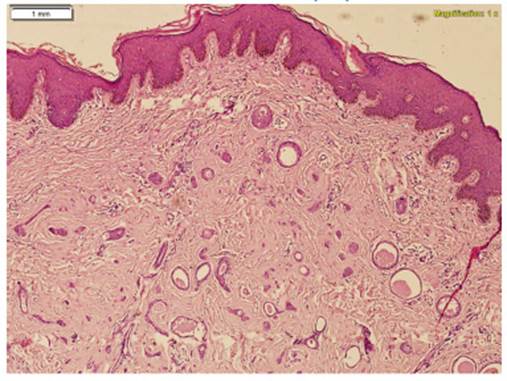
On physical examination, both labia majora showed multiple movable papular lesions between 2 and 6 mm in diameter, of brownish color and soft consistency, covered by skin (Figure 1). The rest of the examination showed no alterations. Subsequently, an incisional biopsy was performed with a 5 mm punch for histopathological study. The microscopic description (Figure 2) showed a vulvar tissue with the presence of a circumscribed lesion with small ducts and narrow to dilated lumens and lined by a cuboidal epithelium with two layers of thickness surrounded by a fibrous stroma.
Given the anatomopathologic diagnosis, the patient requested treatment for cosmetic purposes. Surgical excision under sedation and CO2 laser vaporization of the satellite lesions was scheduled (Figure 3). The pieces were sent to pathology and the microscopic description (Figure 4) showed multiple benign nodular lesions of subepithelial location, due to proliferation of small eccrine glands without significant cellular atypia.
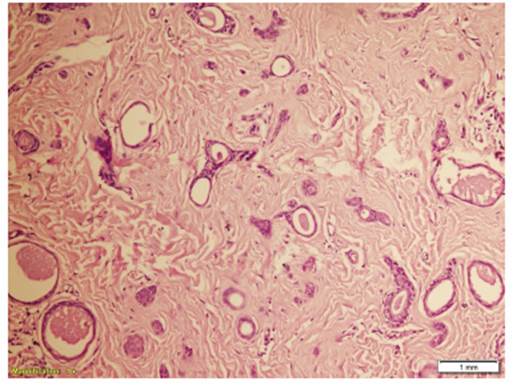
Figure 4 Structures lined by a cuboidal epithelium, with a 'comma' or 'tadpole' shape, surrounded by a fibrous stroma. (20x)
The patient had postoperative follow-up without complications and adequate epithelization. She had a favorable evolution, manifesting personal satisfaction and improved self-esteem.
Discussion
Syringomas occur more frequently in women than in men (2:1 ratio). They are classically located at the periorbital level and there are few published cases at the vulvar level, which can manifest in isolation or associated with extra-genital lesions5. During the physical examination 3 types of skin lesions can be evidenced, such as: multiple skin-colored or brownish papules (61%), lichenified plaques (22%) or whitish cystic papules (17%). These usually present asymptomatically, making the clinical diagnosis of vulvar syringoma difficult6, although they may have cyclic changes in size. The lesions are exacerbated during the premenstrual period, the use of oral contraceptives and pregnancy, and may present genital itching7. These events suggest the role of the hormonal environment and steroid receptors8. In this case, multiple skin-colored papular lesions were found at the vulvar level, without extragenital lesions, asymptomatic and long-standing, which increased in number and volume during pregnancy, as described in the literature.
The diagnosis is made by histopathological study, in which a normal epidermis and dermal proliferation is observed, constituted by tubular eccrine-like structures, some of which present prolongations resembling a comma or a tadpole. The epithelial lining is given by a double layer of cuboidal cells, surrounded by stroma of densely fibrous collagen bundles1,9.
A variety of lesions can affect the vulva. These can be non-neoplastic or represent benign or malignant neoplasms10. Among the differential diagnoses are epidermal cysts, milia, multiple statocystomas, Fox-Fordyce disease, circumscribed lymphangioma, condyloma acuminata, molluscum contagiosum, lichen planus and lichen simplex chronicus1,2,5,9. Therefore, a biopsy will be necessary. We note that the prevalence of this entity may be underdiagnosed as it is underrecognized and asymptomatic.
The goal of syringoma treatment is to improve the esthetic appearance, because these lesions are considered benign, non-progressive and typically asymptomatic11. Both medical and surgical interventions have been described in the literature, with variable success. No treatment has been shown to be consistently effective.
