Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.1 Lima ene./mar. 2022 Epub 24-Feb-2022
http://dx.doi.org/10.31403/rpgo.v68i2396
Original Articles
Maternal and perinatal mortality in municipalities and townships of the land border. Colombia 1998 - 2016
1. Health Systems Manager. Research assistant of the Health Systems Line SISSALUD, Antioquia, Colombia
2. Doctor in Public Health, Professor National Faculty of Public Health, University of Antioquia, Colombia
3. Doctor in Public Health, Fellowhisp (FFPH) Imperial College of London, Professor National Faculty of Public Health, University of Antioquia, Colombia. Coordinator of the Health Systems research line assigned to the Management and Public Policy Research Group, National Faculty of Public Health, Chagualo, Medellín, Colombia
Abstract:
Maternal and perinatal mortality is a priority public health issue that is particularly difficult to control in border areas.
Objectives:
To describe the behavior of maternal and perinatal mortality in the border territories of Colombia, between 1998 and 2016; and to establish its association with sociodemographic, geographic and health care factors.
Methods:
Retrospective observational study, based on official records. Maternal mortality ratio (MMR) and perinatal mortality ratio (RMP) were calculated for the period 1998-2016, identifying inflection points through Joinpoint analysis. Likewise, bivariate and multivariate analyses were performed.
Results:
From 54 municipalities and 12 borders townships belonging to 12 Departments, 687 records maternal mortality records and 12,786 perinatal mortality records were obtained. The ratios observed were 88 x 100,000 BA for MMR and 16 x 1,000 NV for PMR. The trend of these types of mortality was downward. The highest values of perinatal mortality were significantly associated with maternal age 35-54 years, care by subsidized regime, low educational level, women without a partner, and multiple pregnancies.
Conclusion:
Maternal and perinatal mortality registered in border municipalities is above the national average.
Key words: Maternal mortality; Perinatal mortality; Maternal health; Maternal and Perinatal health services; Vulnerable populations
Introduction
Diseases related to pregnancy, childbirth and puerperium are the leading causes of mortality in women of reproductive age1. Maternal death is defined as 'the death of a woman while pregnant or within 42 days of termination of pregnancy, regardless of the duration and site of pregnancy, due to any cause related to or aggravated by the pregnancy itself or its care, but not due to accidental or incidental causes'2. It is calculated using the maternal mortality ratio (MMR) expressed as deaths per 100,000 live births. According to the World Health Organization (WHO), 830 women die every day worldwide from complications related to pregnancy or childbirth. In 2015, 303,000 MM deaths were estimated, mostly in low-income countries, many of which could have been prevented with adequate controls3.
Perinatal death is defined as death occurring 'during the perinatal period, which begins at 22 completed weeks of gestation and ends seven completed days after birth'4.
Maternal and perinatal mortality continue to be a major public health problem in the world. These events are not only individual issues, as they affect the mother-child dyad, the nuclear family and society as a whole5; and they are considered unacceptable, since many of these deaths can be avoided by improving health services.
Maternal and perinatal mortality shows differential patterns in the different territories6, indicating unjust and ethically unacceptable inequalities, which may be greater in border areas, where population mobility and health infrastructure may make control difficult.
In the Colombian municipalities that share land borders with the five neighboring countries -Venezuela, Brazil, Ecuador, Panama and Peru- there are marginalized populations of different peoples and cultures, with important social problems, rural and dispersed populations7. The municipalities and townships in these areas tend to belong to the lowest socioeconomic categories, whose sanitation and road infrastructure and resources are also limited8.
There are 54 border municipalities and 12 border townships in the country, belonging to 12 departments of Colombia. Arauca, Chocó, Vaupés and Putumayo each have 4 border municipalities or townships; Amazonas and Cesar each have 7 border municipalities or townships; Nariño and Guainía each have 6 border municipalities or townships; Boyacá has only 1 border municipality; La Guajira and Norte de Santander each have 10 border municipalities, and Vichada has 3 border municipalities. Of Colombia's 12 border departments, 3 have border townships, including Amazonas with 5 townships, Guainía with 5 townships and Vaupés with 2 townships.
The situation of these municipalities could constitute an obstacle to effective access to health services.
In Colombia, there is no known research on the structure and dynamics of maternal and perinatal mortality in border areas or its association with sociodemographic and health care conditions.
Methods
This is a mortality study based on official records. The population analyzed consisted of all maternal and perinatal deaths registered during the period in the 54 municipalities and 12 townships of Colombia's land borders. Information on live births was obtained from vital statistics databases. Socioeconomic and demographic characteristics were obtained from the Unsatisfied Basic Needs database, officially published by the National Administrative Department of Statistics-NADS9-11. The municipal category was recorded according to the criteria of Law 617 of 200012.
