Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.1 Lima ene./mar. 2022 Epub 24-Feb-2022
http://dx.doi.org/10.31403/rpgo.v68i2397
Original Articles
Characterization and management of subcapsular hepatic hematoma in women with preeclampsia and HELLP syndrome
1. Instituto Nacional Materno Perinatal, Lima, Peru
2. Universidad Nacional Mayor de San Marcos, Faculty of Human Medicine. Lima, Peru
Introduction:
Maternal mortality is higher in developing countries, due to pregnancy and/or puerperium complications, with hepatic rupture being the most catastrophic complication.
Objective:
To describe the characterization and management of subcapsular hepatic hematoma in patients with preeclampsia with severity criteria and HELLP syndrome.
Methods:
Observational, retrospective and descriptive study performed at the Instituto Nacional Materno Perinatal of Peru between 2003 and 2020. Patients with preeclampsia with severity criteria and HELLP syndrome who presented subcapsular hepatic hematoma participated. Information was collected from the clinical history and the surgical technique was documented. Descriptive statistics were used in the data analysis.
Results:
During the study period, 53 patients with subcapsular liver hematoma were identified out of 342.000 deliveries attended. The most frequent symptoms were upper abdominal pain and headache; 37.7% were pregnant women and 62.3% were postpartum women. Surgical treatment by laparotomy and liver packing was performed in 94.3% of the cases. The most frequent complications were multiple organ failure, hypovolemic shock and acute renal failure. Survival rate was 81%.
Conclusions:
An incidence of 1.65 cases of subcapsular hepatic hematoma x 10.000 deliveries was found, with a mortality of ten cases (19%). Subcapsular liver hematoma should be suspected in pregnant women with preeclampsia with severity criteria who present symptoms of epigastric pain and headache, being more frequent in the postpartum period. Laparotomy and liver packing together with volume replacement contribute to the management of these patients, which should be performed promptly in unstable patients.
Key words: Liver; Rupture; Preeclampsia; HELLP syndrome
Introduction
Maternal mortality is higher in developing countries, due to pregnancy and/or puerperium complications1. Hepatic rupture is described as the most catastrophic complication in pregnancy2. Its incidence increases to 0.05% in cases of preeclampsia, eclampsia and HELLP syndrome3,4. Likewise, hepatic rupture is associated with maternal and fetal mortality in 50% and 80% of cases, respectively5.
The pathophysiology has been attributed to vascular endothelial dysfunction in the liver leading to thrombin and fibrin deposits in hepatic arterioles and sinusoids. These deposits cause sinusoidal obstruction and intrahepatic vascular congestion, increased intrahepatic pressure, ischemia and periportal hemorrhagic necrosis, which finally lead to hepatic subcapsular hematoma3,6,7. Rupture is caused by increased intra-abdominal pressure due to abdominal palpation, uterine contractions during labor and even during transport of the pregnant woman. The most common symptom of hematoma or hepatic rupture is pain in the epigastrium or right upper quadrant of the abdomen, a common presenting feature of severe preeclampsia; other clinical manifestations include shoulder pain, vomiting and even sudden and massive circulatory collapse8,9.
The objective of this study is to describe the clinical characterization, medical and surgical management of cases of hepatic rupture in women with preeclampsia with severity criteria and HELLP syndrome attended at the Instituto Nacional Materno Perinatal, Lima, Peru, between 2003 and 2020.
Methods
This is an observational, retrospective and descriptive study conducted at the Instituto Nacional Materno Perinatal (National Maternal-Perinatal Institute (NMPI) of the Peruvian Ministry of Health), which is a third-level care facility, category III-2, and a national reference center.
The study included pregnant women with a diagnosis of preeclampsia with severity criteria and/or HELLP syndrome attended between 2003 and 2020. All cases of pregnant women who presented with ruptured and non-ruptured subcapsular hepatic hematoma and who had a record of their findings and description of the procedures in the clinical history were included. Those pregnant women without confirmed findings in the clinical record were excluded.
Subcapsular hepatic hematoma was defined as direct visualization of the hematoma through laparotomy and/or by means of diagnostic imaging examination recorded in the clinical history. The steps recorded for the surgical management of the hepatic hematoma were collected, as well as the documented images of the same.
