Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.4 Lima oct./dic 2021
http://dx.doi.org/10.31403/rpgo.v67i2376
Case Report
Neonatal hydrometrocolpos: a clinical case of difficult diagnosis
1Departamento de Obstetricia y Neonatología, Clínica Santa Isabel, Lima, Perú
The diagnosis of fetal malformations continues to be a challenge for the obstetriciangynecologist, despite advances in fetal medicine and ultrasonographic technology. Hydrometrocolpos is a dilatation of the uterus and vagina due to accumulation of secretions, product of genital obstruction usually associated with congenital malformations. We present the case of a female newborn with congenital hydrometrocolpos, whose diagnostic suspicion in pelvic studies was ovarian cysts, but it was due to the increase of bilateral hydronephrosis. At birth, it was decided to surgically decompress the urinary tract, at which time hydrometrocolpos associated with imperforate hymen was found.
Key words: Uterus; Hymen
INTRODUCCIÓN
The development of the female genital apparatus begins in the fifth week after fertilization from the Müllerian ducts, in a cranio-caudal direction, with the fusion of what will constitute the uterus and keeping separate the portions that will give rise to the fallopian tubes1. The hymen represents the union of the bulbs of the vaginal sinus with the urogenital sinus, which is usually perforated in embryonic life and, when it does not occur, can lead to vaginal malformations2.
Congenital malformations of the uterus occur in 0.5% of the population and vaginal malformations in 0.025%. Hydrometrocolpos or hydrocolpos is a rare condition, with an incidence of 1/16.000 female births. It consists of dilatation of the uterus and vagina due to accumulation of secretions resulting from glandular hypersecretion stimulated by maternal hormones, which is associated with obstructive congenital malformations, such as imperforate hymen, septum or vaginal atresia, due to anomalies of the urogenital sinus or cloaca1,2. Many cases are newly discovered in adolescence1. We present the case of a newborn with congenital hydrometrocolpos.
CLINICAL CASE
We present the case of a female newborn born of normal vaginal delivery at 39 weeks, weighing 3,575 grams, Apgar 9 at one minute and 9 at 5 minutes. The clinical course of the pregnancy was uneventful, with a single umbilical artery and mild left pyelectasis of 9 mm at 24 weeks; no additional pelvic lesion was described. In a subsequent ultrasound at 34 weeks, a 36 mm intrapelvic echolucent image was described, with an inner papilla and scarce peripheral vascularization on Doppler, which was classified as an ovarian cyst. In an ultrasound control by another observer one week later, the image of the same size and bilateral moderate pyelectasis of 11 and 12 mm was described.
At 36 weeks, a third evaluator mentioned similar characteristics and reported it as ovarian cyst versus renal cyst. It was assumed that the pyelectasia could be secondary to tumor compression and, as the fetus remained stable, it was decided to wait for delivery. On further evaluation, vaginal delivery was considered due to previous normal vaginal delivery and good fetal health conditions.
After birth, an ultrasound of the newborn's abdomen correlated with intrauterine findings of an ovarian cyst with irregular borders and intracystic papilla (Figure 1). However, CA 125 and alpha-fetoprotein levels were elevated: CA 125 112 U/mL (reference value less than 35) and AFP 17 928 ng/mL (reference value 0 to 7). Renal evaluation determined moderate bilateral pyelectasis (Figure 2).
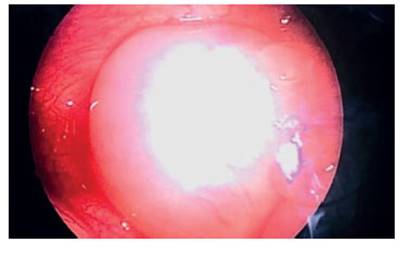
Due to the findings described above, it was decided to perform surgery to solve the tumor problem and renal decompression by means of a laparoscopic approach. The finding was a very distended uterus without the presence of the referred cyst (Figure 3), so the intervention was converted to a mini-laparotomy, which found the hydrometrocolpos. The uterus was punctured and mucoid material was obtained, which allowed its decompression (Figure 4).
At the end of the operation, the vaginal study was completed, with the finding of imperforate hymen. The evolution was clinically satisfactory, with remission of pyelectasia in the ultrasound control at 5 postoperative days.
DISCUSSION
The first case of hydrometrocolpos was published in 1856, by Godefroy, who described it associated with urinary and intestinal obstruction3.