Both medical and surgical treatments are available. Within medical management, retinoids target cell proliferation, differentiation and keratinization, atropine inhibits sweat production, tranilast can suppress syringoma stromal connective tissue proliferation by inhibiting interleukin-1 beta release from eccrine ducts. Oral antihistamines and topical corticosteroids are recommended in cases of pruritus but not for the treatment of syringomas5,11,12.
From the surgical point of view, treatments have been described with curettage, surgical excision, in addition to ablative methods such as electrocoagulation, cryotherapy, use of CO2 laser, argon laser and combination of application of 35% trichloroacetic acid plus CO2 laser with multiple perforation technique. This combination can reduce the degree of tissue damage produced when only CO2 laser is used, synergistically stimulate type I collagen synthesis and promote tissue regeneration. It is important to note that recurrence, scar formation and depigmentation often complicate ablative procedures7,11.
REFERENCES
1. Martínez MJ, Marchitelli CE, Sluga MC, Wernicke A, Gogorza SJ. Siringomas vulvares. Dermatol Argent. 14 de junio de 2017;23(2):95-7. ISSN 1669-1636 [ Links ]
2. Flores IC, Oliveros TG, Cabello DG. Siringomas en la vulva. Dermatol Rev Mex. 2011;55(3):152-4. ISSN 0185-4038 [ Links ]
3. Lernia VD, Bisighini G. Localized vulvar syringomas. Pediatr Dermatol. 1996;13(1):80-1. https://doi. org/10.1111/j.1525-1470.1996.tb01198.x [ Links ]
4. Villagrasa-Boli P, Bularca E-A, Martínez Pallás I, García García M, de la Fuente Meira S. Siringomas vulvares; cuando el diagnóstico diferencial es un reto. Clínica e Investig en Ginecol Obstet [Internet]. 17 de julio de 2020 [citado 23 de marzo de 2021]. DOI: 10.1016/j.gine.2020.06.006 [ Links ]
5. Baquerizo Nole KL, Tolentino Moreno J, Arroyo P, Castro Vargas E, Muñoz S. Siringomas vulgares, patología frecuente en una localización infrecuente. Folia Dermatol Peru. 2006;72- 5. ID: lil-475618 [ Links ]
6. Pérez-Bustillo A, Ruiz-González I, Delgado S, Alonso T, Ingelmo J. Siringomas vulvares: una causa infrecuente de prurito vulvar. Actas Dermo-Sifiliográficas. 1 de septiembre de 2008;99(7):580-1. DOI: 10.1016/S0001-7310(08)74752-5 [ Links ]
7. Huang Y-H, Chuang Y-H, Kuo T, Yang L-C, Hong H-S. Vulvar syringoma: A clinicopathologic and immunohistologic study of 18 patients and results of treatment. J Am Acad Dermatol. 1 de mayo de 2003;48(5):735-9. DOI: 10.1067/mjd.2003.285 [ Links ]
8. Turan C, Ugur M, Kutluay L, Kükner S, Dabakoglu T, Aydogdu T, et al. Vulvar syringoma exacerbated during pregnancy. Eur J Obstet Gynecol Reprod Biol. January 1996;64(1):141-2. DOI: 10.1016/0301-2115(95)02246-5 [ Links ]
9. Tadeo MTS, Rivera MP. Siringomas vulvares: reporte de caso y revisión de la literatura. 2017;4. [ Links ]
10. Heller DS. Benign tumors and tumor-like lesions of the vulva. Clin Obstet Gynecol. Sept. 2015;58(3):526-35. DOI: 10.1097/GRF.0000000000000133 [ Links ]
11. Williams K, Shinkai K. Evaluation and management of the patient with multiple syringomas: A systematic review of the literature. J Am Acad Dermatol. 1 June 2016;74(6):1234-40. e9. DOI: 10.1016/j.jaad.2015.12.006 [ Links ]
12. Kavala M, Can B, Zindanci I, Kocatürk E, Türkoglu Z, Büyükbabani N, et al. Vulvar pruritus caused by syringoma of the vulva. Int J Dermatol. 2008;47(8):831-2. DOI: https://doi.org/10.1111/j.1365-4632.2008.03664.x [ Links ]
Received: April 28, 2021; Accepted: June 25, 2021











 text in
text in