To collect the information, the medical records of pregnant women with a diagnosis of preeclampsia were identified in the institution's Statistics and Informatics Office, reviewing and verifying the diagnoses recorded by the attending physician and applying the inclusion and exclusion criteria. Information was collected on maternal age measured in years and classified as under 19, 19 to 35 years and over 35 years of age; parity; obstetric morbidity such as severe preeclampsia, HELLP syndrome, eclampsia, placental abruption, placenta previa, intrauterine growth restriction or any other morbidity specified in the maternal history; route of pregnancy term (vaginal, cesarean section or cesarean section with hysterectomy); clinical symptoms and signs; diagnostic means to identify hepatic subcapsular hematoma (ultrasound, clinical, at cesarean section); laboratory tests; medical treatment received, surgical treatment performed; postsurgical complications; reinterventions; days of hospitalization and occurrence of maternal death.
The information was collected on an ad hoc form, taking the necessary precautions to guarantee the anonymity of the participants, by means of alphanumeric coding of their identity.
In the statistical analysis, for the categorical variables, contingency tables were made with representations of absolute frequencies and proportional frequencies by column. For the numerical variables, measures of central tendency such as mean and median were used and, as measures of dispersion, standard deviation and ranges. The data were processed in R statistical software version 4.0 and its R studio platform.
The research had the approval of the NMPI Institutional Research Ethics Committee and the corresponding institutional permission. The identity of the participants was protected by alphanumeric coding.
Results
In the period from 2003 to 2020, 53 cases of ruptured and non-ruptured subcapsular hepatic hematoma in patients with preeclampsia with severity criteria and/or HELLP syndrome were managed at the NMPI. There were between 0 and 7 cases per year, with an average of 2.9 cases per year. The years 2014, 2015 and 2017 handled the highest number of cases, 7 per year. No cases occurred in 2004 and 2007 (Figure 1).
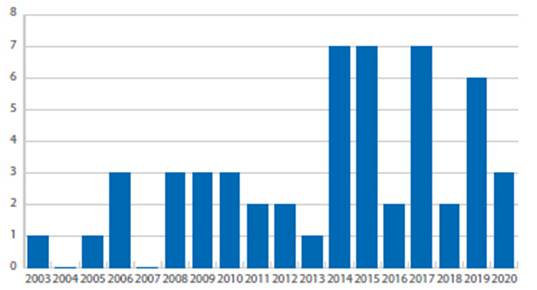
Source: Own elaboration
Figure 1 Annual number of cases of pregnant women with hepatic subcapsular hematoma. National Maternal-Perinatal Institute, Lima, Peru, 2003-2020.
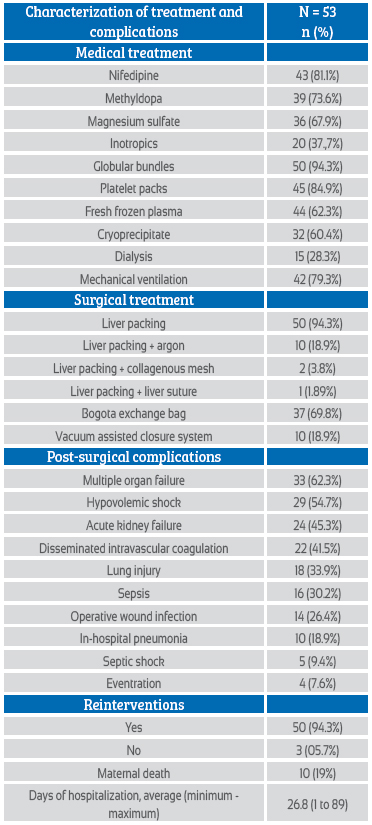
The majority of pregnant women, 29 cases (54.7%) were between 19 and 35 years of age, followed by 21 cases (39.6%) over 35 years of age and 3 cases (5.7%) under 19 years of age. The mean age was 32.3 years, with minimum and maximum values of 19 and 48 years. Of the pregnant women, 69.8% were multiparous and 30.2% were nulliparous. The main obstetric conditions presented by the pregnant women with subcapsular hepatic hematoma were severe preeclampsia (97.2%), HELLP syndrome (67.9%), eclampsia (11.3%) and placental abruption (11.3%). In 69.9% of the pregnant women, gestation was terminated by cesarean section and 13.2% vaginally; in nine pregnant women, the termination was by cesarean section with hysterectomy (Table 1).