From the official death records published annually by NADS, a new database was extracted, compiled by year and made up of all the records of maternal and perinatal deaths that occurred in the municipalities and townships of the land borders during the selected period.
The explanatory variables included in the study were classified into four categories. Contextual variables: municipal category, multidimensional poverty index-MPI and unsatisfied basic needs. Clinical variables: maternal mortality ratio-MMR, fetal mortality ratio-FMR and perinatal mortality ratio-PMR, basic cause and direct cause. Sociodemographic variables: area where the death occurred, area of usual residence, country of usual residence, social security system, marital status of the mother, educational level of the mother, age and ethnicity in the case of maternal deaths. Variables related to health care: place where death occurred and medical care. Mortality trends was analyzed by means of the joinpoint regression technique.
A logistic regression model was applied to establish the association between perinatal deaths and explanatory variables of a sociodemographic nature and birth characteristics. The response variable was cases of perinatal deaths and the control group was live births. The variables were included in the model according to the Hosmer-Lemeshow criterion if the value was p<0.25. The population studied corresponded to 12,786 perinatal deaths (PM) and 781,140 live births. The logistic regression model was performed according to the recommendations of Fernandez et al13. A multivariate analysis was not performed for maternal death (MM), since there was no adequate comparison group.
The power of the study, understood as the 'probability of rejecting the null hypothesis when it is actually false', was calculated a posteriori based on sample size, effect size, and alpha14. The alpha size used was 0.05. Since each analysis yielded a different effect size, the power was calculated for a minimum value of 0.1 with respect to the OR of the insurance scheme15. The power was calculated according to the method proposed by Pértegas and Pita14, obtaining a power of 91.92%. Standard deviation-SD was also calculated.
Data analysis was performed using the IBM SPSS Statistics software version 21.0 licensed by the University of Antioquia and the Joinpoint 4.0.4 software licensed free of charge from the National Cancer Institute of the United States16. The project was approved by the Research Ethics Committee of the Facultad Nacional de Salud Pública (FNSP) according to certificate CI 00411- 2018.
Results
Although maternal and perinatal mortality are strictly monitored in Colombia, 15 (23%) of the municipalities and townships did not report cases of MM and three (5%) of the townships did not report cases of perinatal deaths, in any of the years of the selected time series (1998-2016).
Between 1998 and 2016, 13,270,939 live births and 3,732,051 deaths from all causes were officially registered in Colombia, including 11,636 maternal deaths and 207,251 perinatal deaths. Records were selected from the 54 municipalities and the 12 border townships corresponding to 687 records of maternal deaths and 12,786 perinatal deaths (Figure 1).
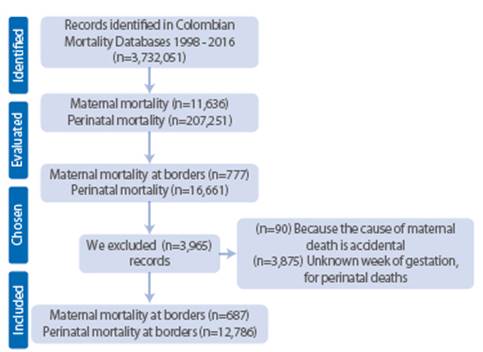
Figure 1 PRISMA diagram of maternal and perinatal mortality records, during the period from 1998 to 2016.
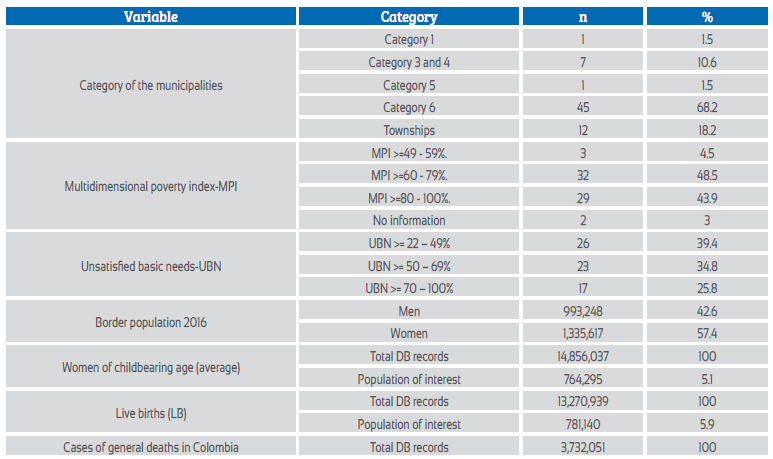
At the time of the study, the regions studied had high poverty rates; 68.2% of the municipalities belonged to the sixth municipal category; 60.6% had more than 50% of unsatisfied basic needs; and 92.4% of their population had a multidimensional poverty index (MPI) above 60%. During the period 1998-2016 it was estimated that there were on average 14,856,037 women of childbearing age (between 10 and 54 years old) in Colombia and of these 764,295 (5.1%) resided in border areas (Table 1).
