Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.67 no.4 Lima Oct./Dec. 2021
http://dx.doi.org/10.31403/rpgo.v67i2377
Case Report
Prenatal diagnosis of intra-abdominal varicose vein of the fetal umbilical vein
1. Obstetrics and Gynecology Service, Hospital Central "Dr. Urquinaona , Maracaibo. Zulia, Venezuela
Intra-abdominal varices of the fetal umbilical vein are rare entities characterized by focal aneurysmal dilatation. They account for approximately 4% of umbilical cord anomalies and are thought to represent a developmental anomaly rather than a congenital malformation. Their clinical significance has not yet been clearly established. Prenatal diagnosis is made by conventional ultrasonography, in which the lesion appears as a round or fusiform cystic structure within the fetal abdomen. In addition, it is useful to establish the diameter and the presence of other associated fetal anomalies. Doppler evaluation allows identification of the type of intralesional flow. The perinatal prognosis is favorable when it is identified as an isolated finding. However, in those cases associated with other anatomical/structural alterations, the fetal and neonatal outcome is variable. We present a case of prenatal diagnosis of intra-abdominal varicose vein of the fetal umbilical vein.
Key words: Fetus; Umbilical cord; Umbilical veins; Ultrasonography; Prenatal diagnosis
Introduction
Intra-abdominal varices of the fetal umbilical vein are represented by focal aneurysmal dilatation from its entry into the abdominal wall to its outflow into the fetal portal system1. Although they are uncommon (they represent only 4% of umbilical cord malformations), they are easily detectable due to technical advances in imaging techniques (conventional ultrasound and color Doppler)2. The significance and importance of this vascular malformation on fetal and neonatal outcome are currently unknown. Although cases detected in isolation have a reasonably favorable perinatal outcome, different studies associate its presence with chromosomal, anatomical or structural anomalies and increased frequency of adverse perinatal outcomes2,3. We present a case of prenatal diagnosis of intra-abdominal varicose vein of the fetal umbilical vein.
Case presentation
The patient was 21 years old, primigravida, 28 weeks pregnant, referred to the high-risk prenatal clinic for presenting intrauterine growth restriction of the fetus in the routine ultrasound control. She reported an uncomplicated pregnancy course. In the ultrasound evaluations at 11 and 20 weeks there were no alterations in the volume of amniotic fluid or fetal growth. The pregnancy was achieved spontaneously and the result of the first trimester aneuploidy evaluation was low risk. She denied any significant personal or family history, as well as tobacco, alcohol or illicit drug use. The results of the biochemical, hormonal and functional panel were normal.
The ultrasound showed a female fetus of 29 weeks gestation by ultrasound measurements, but with fetal growth below the 10th percentile for gestational age. Fetal movements, amniotic fluid volume and Doppler parameters of the uterine, umbilical and middle cerebral fetal arteries were normal. An ovoid-shaped structure measuring 26 x 12 millimeters was found inside the abdomen near the anterior abdominal wall. The intralesional blood flow was turbulent, with no evidence of thrombus within it (Figure 1). The umbilical artery was normal, with no evidence of reverse or absent flow. No other anatomic abnormalities or venous tortuosities were noted inside or outside the abdomen. Fetal echocardiography was normal. Both cardiac and umbilicoportal venous connections had normal appearances. The ductus venosus was present with normal Doppler wave. The anatomic distribution of stomach and gallbladder were also preserved. No signs of hydrops fetalis or other structural alterations were found. The final diagnosis was intra-abdominal variceal fetal umbilical vein. The patient refused to undergo any procedure for genetic evaluation.
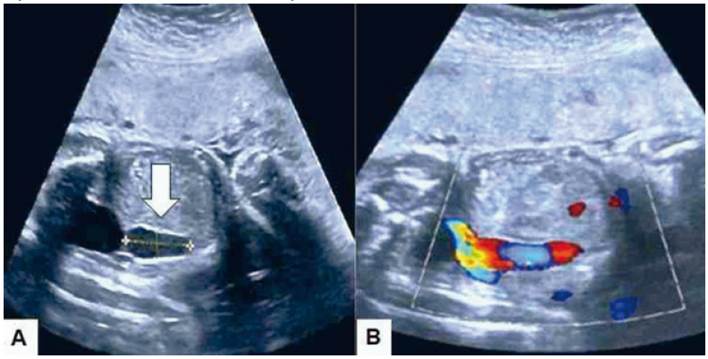
Figure 1 Ultrasound image of the fetal abdomen at 29 weeks. a) Arrow points to rounded lesion compatible with intra-abdominal varicose vein of the fetal umbilical vein measuring 26 x 12 millimeters located near the abdominal wall. b) Doppler flow image showing vascular flow within the lesion with continuity of flow with the fetal umbilical vein.
Follow-up ultrasound evaluations during the third trimester showed no change in variceal size, but growth remained below the 10th percentile for gestational age, with Doppler values, as well as amniotic fluid volume, within normal limits. The new fetal echocardiographic evaluation at 35 weeks showed no pathological alterations.
