Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.4 Lima oct./dic 2021
http://dx.doi.org/10.31403/rpgo.v67i2375
Case Report
Prenatal diagnosis of thrombosis of the torcula of Herophilus
1. Obstetrics and Gynecology Service, Hospital Central "Dr. Urquinaona , Maracaibo. Zulia State, Venezuela
Thrombosis of the torcula of Herophilus is a rare disease of unknown etiology. So far about 50 cases have been described in the literature. Ultrasonography is an effective diagnostic method and useful for follow-up. Characteristic sonographic findings include a well-defined triangular anechoic lesion in the occipital region, with echogenic structure inside which is the thrombus. Doppler ultrasound can help to establish the diagnosis more precisely. The prognosis is variable, as most cases have an irrelevant clinical course due to spontaneous resolution of the thrombus, while other cases may experience cerebral atrophy and death. A case of prenatal diagnosis of thrombosis of the torcula of Herophilus is presented.
Key words: Thrombosis; torcula of Herophilus; Prenatal diagnosis
Introduction
Thrombosis of the confluence of the cerebral venous sinuses, or torcula of Herophilus, is a rare fetal cerebrovascular condition, but represents the most frequently diagnosed cerebral thrombotic event during fetal life, with approximately 50 cases reported in the literature1,2. Suspicion of this disorder usually occurs during routine prenatal ultrasound evaluation, but it is often not diagnosed with certainty, as it can be confused with other similar posterior fossa lesions. The neonatal prognosis can range from spontaneous resolution without neurological complications to severe neurological impairment and death3. A case of prenatal diagnosis of thrombosis of the torcula of Herophilus is presented.
Case report
A 22-year-old female patient, gestation II, para I, with a 28-week pregnancy was referred to the high-risk prenatal clinic for assessment of a cystic structure in the fetal posterior cerebral fossa found during routine prenatal ultrasound. The patient denied personal or family history of thrombosis, anemia, hemorrhage and coagulation disorders.
Ultrasound evaluation showed a single female fetus with normal biometry and normal amniotic fluid volume for gestational age (29 weeks). Fetal brain evaluation denoted a triangular heterogeneous lesion located in the posterior fossa above the midline and immediately above the cerebellar tentorium, 23 millimeters in diameter. Within this lesion was a 12 × 10 × 9 millimeter echogenic formation compatible with a blood clot. The cerebral hemispheres were slightly displaced, without ventriculomegaly (Figure 1). Color Doppler showed no evidence of flow within the lesion. In the posterior fossa, the cerebellum, vermis and cisterna magna were normal. There was no evidence of associated intra- or extracranial lesions or signs of cardiac insufficiency. The location and appearance of the lesion raised the possibility of the torcula of Herophilus (confluence of the fetal cerebral venous sinuses).
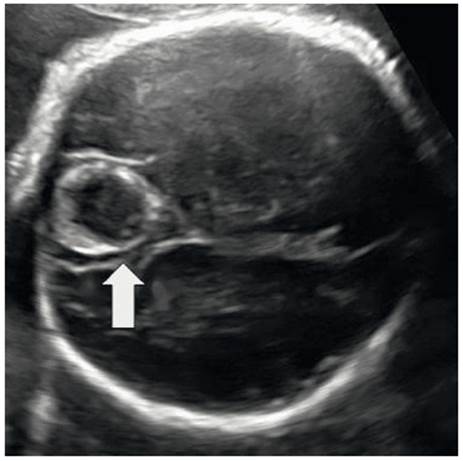
Figure 1 Ultrasound image of fetal Herophilus torcula thrombosis at 29 weeks of gestation. The arrow indicates the position of the lesion in the fetal posterior cerebral fossa.
Prenatal magnetic resonance imaging at 32 weeks showed a triangular-shaped hyperintense lesion in the posterior fossa, corresponding to the area of the torcula of Herophilus, with organized thrombus inside, slight dilatation of the longitudinal venous sinus and no evidence of compression of the surrounding tissues (Figure 2).
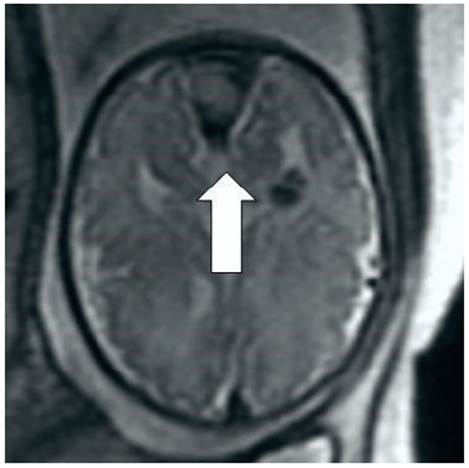
Figure 2 Magnetic resonance image at 32 weeks. The arrow indicates a triangular-shaped lesion in the posterior fossa compatible with thrombosis of the torcula of Herophilus.