During the period, the median overall maternal and perinatal mortality ratio in the border municipalities was 88 MM x 100,000 (66.2-118.8; SD=15.1) and 16 MP x 1,000 NV (13.9-21.5; SD=2.6). A median MMR of 103.8 MM x 100,000 NV and a median PMR of 13.8 x 1,000 NV were estimated.
Trend analysis (Figure 2) showed a reduction in MMR and MPR during the study period. The MMR showed an inflection in 2005, with a tendency to decrease the slope of reduction from this year onwards.
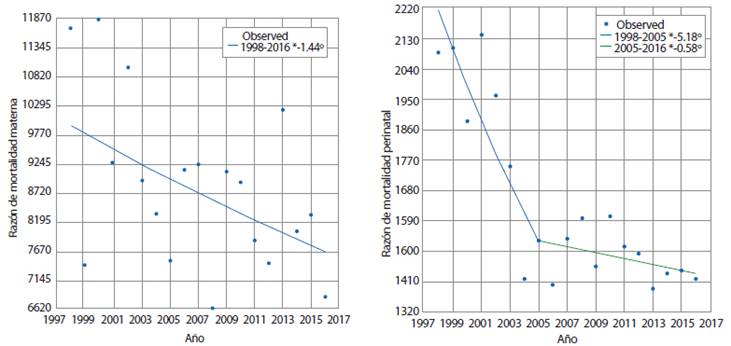
Figure 2 Trends in maternal and perinatal mortality ratios in Colombia's border municipalities 1998-2016. Joinpoint analysis.
Table 2 shows the distribution of maternal and perinatal deaths according to the sociodemographic conditions of the mother. Most of the registered deaths corresponded to women residing in the county seat: MM 337 (49.1%); and PM 8,546 (66.8%). Likewise, most of the deaths also occurred in the county seat: 550 (80.1%) MM and 11,680 (91.3%) PM.
Table 2 Maternal and perinatal mortality according to sociodemographic and health care conditions of mothers in border municipalities of Colombia (1998 - 2016).
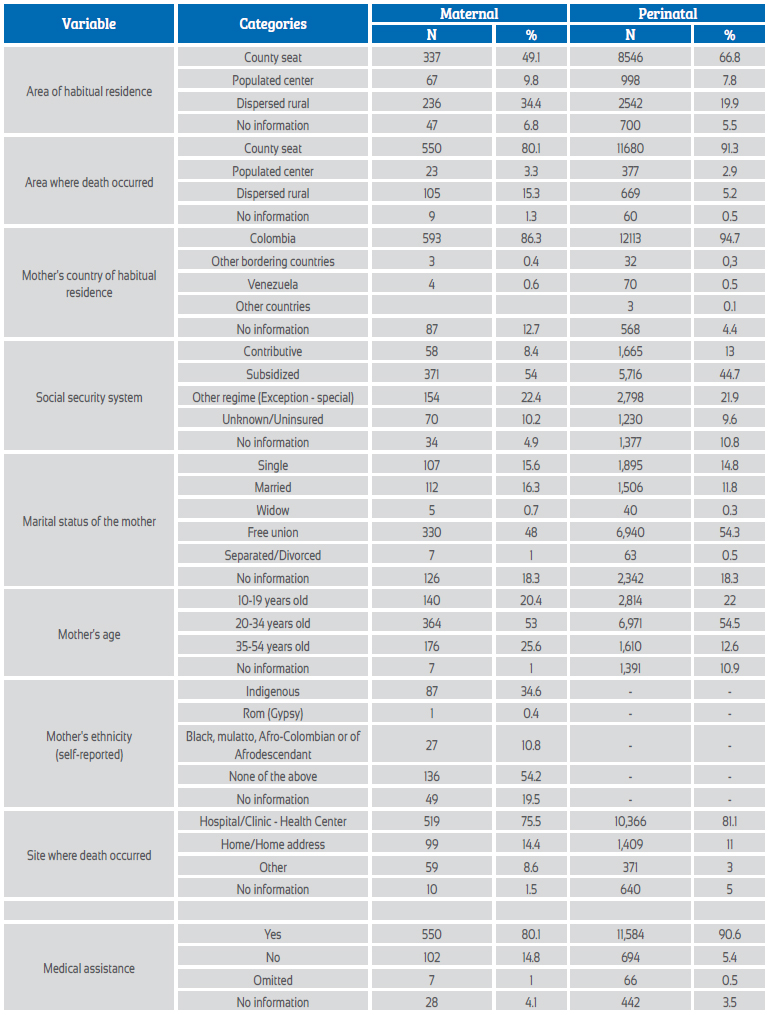
Most of the events corresponded to women who usually resided in Colombia; however, among women coming from neighboring countries, such as Venezuela, Ecuador, Brazil and Peru, there were 7 (1.0%) MM and 102 (0.8%) MP.