At 37 weeks, the patient presented evidence of acute fetal distress and underwent emergency cesarean section, resulting in a live female newborn weighing 2,300 grams, with Apgar scores of 7 and 9 at one minute and 5 minutes, respectively. Postnatal physical examination revealed no obvious anatomical alterations. Ultrasound evaluation of the vascular lesion showed de creased size, confirming the diagnosis of intraabdominal variceal umbilical vein. Echocardiography was normal. Karyotyping could not be performed. In the evaluation at 6 months, the infant presented adequate growth and development for her age.
Discussion
The left umbilical vein enters the fetus through the umbilical ring and runs along the inferior border of the fetal liver, joining the portal system, forming the portoumbilical system. Subsequently, the blood passes into the inferior vena cava through the ductus venosus4. In the period between 20 and 40 weeks of gestation, the mean diameter within the umbilical ring increases from 2.8 to 5.9 millimeters, while the mean flow velocity varies between 20 and 41 cm/s5,6.
Fetal umbilical vein varices have an unknown exact incidence, but the literature describes a prevalence of approximately 1.1 to 2.8 / 1,000 live births3,7. Several etiologies have been proposed for its occurrence, among which are degenerative changes, syphilis, decreased vascular resistance and congenital thinning of the vessel near the lower abdominal wall6. The latter is the most likely cause in most cases.
Among the types of intra-abdominal umbilical vein varices, extrahepatic varices are more frequent than intrahepatic varices. This is probably due to the fact that this portion has a weak support structure, without support from the hepatic parenchyma, which allows the increase of venous pressure, secondary to the jet flow from the constriction site, and produces segmental dilatation of the vessel3.
Intra-abdominal varicose vein of the fetal umbilical vein appears on ultrasound imaging as a rounded or fusiform cystic structure, anechoic and fluid-filled, oriented obliquely cephalo-caudally, between the anterior abdominal wall and the lower border of the liver. The diameter of most lesions varies from 6 to 12 standard deviations above the average umbilical vein diameter for the corresponding gestational age8. However, there is one report of a lesion measuring 85 millimeters9.
Diagnostic criteria for intra-abdominal variceal fetal umbilical vein include: 1) varicose vein diameter greater than 9 millimeters, 2) the index portion of the fetal umbilical vein is 50% wider compared to the undilated portion, or 3) index portion greater than two standard deviations above the mean value for gestational age and with vascular flow within the lesion3.
Other differential diagnoses are abdominal cystic lesions, such as distended gallbladder, mesenteric cyst or enteric duplication. Color Doppler evaluation detects the venous flow in its interior and allows differentiating it from other sonolucent structures, such as common bile duct cyst or urachus10. In addition, the spectral tracing also contributes to confirm the pattern of venous flow within the lesion2.
The fetal alterations most commonly related to this condition are hydrops, anemia, diaphragmatic hernia, limb shortening, hydrocephalus, oligohydramnios, polyhydramnios, intrauterine growth retardation, pulmonary sequestration, ventriculomegaly and echogenic bowel. The frequency of association is close to 10% when there are no chromosomal abnormalities3. Aneuploidies (trisomies 9, 18 and 21), as well as triploidies, may also be associated with the development of the lesion. All these conditions justify further evaluation by neonatal karyotyping10-12.
Although intra-abdominal varices of the fetal umbilical vein are rare, they are associated with a high mortality rate and their clinical course should be considered. The most frequent complications described are rupture, thrombosis, umbilical artery compression and fetal heart failure due to vascular steal and increased preload. The mortality rate for rupture and thrombosis is 50% and 80%, respectively12-14. Perinatal outcome depends on gestational age at detection, associated malformations and intralesional flow characteristics. The larger the diameter of the lesion, the greater the risk of thrombosis2. In addition, bidirectional turbulent flow in the dilated segment has been described in approximately 50% of cases4,15.
The greatest likelihood of fetal death occurs between 27 and 30 weeks of gestation, due to increased blood flow in the fetus. Early onset of vascular malformation (before 26 weeks) warrants close monitoring for abnormalities in growth and fetal flow rates, as the risk of adverse outcome is higher. Cases diagnosed during the third trimester probably have lower mortality rates10.
Pregnant women diagnosed with intra-abdominal varices of the fetal umbilical vein should undergo ultrasound evaluation and Doppler monitoring more frequently than usual and be informed of potential complications11,14. Induction of labor may be attempted at 34 to 36 weeks gestation, once fetal lung maturity has been confirmed. The route of termination of pregnancy depends on obstetric causes, since the vaginal route is not contraindicated in these cases11.
We will conclude by pointing out that the diagnosis of intra-abdominal varices of the fetal umbilical vein requires careful obstetric evaluation. In the absence of malformations or chromosomal alterations, the prognosis is generally favorable, but the perinatal outcome is variable. Termination of pregnancy after reaching fetal lung maturity may be necessary in those cases with enlargement of the lesion and evidence of turbulent flow to avoid complications associated with rupture. It is also necessary to rule out the possibility of other fetal conditions, due to their high perinatal mortality rate.