In view of the findings, different laboratory tests were performed. The platelet count and maternal prothrombin time were normal and the indirect Coombs test was negative. No auto- or alloimmune anti-platelet antibodies were detected. Screening tests for cytomegalovirus, toxoplasmosis, rubella and herpes simplex resulted in positive IgG for toxoplasmosis, rubella and cytomegalovirus and negative IgM values. Both IgM and IgG for herpes simplex were negative. Genetic amniocentesis results showed 46,XX karyotype with no structural abnormalities.
On subsequent ultrasound evaluations the lesion was found to be increasingly echogenic, while the contents had more heterogeneous characteristics, showing echogenic anechoic areas. The diameter of the lesion had decreased to 11 millimeters at 35 weeks (Figure 3).
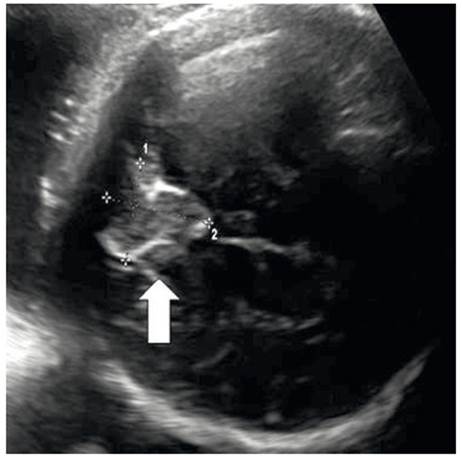
Figure 3 Ultrasound image of fetal Herophilus torcula thrombosis at 35 weeks of gestation. The arrow indicates the location of the lesion with decreased diameter and echogenic changes.
At 39 weeks, a cesarean section was performed due to wedging dystocia and descent, resulting in a live female newborn in good general condition, weighing 3,500 grams and with a good transition to postnatal life (Apgar scores of 6 and 9 at one minute and 5 minutes, respectively). Physical and neurological examinations showed no alterations. Transfontanelar ultrasound showed a lesion of approximately 9 millimeters in diameter above the tentorium, near the occipital bone. Hematologic, biochemical and coagulation profiles were normal. Coagulation tests showed normal results for platelet count, prothrombin time, activated partial thromboplastin time and fibrinogen. Lupus anticoagulant, protein S and protein C concentrations were normal and there was no evidence of factor V Leiden mutation. MRI two months after delivery showed resolution of the clinical picture. The child has had somatic and cognitive development according to her age and no evidence of intracranial hypertension after 30 months of follow-up.
Discussion
Maternal coagulation disorders, prematurity, perinatal asphyxia and perinatal trauma have been reported as predisposing factors for neonatal cerebral sinus thrombosis4. However, the etiology of thrombosis of the torcula of Herophilus is unknown and has been the subject of in-tense discussion. Due to its low frequency, there is insufficient epidemiological data on its origin and whether there is an increased incidence related to fetal sex2,5.
The embryological development of the fetal cerebral vasculature is complex. The dura mater is the outermost of the meninges, and its expansions, the septum pellucidum and tentorium, divide the cerebral volume. This is a relatively lax structure that allows some distension in response to hydrostatic changes in the drainage of the local venous system. The dural sinuses are duplications of the dura mater, which contain the cerebral venous system. There are two venous systems: deep and superficial, which form at 15 weeks of gestation. Between the fifth and twelfth day of conception, the organization of the arterial vessels occurs and subsequently the upper and lower central cerebral venous system develops until 20 weeks. The development of the major venous system ends, but the connection of the other vessel system and the internal calibration of the transverse sinus continues5,6.
The dural venous sinuses are endothelium-lined intracranial channels that run between the two layers of the dura mater and are characterized by lacking muscular walls and venous valves. The superior sagittal, rectus and occipital sinus meet in the area of the cerebellar tentorium, a region called the confluence of dural venous sinuses or torcula of Herophilus, which drains into the bilateral transverse sinuses and then into the internal jugular veins5.
Thrombosis of the torcula of Herophilus seems to be related to the persistence of physiological ballooning of the transverse or posterior portion of the superior sagittal sinus, between the fourth and sixth month of fetal development, which leads to alterations in blood flow, modifications of the endothelial lining and the appearance of low-flow accessory shunts7,8. Another hypothesis proposes excessive and anarchic development of the vascular region. However, it is not possible to determine whether this occurs before the thrombotic event or arises as a consequence of it9.