The majority of maternal and perinatal deaths (44.7%-54%) were among women affiliated with the subsidized social security system. Between 9.6%-10.2% of the cases corresponded to women who were not insured under a social security system.
Most of the deaths registered were related to women living in free union: 330 (48.0%) of MM; and 6,940 (54.3%) of PM. In the case of the MM, the second marital status with a high number of cases was married women, with 112 (16.3%); while, for the PM, the second marital status with the highest number of cases was single, with 1,895 (14.8%) PM.
The majority of deaths occurred in women aged 20-34 years, 364 (53.0%) of MM and 6,971 (54.5%) of PM. A quarter of the MMs occurred in women aged 35-54 years, while 22.0% of the PMs were recorded in adolescents aged 10-19 years.
For the period 2008-2016, information on the mother by ethnicity was available; in the border zone 136 (54.1%) women belonged to the general population, which in Colombia is predominantly mestizo, and 34.6% to the indigenous ethnic group.
Regarding health care conditions, most of the events obtained institutionalized care in a hospital, clinic, health center or health post: 519 (75.5%) of MM and 10,366 (81.1%) of PM. However, between 11.0 and 14.4% of the events occurred in places such as the home or domicile.
In most of the events recorded, the pregnant woman obtained care during pregnancy complications, 550 women (80.1%) of MM and 11,584 (90.6%) of PM. Between 5.4% and 14.8% of the women with any of the events did not receive health care. It is worth noting that 58.8% of MM that did not receive care corresponded to women in the subsidized regime. Likewise, for women with MM who did not receive medical care, 64.7% resided in dispersed rural areas.
The top ten basic causes of MM in women in the border municipalities of Colombia were identified. These causes accounted for 320 (46.6%) of the deaths and can be divided into three groups: the first group was associated with severe preeclampsia with 64 events (9.3%) and other types of preeclampsia 75 (10.9%). The second group included causes related to hemorrhage, either third-term or immediate hemorrhage, for a total of 73 (10.6%). The third group added diseases of the circulatory system, respiratory system, specified diseases and conditions complicating pregnancy, childbirth and puerperium, and corresponded to 68 (9.9%) MM.
The most frequent cause of perinatal death was respiratory distress syndrome of the newborn, which caused 1,546 (12.1%) deaths, followed by fetal and newborn impairment due to other morphological and functional abnormalities of the placenta and unspecified abnormalities, which caused 1,210 (9.5%) of the deaths.
Multivariate analysis - logistic regression
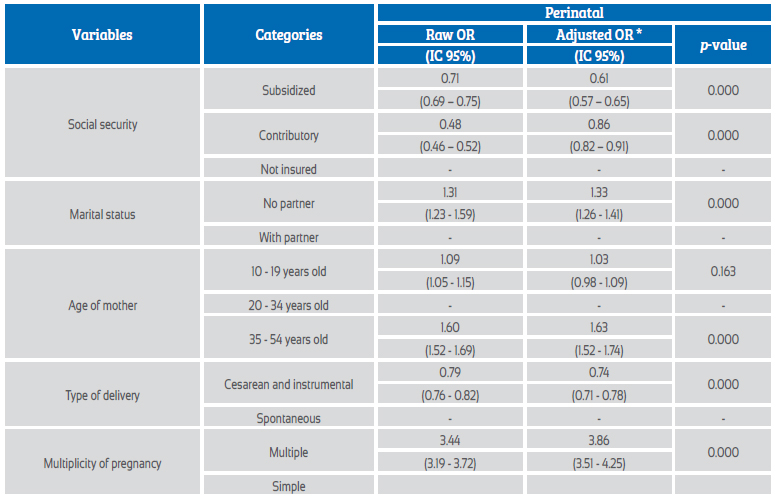
The OR of PM was estimated by multivariate logistic regression. For the social security system, it was found that the OR of the subsidized and contributory systems did not include the value 1, so that neither of the two systems appeared to be a risk factor for perinatal death; the subsidized system presented an OR of 0.62 (95% CI 0.57-0.65) and the contributory system an OR of 0.86 (95% CI 0.82-0.91).