Imperforate hymen corresponds to 0.1% of girls born at term4, but it is rarely associated with hydrocolpos or hydrometrocolpos, closely related to estrogen levels, which usually remain low in the perinatal period and infancy, responsible for the production of mucus from the cervical glands; this only increases in adolescence, when it is diagnosed2,4-7. Additionally, hydrometrocolpos has been described due to urine accumulation secondary to vesico-vaginal fistulas4. Many times, the finding is associated with fluid protrusion through the obstructed vaginal introitus.
The most common neonatal diagnosis is congenital ovarian cyst 3,8 and, although ultrasound is the diagnostic tool of choice, images can be inconclusive, sometimes requiring the request of an MRI. Pelvic cystic images may correspond to gynecological (hydrometrocolpos, hydrocolpos, ovarian cyst, ovarian torsion), urinary (megacystis) or intestinal (imperforate anus, gastrointestinal duplication) malformations2,3,5.
Imperforate hymen causes 50% of vaginal obstructions4 and is associated with duplication of the ureter, polydactyly, imperforate anus, renal dysplasia, ectopic ureter and other malformations7.
The compressive effect is often associated with hydronephrosis and rectal obstruction for defecation, and even compression of the inferior vena cava. Any pelvic tumor in a newborn should lead to a detailed genital inspection6,8. An attempt has been made to look for a suspicious sign of hydrometrocolpos, “The Fjord sign” in Norwegian, which is described as a narrow channel separating the dilated vagina from the uterus5 and which would be differential diagnosis of ovarian cysts.
Hydrometrocolpos is sometimes associated with an autosomal recessive disorder, called Mckusick-Kaufman syndrome3.
Because of its low incidence, it is difficult to find worldwide series. Okoro reported 7 cases in Nigeria, from 7 to 27 days of life, associated with other malformations. Some patients underwent laparotomy and some underwent hymenotomy. Thirty percent of the cases were diagnosed intraoperatively, due to the low index of suspicion7.
As a final suggestion, every newborn should have a thorough vulvovaginal evaluation, especially if a congenital malformation of the genitourinary system is found.
REFERENCES
1. Sarmiento Y, Crespo A, Sánchez I, Menéndez Y. Hidrocolpos neonatal. Rev Cubana Pediatr. Dic 2009;81(4):93-7. [ Links ]
2. Yildirim G, Gungorduk K, Aslan H, Sudoimus S, Ark C, Saygin S. Prenatal diagnosis of imperforate hymen with hydrometrocolpos. Arch Gynecol Obstet. 2008;278:483-5. doi.org/10.1107/s00404-008-0603-x [ Links ]
3. Ekenze S, Ezegwui H. Hydrometrocolpos from a low vaginal atresia: An uncommon cause of neonatal intestinal and urinary obstruction. Afr J Paediatr Surg. 2008;5(1):43-5. doi:10.4103/0189-6725.41637 [ Links ]
4. Madero G, Echeverry LM, Jiménez YL. Diagnóstico neonatal de hidrometrocolpos. 2015;48(3):75-9. doi:10.1016/rcpe.2015.10.002 [ Links ]
5. Schumacher R, Brzezinska R. Hydrometrocolpos: The Fjord Sign. Ultraschall in der Medizin-European Journal of Ultrasound. 2007;28(05):518-20. doi:10.1055/s-2007-963211 [ Links ]
6. Garfias C, Barrera A, Zubieta R, Ugarte F. Caso clínico: Hidrocolpos e hidrometrocolpos neonatal: a propósito de un caso clínico. Rev Chil Pediatr. 2011;82(2):137-41. doi:10.4067/S0370-41062011000200008 [ Links ]
7. Okoro P, Obiorah C, Enyindah CE. Experience with neonatal hydrometrocolpos in the Niger Delta area of Nigeria: Upsurge or increased recognition? Afr J Paediatr Surg. 2016 Oct-Dec;13(4):161-5. [ Links ]
8. Messina M, Severi F, Bochi C, Ferrucci E, Di Maggio G, Petroglia F. Voluminous perinatal pelvic mass: a case of congenital hydrometrocolpos. J Maternal-Fetal Neonatal Med. 2004;15:135-7. doi:10.1080/14767050410001659888 [ Links ]
Authorship contributions: We, the authors, declare that we have made significant contributions to the conception and design of the manuscript, collection of data, drafting and critical revision of the content of the manuscript, final approval of the version to be published, and assume responsibility for all aspects of the manuscript. The manuscript has not been previously published
Rights to confidentiality and informed consent: They were granted by the patient after being adequately informed of the purpose of the manuscript
Received: April 19, 2021; Accepted: June 02, 2021











 texto en
texto en