Ultrasound is the initial diagnostic technique in cases of thrombosis of the torcula of Herophilus10. The ultrasound appearance varies depending on the size and stage of thrombus formation (in some cases causing distortion of surrounding structures). Typical sonographic findings include hypoechoic/anechoic, triangular, well-defined lesion above the tentorium and thus in close relation to the cerebellum and occipital bone, with an echogenic structure inside, corresponding to the thrombus. In addition, distal dilatation of the superior sagittal sinus is almost always present due to retrograde venous hypertension. On ultrasound follow-up, this thrombus usually shows the usual changes of organization and subsequent retraction over a period of 3 to 11 weeks, allowing for complete anatomical remodeling9,11. Blood flow on color Doppler ultrasound may be interrupted in most of the cases described, but evidence of marginal flow may be found in some cases due to mural arteriovenous shunts12. The diagnosis of thrombosis is usually established around 26 to 30 weeks of gestation9.
Fetal MRI can be used as a complementary diagnostic modality in the prenatal period, as it confirms the diagnosis, provides more precise anatomical information, allows characterization of the lesion and evaluation of parenchymal brain alterations2,3. The images also offer detailed resolution of the posterior fossa, cerebellum and dural venous structures9. Diagnosticfindings include extra-axial lesion in the torcula of Herophilus that is isointense/hypointense compared to the gray matter, with or without eccentric focal areas of increased hypointensity on T2-weighted images8. However, the thrombus may become hyperintense during the subacute period. Another advantage is that any tumor structure, blood products, mass effect and solid components can be detected. Some factors such as cerebral and intraventricular hemorrhage, mass effect in neighboring structures, prematurity, ventriculomegaly and schizencephaly are considered of poor prognosis in these cases3,5,9.
Differential diagnoses include those causes of cystic lesions in the posterior fossa, such as Dandy-Walker malformation, arachnoid cyst or aneurysm of the vein of Galen13. Dandy-Walker malformation and arachnoid cyst are differentiated from thrombosis of the torcula of Herophilus by thin-walled anechoic images, absence of blood flow on color Doppler and signal intensity similar to cerebrospinal fluid10. Vein of Galen aneurysm can be differentiated by location, since it usually affects the region of the choroidal fissure and extends from the foramen interventricularis to the pineal gland3. Other differential diagnoses that should be considered are intracranialnposterior fossa tumors -such as teratoma or lipoma-, intracranial hemorrhage with involvement of the cerebellum or occipital lobes, and thrombosis of a vein of Galen malformation10.
Prenatal counseling can be difficult due to the variability of the perinatal outcome. In the majority of cases (75%), thrombosis of the torcula of Herophilus remits spontaneously without perinatal complications3. However, in the minority of cases it may cause ischemic brain damage secondary to cerebral hypoperfusion due to retrograde venous hypertension and mass effect compression, which may be associated with a worse long-term neurodevelopmental outcome. Venous congestion due to inadequate venous drainage may leadmto prolapse of the cerebellar tonsils through the foramen magnum5. Perinatal complications are more common in preterm neonates and in cases associated with secondary cerebral sinus thrombosis or ventricular hemorrhage4.
Several hypotheses have been proposed to explain the favorable perinatal outcome and the absence of associated symptoms. The anasto moses between the different cerebral venous territories are numerous and communicate the deep and superficial cerebral veins, thus allowing redirection of venous flow in case of obstruction of one of the outlets. In addition, the torcula of Herophilus forms a variable system of anastomotic channels between the straight and superior sagittal sinuses with the lateral sinuses. These features would allow normal outflow in case of partial obstruction. On the other hand, the partial or complete dural partition of the superior sagittal sinus allows that, while one channel is obstructed, another one drains correctly5,12,14. On the other hand, arteriovenous shunts in this malformation are generally of low velocity and rarely cause systemic hemodynamic complications15. Prognosis depends on the absence of predisposing conditions and normal MRI evaluation of the brain parenchyma7.
In conclusion, thrombosis of the torcula of Herophilus is a rare condition with a good prognosis. Its etiology is unknown. The sonographic appearance is of a triangular anechoic lesion with an echogenic mass inside in the occipital region. Although the vast majority of cases show spontaneous prenatal regression, clinically significant complications may occur. It is necessary to know that there is a high possibility of a favorable perinatal outcome.