The OR suggests a higher risk for women without a partner, women aged 35 years and older, and women with multiple pregnancies (95% CI 3.4-4.3). See Table 3.
* The ORs were adjusted for social security regime, educational level of the mother, marital status, multiplicity of pregnancy and type of delivery.
Discussion
MM and PM are events of public health interest because they are linked to living conditions, as well as to the characteristics of the provision of health services. Most of them are preventable; therefore, they reflect events of inequities and constitute socially unacceptable phenomena.
One of the most important findings of the present investigation, but at the same time unexpected, was the persistent epidemiological silence for the registration of the two events17 in several localities. In Colombia, MM and PM are notifiable events as a component of the public health epidemiological surveillance system2,4. However, the present investigation identified that, in the case of maternal deaths, several municipalities (23%) did not report cases and for perinatal deaths (5%) of the townships did not do so either.
In the border municipalities, during the period, maternal and perinatal mortality averages were estimated as follows: 88 MM x 100,000 live births and 16 x 1,000 live births for PM. The median MMR identified in the study was higher than the MMR estimated for Colombia in 201418. The median PMR was higher than the PMR reported in Colombia in 201619.
In the country, MMR showed a decrease between 1998 and 2015; this estimator fell from 91.4 x 100,000 live births in 1998 to 51.4 x 100,000 live births in 201520. The MMR has also been decreasing worldwide, from 380 deaths x 100,000 live births in 1990 to 216 x 100,000 in 201521,22. In the Latin American and Caribbean region, MMR also declined from 135 MM x 100,000 live births in 1990 to 67 x 100,000 live births in 201522.
According to the National Demographic and Health Survey-NDHS, PMR has been decreasing in Colombia over the years; in 2000, it amounted to 24 x 1,000 live births; in 2005 it went to 17 x 1,000 live births; in 2010 it dropped to 14 x 1,000 live births, and in 2015 to 13.9 x 1,0004,19. Latin America and the Latin Caribbean have the highest perinatal mortality ratios, with figures of 52.8 per 1,000 live births. For the case of South America and some Central American countries, PMRs ranged around 21.4 per 1,000 live births4.
The decrease in maternal and perinatal deaths in Colombia should give rise to specific studies that go beyond the objectives of this research. It could be associated with the implementation of the Millennium Development Goals (MDGs) and later with the Sustainable Development Goals (SDGs) applied in the country since 200023. However, it could also be due to underreporting and even to the attention given to cases on the other side of the borders.
Most maternal and perinatal deaths occurred in the county seats, despite the fact that most of the women resided in scattered rural areas and population centers. Others died in rural areas without medical attention. This could be related to the low supply of maternal services in remote and dispersed areas.
The study established that maternal and perinatal mortality affects the most vulnerable populations. More than 50% of the women with maternal or perinatal deaths were women in the subsidized regime. These results reflect the economic disadvantage of women in the border population who do not have adequate insurance coverage. Similar to this finding, two studies that sought to reflect the situation of maternal and perinatal mortality in Colombia identified that most of the affected women belonged to the subsidized regime24,25. However, the risk of MM and PM is lower among women who have some type of insurance when compared to women in other regimens.
It has been described those women living in rural areas are not able to attend medical care in time when the complication occurs, due to several conditions: the costs involved, the mistreatment many receive from health personnel, the waiting times and the distance between the nearest health care center and the place of residence26. A maternal mortality study conducted in the department of Sucre revealed similar findings, where the majority of the population dies in the county seats, taking into account that many of these women reside in populated centers and dispersed rural areas27.
With regard to the ethnicity of the women who presented any of the events, it is noteworthy that, although most of the events occurred in women registered as mestizo and white, a high percentage occurred in indigenous women, an important fact considering that in the border areas there is a high number of indigenous population. It should be clarified here that the obligation to include this information in the death certificate came into force in Colombia in 2008, which is why many of these data are unknown. Despite this limitation, the findings suggest that indigenous peoples in border areas are more exposed to factors that lead to an increase in cases of MM. Indigenous peoples are exposed to inequalities, given the cultural and ethnic diversity in which they live28.
Another aspect assessed by this study was the marital status of the women. More than half of the women who suffered maternal or perinatal mortality events cohabited with a common-law partner. A study conducted in Mexico, which sought to analyze some social determinants associated with MM, found something contrary to our findings, because approximately half of the women were married29. Another study that evaluated maternal mortality in the Department of Tolima found results similar to ours, where most of the women who died lived in a common-law marriage, followed by those who were single30.