REFERENCES
1. Virdis G, Gulotta A, Cherchi C, Spanedda G, Olzai MG, Ambrosini G, et al. Umbilical intra-abdominal vein varix: a case report and review of the literature. Clin Exp Obstet Gynecol. 2016;43(2):268-70. PMID: 27132426 [ Links ]
2. Gowda S, Chakkalakkoombil SV, Bharathi S, Barathi D. Large fetal intra-abdominal umbilical vein varix: Antenatal sonographic diagnosis and follow-up. J Obstet Gynaecol Res. 2019;45(9):1936-40. doi: 10.1111/jog.14045 [ Links ]
3. Shah KH, Nambiyar R, Bhat S. Prenatal diagnosis and management of fetal intra-abdominal umbilical vein varix. J Family Med Prim Care. 2018;7(2):458-60. doi: 10.4103/jfmpc.jfmpc_76_17 [ Links ]
4. di Pasquo E, Kuleva M, O'Gorman N, Ville Y, Salomon LJ. Fetal intra-abdominal umbilical vein varix: retrospective cohort study and systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2018;51(5):580-5. doi: 10.1002/uog.18895 [ Links ]
5. Hasegawa J, Mimura T, Morimoto T, Matsuoka R, Ichizuka K, Sekizawa A, et al. Detection of umbilical venous constriction by Doppler flow measurement at midgestation. Ultrasound Obstet Gynecol. 2010;36(2):196-201. doi: 10.1002/uog.7695 [ Links ]
6. Flo K, Wilsgaard T, Acharya G. Agreement between umbilical vein volume blood flow measurements obtained at the intra-abdominal portion and free loop of the umbilical cord. Ultrasound Obstet Gynecol. 2009;34(2):171-6. doi: 10.1002/uog.6441 [ Links ]
7. Rosenblatt J, Loberstajn A, Coulomb A, Stos B, Garel C, Abarah B, et al. Intra-abdominal umbilical vein varix associated with fetal cardiac failure: a pitfall to the prenatal diagnosis of a-zero-thalassemia. Fetal Diagn Ther. 2013;34(1):59- 62. doi: 10.1159/000345784 [ Links ]
8. Lei T, Xie HN, Feng JL. Prenatal diagnosis of four-vessel umbilical cord with supernumerary vein varix: A case report and literature review. J Obstet Gynaecol Res. 2017;43(7):1200-4. doi: 10.1111/jog.13324 [ Links ]
9. Fuster JS, Benasco C, Saad I. Giant dilatation of the umbilical vein. J Clin Ultrasound. 1985;13(5):363-5. doi: 10.1002/jcu.1870130516 [ Links ]
10. Sanapo L, Burul G, Saccardi C, Nardelli GB, D'Antona D. Four cases of fetal intra-abdominal umbilical vein varix: a single centre's approach to management. J Obstet Gynaecol. 2013;33(4):375-7. doi: 10.3109/01443615.2013.771157 [ Links ]
11. Ismail H, Chang YL, Chang SD, Nusee Z. Fetal intra-abdominal umbilical vein varix in monochorionic twins: is it significant? Malays J Med Sci. 2012;19(3):69-73. PMID: 23785250 PMCID: PMC3684235 [ Links ]
12. Rahemtullah A, Lieberman E, Benson C, Norton ME. Outcome of pregnancy after prenatal diagnosis of umbilical vein varix. J Ultrasound Med. 2001;20(2):135-9. doi: 10.7863/jum.2001.20.2.135 [ Links ]
13. Melcer Y, Ben-Ami I, Wiener Y, Livne A, Herman A, Maymon R. Long-term outcomes of children with umbilical vein varix diagnosed prenatally. Prenat Diagn. 2013;33(5):492-6. doi: 10.1002/pd.4098 [ Links ]
14. Ipek A, Kurt A, Tosun O, Gümüs M, Yazicioglu KR, Asik E, et al. Prenatal diagnosis of fetal intra-abdominal umbilical vein varix: report of 2 cases. J Clin Ultrasound. 2008;36(1):48-50. doi: 10.1002/jcu.20334 [ Links ]
15. Pamplona-Bueno L, Padilla-Iserte P, Ferri-Folch B, Juárez- Pallarés I, Gómez-Portero R, Perales-Marín A. Fetal intraabdominal umbilical vein varix: a case report and literature review. J Obstet Gynaecol India. 2015;65(6):420-2. doi: 10.1007/s13224-015-0694-9 [ Links ]
Declaration of ethical aspects
Ethical responsibilities: Protection of persons. The authors declare that the procedures followed conformed to the ethical standards of the committee on responsible human experimentation and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality: We, the authors, declare that we have followed the protocols of the Central Hospital "Dr. Urquinaona" on the publication of patient data
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Financing: The authors certify that we have not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the conduct of the study.
Received: March 18, 2021; Accepted: June 15, 2021











 text in
text in 