REFERENCES
1. Corral E, Stecher X, Malinger G, Ochoa JH, de Catte L, Sepulveda W. Thrombosis of the torcular herophili in the fetus: a series of eight cases. Prenat Diagn. 2014;34(12):1176-81. doi: 10.1002/pd.4453 [ Links ]
2. Rayssiguier R, Dumont C, Flunker S, Couture A, Boulot P, Prodhomme O. Thrombosis of torcular herophili: diagnosis, prenatal management, and outcome. Prenat Diagn. 2014;34(12):1168-75. doi: 10.1002/pd.4448 [ Links ]
3. Has R, Esmer AC, Kalelioglu I, Yuksel A, Pata O, Demirbas R. Prenatal diagnosis of torcular herophili thrombosis: report of 2 cases and review of the literature. J Ultrasound Med. 2013;32(12):2205-11. doi: 10.7863/ultra.32.12.2205 [ Links ]
4. Yang Q, Duan J, Fan Z, Qu X, Xie Y, Nguyen C, et al. Early detection and quantification of cerebral venous thrombosis by magnetic resonance black-blood thrombus imaging. stroke. 2016;47(2):404-9. doi: 10.1161/STROKEAHA.115.011369 [ Links ]
5. Gao J, Liu J, Zhou X, Bian X, Dai Q, Feng F, et al. Spontaneous resolution of a fetal dural sinus thrombosis: one case report and review of the literatures. Int J Fertil Steril. 2012;5(4):259-62. [ Links ]
6. Rosenblum JS, Tunacao JM, Chandrashekhar V, Jha A, Neto M, Weiss C, et al. Tentorial venous anatomy: Variation in the healthy population. AJNR Am J Neuroradiol. 2020 Oct;41(10):1825-32. doi: 10.3174/ajnr.A6775 [ Links ]
7. Komiyama M, Nishikawa M, Kitano S, Sakamoto H, Miyagi N, Kusuda S, et al. Transumbilical embolization of a congenital dural arteriovenous fistula at the torcular herophili in a neonate. Case report. J Neurosurg. 1999;90(5):964-9. doi: 10.3171/jns.1999.90.5.0964 [ Links ]
8. Fanou EM, Reeves MJ, Howe DT, Joy H, Morris S, Russell S, et al. In utero magnetic resonance imaging for diagnosis of dural venous sinus ectasia with thrombosis in the fetus. Pediatr Radiol. 2013;43(12):1591-8. doi: 10.1007/s00247- 013-2745-7 [ Links ]
9. Xia W, Hu D, Xiao P, Yang W, Chen X. Dural sinus malformation imaging in the fetus: based on 4 cases and literature review. J Stroke Cerebrovasc Dis. 2018;27(4):1068-76. doi: 10.1016/j.jstrokecerebrovasdis.2017.11.014 [ Links ]
10. Laurichesse Delmas H, Winer N, Gallot D, Lopes K, Perrotin F, Fluncker S, et al. Prenatal diagnosis of thrombosis of the dural sinuses: report of six cases, review of the literature and suggested management. Ultrasound Obstet Gynecol. 2008;32(2):188-98. doi: 10.1002/uog.5348 [ Links ]
11. Beresford C, Hall S, Smedley A, Mathad N, Waters R, Chakraborty A, et al. Prenatal diagnosis of arachnoid cysts: a case series and systematic review. Childs Nerv Syst. 2020;36(4):729-741. doi: 10.1007/s00381-019-04477-6 [ Links ]
12. Legendre G, Picone O, Levaillant JM, Delavaucoupet J, Ozanne A, Frydman R, et al. Prenatal diagnosis of a spontaneous dural sinus thrombosis. Prenat Diagn. 2009;29(8):808- 13. doi: 10.1002/pd.2277 [ Links ]
13. Byrd SE, Abramowicz JS, Kent P, Kimura RE, Elias D, Heydeman PT. Fetal MR imaging of posterior intracranial dural sinus thrombosis: a report of three cases with variable outcomes. Pediatr Radiol. 2012;42(5):536-43. doi: 10.1007/s00247-011-2287-9 [ Links ]
14. Matsuda W, Sonomura T, Honma S, Ohno S, Goto T, Hirai S, et al. Anatomical variations of the torcular Herophili: macroscopic study and clinical aspects. Anat Sci Int. 2018;93(4):464-468. doi: 10.1007/s12565-018-0436-z [ Links ]
15. Liby P, Lomachinsky V, Petrak B, Kyncl M, Charvat F, Padr R, et al. Torcular dural sinus malformations: a single-center case series and a review of literature. Childs Nerv Syst. 2020;36(2):333-341. doi: 10.1007/s00381-019-04280-3 [ Links ]
Ethical responsibilities: Protection of persons. We, the authors, declare that the procedures followed conformed to the ethical standards of the committee on responsible human experimentation and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality: The authors declare that we have followed the protocols of the Hospital Central "Dr. Urquinaona" on the publication of patient data.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Funding: The authors certify that we have not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the conduct of the study.
Received: March 18, 2021; Accepted: June 02, 2021











 texto en
texto en 