This study identified that most of the mothers were in the age group with the lowest risk of maternal death between 20-34 years of age; however, there is another high number of deaths that occurred in women older than 35 years of age. The age of risk may vary from one country to another or according to the conditions in which the woman lives. Different studies that sought to evaluate the risk of pregnancy at an advanced age, i.e., older than 35 years, concluded that women who become pregnant at that age or older have a higher risk of maternal death31-33. However, other studies have identified the opposite; a study in Pasto suggests that pregnancy at younger ages is riskier and may lead to maternal death34.
Most of these deaths occurred in a hospital or clinic; however, this study highlighted that many deaths occurred at the pregnant woman's home and did not receive medical attention at the time of the complication. This condition could be associated with the remoteness of the places where they live and where they can receive specialized care (those who died at home). It could also be due to the scarcity of economic resources; because of this, some only consult when serious complications arise. Pregnant women, at the time of complications or at the time of delivery, should be attended appropriately. The fact that maternal and perinatal deaths occur at home is a challenge for health systems35.
The study shows that the majority of events (about 90% of women with perinatal death and more than 80% with maternal death) received medical care during the complication leading to death. This raises a question: why did maternal or perinatal death occur if the women received medical care during their complication? Perinatal mortality is an indicator that provides an insight into the quality of maternal and child care in the first days of life; lack of medical care during the birth period can lead to preventable death with appropriate public policies36.
The study also revealed that the basic causes of maternal death were hypertensive disorders, hemorrhage, problems of the respiratory and circulatory systems. According to WHO data, the main complications that can cause about 75% of maternal deaths are: severe hemorrhage, infections, gestational hypertension (preeclampsia and eclampsia), complications of childbirth and unsafe abortion3.
Association analyses performed by logistic regression show that there is a higher risk of perinatal death when the mother is older than 35 years of age. A study in Colombia suggests the opposite, that there is a higher risk of perinatal mortality when the pregnancy is in an adolescent mother34.
Regarding marital status, the association showed that mothers without a partner have a higher risk of perinatal death compared to those with a partner. However, some studies have determined that the marital status of the mother does not influence this type of death37.
Association analyses showed that mothers with cesarean or instrumental delivery have a lower risk of perinatal death. A study carried out in Venezuela, which evaluated the incidence of cesarean section on perinatal mortality, found that cesarean sections were increasing and that the perinatal mortality rate was also increasing. Therefore, it was concluded that performing a cesarean section on the mother does not influence the decrease in perinatal mortality rates, a result contrary to the findings revealed by this research38. These results should be taken with caution, since other authors have indicated the inconvenience of cesarean section as a widely used procedure. This surgical procedure has initially been identified as a method that seeks to reduce both maternal and perinatal morbidity and mortality. Although cesarean section has been defined as a way to reduce deaths, there is a counterpart, which reveals that this surgical procedure can put the life of newborns at risk38.
Mothers who have multiple pregnancies, i.e., twins, triplets, quadruplets, among others, are at higher risk of perinatal death. A study conducted in Mexico found that mothers who had twin pregnancies were at higher risk of perinatal death39.
Geographic barriers represent a problem that the border population has to face in order to access prenatal care services; peripheral health centers have a low capacity to attend high-risk pregnant women. Border municipalities have a high incidence of MM and PM in their departments, with the exception of Boyacá, where these events were generally rarer. In the period studied, maternal and perinatal mortality have decreased; however, the figures continue to be higher than the national average and may even be underestimated due to high underreporting.
As limitations of the study, we must consider that this study considers secondary information from vital statistics. The quality of these records may cause bias in the information provided. On the other hand, there was a high underreporting, as evidenced in the results; several municipalities and townships did not report maternal and perinatal deaths for the time series evaluated.
For the analysis of PM, the records of deaths up to the seventh day of life should be taken into account. However, the official coding of the NADS variables only considers the first 6 days. It was not possible to perform other analyses of MM due to the lack of reliable data on maternal deaths.
The mother's ethnicity variable was included only from the 2008 death certificates, so records from 1998 to 2007 had to be discarded. Likewise, the educational level variable presented a high percentage of data loss; i.e., records with 'no information', and therefore had to be discarded for the analyses, because there was a loss of more than 20% of the records.
REFERENCES
1. UNICEF. La Morbilidad Materna Extremadamente Grave. Cuba: Molinos Trade S.A.; 2013: 209 pag. [ Links ]
2. Instituto Nacional de Salud. Protocolo de Vigilancia en Salud Pública - Mortalidad Materna. Ministerio de Salud y Protección Social 2016: 93 pag. [ Links ]
3. Organización Mundial de la Salud. Mortalidad materna 2018 [cited 2018 Febrero 15]. http://www.who.int/mediacentre/factsheets/fs348/es/. [ Links ]
4. Instituto Nacional de Salud. Protocolo de Vigilancia en Salud Pública Mortalidad Perinatal y Neonatal Tardía. In: Equipo de Maternidad Segura, editor. Bogotá D.C.: Ministerio de Salud y Protección Social; 2016. [ Links ]
5. Lozano-Avendaño L, Bohórquez-Ortiz AZ, Zambrano-Plata GE. Implicaciones familiares y sociales de la muerte materna. Universidad y Salud. 2016;18(2):364-72. [ Links ]
6. Ministerio de Salud y Protección Social. Análisis de situación de Salud. Colombia, 2015. Bogotá, D. C: Ministerio de Salud y Protección Social; 2015: 242 pag. [ Links ]
7. Unigarro DE. "Alegria sin fronteras" entre Brasil, Colombia y Perú: de cómo "tres países hermanos" celebran el nacionalismo. Universidad Nacional de Colombia · Bogotá. 2012;26(1):263-97. [ Links ]
8. Silva NA. Caracterização geográfica, epidemiológica e da organização dos serviços de saúde na tríplice fronteira Brasil/Colômbia/Peru [Tese de Doutorado]. Recife: Centro de Pesquisas Aggeu Magalhães, Fundação Oswaldo Cruz; 2010. Recife Fundação Oswaldo Cruz; 2010. [ Links ]
9. Departamento Administrativo Nacional de Estadística. Estadísticas vitales nacimientos y defunciones DANE2018 [cited 2018 marzo 1]. https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/nacimientos-y-defunciones/estadisticas-vitales-nacimientos-y-defunciones-historicos [ Links ]
10. Departamento Administrativo Nacional de Estadística. Necesidades básicas insatisfechas (NBI) 2006 [cited 2018 Mayo 17]. https://www.dane.gov.co/index.php/estadisticas-por-tema/pobreza-y-condiciones-de-vida/necesidades-basicas-insatisfechas-nbi [ Links ]
11. Departamento Administrativo Nacional de Estadística. Pobreza Monetaria y Multidimensional en Colombia 2017 [cited 2018 Mayo 17]. https://www.dane.gov.co/index.php/estadisticas-por-tema/pobreza-y-condiciones-de-vida/pobreza-y-desigualdad/pobreza-monetaria-y-multidimensional-en-colombia-2017 [ Links ]
12. Congreso de Colombia. Ley 617. Por la cual se reforma parcialmente la Ley 136 de 1994, el Decreto Extraordinario 1222 de 1986, se adiciona la Ley Orgánica de Presupuesto, el Decreto 1421 de 1993, se dictan otras normas tendientes a fortalecer la descentralización, y se dictan normas para la racionalización del gasto público nacional. Bogotá, D. C: Ministerio del Interior; 2000. [ Links ]
13. Fernández-Niño JA, Hernández-Montes RI, Rodríguez-Villamizar LA. Reporte estadístico en los análisis de regresión en Biomédica: una revisión y evaluación crítica. 2018. 2018;38(2):7. [ Links ]
14. Pértegas Díaz S, Pita Fernández S. Cálculo del poder estadístico de un estudio. Investigación: Cálculo del poder estadístico de un estudio. España: Unidad de Epidemiología Clínica y Bioestadística; 2003. [ Links ]
15. Frías MD. Potencia estadística Valencia, España: Universidad de Valencia; 2011 [cited 2020 Mayo 14]. http://www.uv.es/~-friasnav [ Links ]
16. National Cancer Institute. Joinpoint Trend Analysis Software: NIH; [cited 2018 Junio 27]. https://surveillance.cancer.gov/joinpoint/ [ Links ]
17. Organización Panamericana de la Salud, Organización Mundial de la Salud. Lineamientos básicos para el análisis de la mortalidad. Washington, D.C: OPS; 2017. [ Links ]
18. Dirección de Epidemiología y Demografía. Análisis de Situación se Salud (ASIS) Colombia, 2016. Bogotá: Ministerio de Salud y Protección Social; 2016. [ Links ]
19. Sistema Integral de Información de la Protección Social. Sistema de seguimiento de los indicadores básicos de salud: Ministerio de Salud; 2015 [cited 2018 Abril 3]. http://www.sispro.gov.co/Pages/Observatorios/segbasicos.aspx [ Links ]
20. Organización Panamericana de la Salud, Instituto Nacional de Salud. Protocolo de vigilancia epidemiológica de la mortalidad materna. Bogotá: OPS; 2016. [ Links ]
21. Organización Mundial de la Salud, Organización Panamericana de la Salud. Reducción mortalidad materna en 11 países de la Región: Paho; 2014 [cited 2018 Septiembre 28]. https://www.paho.org/clap/index.php?option=com_content&view=article&id=220:reduccion-mortalidad-materna-en-11-paises-de-la-region&Itemid=354&lang=es [ Links ]
22. World Health Organization, Unicef, World Bank Group, United Nations, Unfpa. Trends in Maternal Mortality: 1990 to 2015. Geneva WHO; 2015. [ Links ]
23. Naciones Unidas. Objetivos de Desarrollo del Milenio Informe de 2015. Nueva York UN. 2015. [ Links ]
24. Carrillo U A. Mortalidad materna en Colombia: reflexiones en torno a la situación y la política pública durante la última década. Revista Ciencias de la Salud. 2007;5(2):72-85. [ Links ]
25. Rozo Gutiérrez N. Informe del Evento Mortalidad Perinatal y Neonatal Tardía Periodo Epidemiológico 01-09, Colombia. Mortalidad Perinatal y Neonatal Tardía. Bogotá D.C: Instituto Nacional de Salud; 2017. [ Links ]
26. Campos Castillo C, Hurtado López M, Pulido Reynosa A, Guerrero Hernández A, Briones Garduño JC. Muerte materna en México. Mortalidad Materna. México, D. F: Editorial Alfi; 2013. [ Links ]
27. Buelvas Meza DJ, Sección Análisis de Salud Pública, Dasssalud. Mortalidad materna en Sucre, un problema de salud pública. Inf Quinc Epidemiol Nac. 2008;13(21):319-34. [ Links ]
28. Asociación Probienestar de la Familia Colombiana. Encuesta Nacional de Demografía y Salud 2015. In: Ministerio de Salud y Protección Social, editor. Bogotá: Profamilia; 2016. [ Links ]
29. Karam Calderón MA, Bustamante Montes P, Campuzano González M, Camarena Pliego Á. Aspectos sociales de la mortalidad materna. Estudio de caso en el Estado de México. Medicina Social. 2007;2(4):205-11. [ Links ]
30. Rodríguez Leal D. Muertes maternas: crisis familiares y fallos institucionales. Alicante: Universidad de Alicante 2013. [ Links ]
31. Pons A, Sepúlveda E, Leiva JL, Rencoret G, Germain A. Muerte fetal. Rev Med Clin Las Condes. 2014;25(6):908-16. [ Links ]
32. Yogev Y, Melamed N, Bardin R, Tenenbaum-Gavish K, Ben-Shitrit G, Ben-Haroush A. Pregnancy outcome at extremely advanced maternal age. Am J Obstet Gynecol. 2010;203(6):558.e1-7. [ Links ]
33. Kenny LC, Lavender T, McNamee R, O'Neill SM, Mills T, Khashan AS. Advanced maternal age and adverse pregnancy outcome: evidence from a large contemporary cohort. PloS one. 2013;8(2):e56583. [ Links ]
34. Jurado-Fajardo D, Chaves-Marcillo MC, Belalcázar-Fajardo AT, Achicanoy-Puchana DM, Guerrero CA, Quiñonez-Arteaga CE, et al. Determinantes sociodemográficos y clínicos asociados a mortalidad fetal intrauterina en el municipio de Pasto, 2010-2012. Universidad y Salud. 2017;19(2):207-14. [ Links ]
35. Wong L, Wong E, Husares Y. Mortalidad materna en la Dirección Regional de Salud Ancash. Rev Peru Ginecol Obstet. 2011;57(4):237-41. [ Links ]
36. Departamento Administrativo Nacional de Estadística. Estadísticas Vitales. Cifras preliminars 2014p-2015p. Boletín Técnico. DANE: Bogotá D.C.; 2016. [ Links ]
37. Dámaso-Mata BC, Carbajal-Álvarez C, Loza-Munarriz C, Raraz-Vidal O, Raraz-Vidal J. Factores relacionados a la mortalidad perinatal en un hospital público de Huánuco. Acta Med Peru. 2014;31(1):15-22. [ Links ]
38. Faneite P, Rivera C, Faneite J, Amato R. Cesárea y mortalidad perinatal: Incidencia y tendencia 42 años (1969-2010). Rev Obst Ginecol Venezuela. 2012;72(3):145-51. [ Links ]
39. Panduro B JG, Pérez M JJ, Panduro M EG, Castro H JF, Vázquez G MD. Factores de riesgo prenatales en la muerte fetal tardía, Hospital Civil de Guadalajara, México. Rev Chilena Obstet Ginecol. 2011;76(3):169-74. [ Links ]
Received: April 28, 2020; Accepted: September 21, 2021; pub: April 22, 2022











 texto en
texto en