Table 1 Maternal characteristics of pregnant women with subcapsular hepatic hematoma.
Source: Own elaboration
* The obstetric morbidity condition does not add up to 53 cases, since the same patient may have developed more than one obstetric morbidity.
Most cases of subcapsular hepatic hematoma occurred during the puerperium, with 33 cases (62.3%); the other 20 cases occurred during pregnancy (37.7%). Diagnosis was by ultrasound (39.6%), during cesarean section (33.9%) or clinically (26.5%). The most frequent symptoms in pregnant women with subcapsular hematoma were upper abdominal pain (41.5%), headache (26.4%), scotomas (7.5%); 23 cases had no symptoms (43.4%). On admission, laboratory tests of liver function (prothrombin time, partial thromboplastin time, glutamic oxaloacetic transaminases, glutamic pyruvic transaminases, total bilirubins, direct and indirect bilirubins) and creatinine were increased, while hemoglobin and platelet count were below normal values (Table 2).
Table 2 Clinical and laboratory characterization of pregnant women with hepatic subcapsular hematoma.
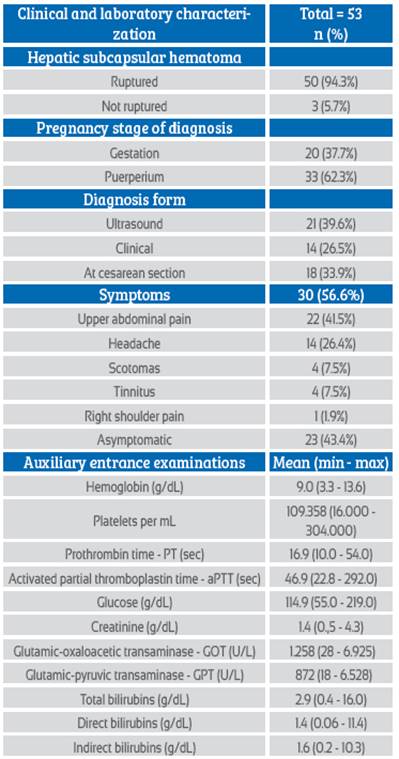
Source: Own elaboration
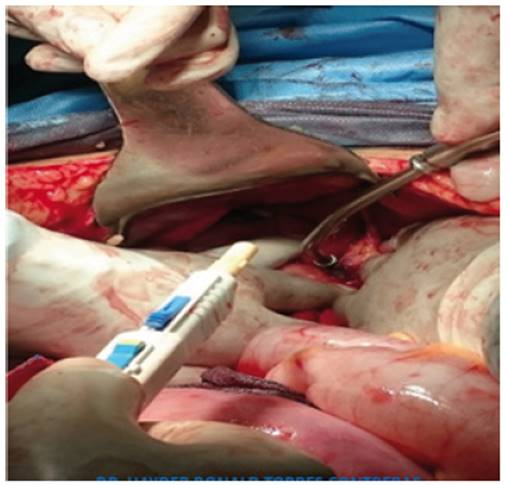
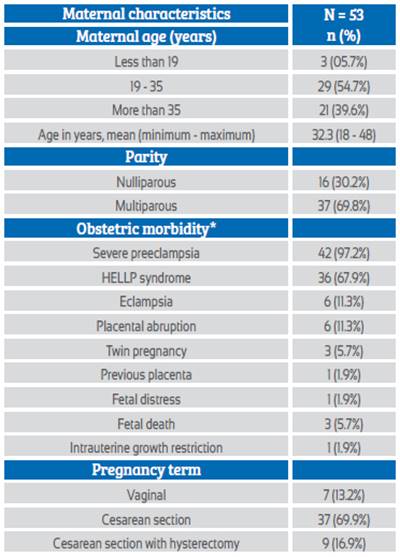
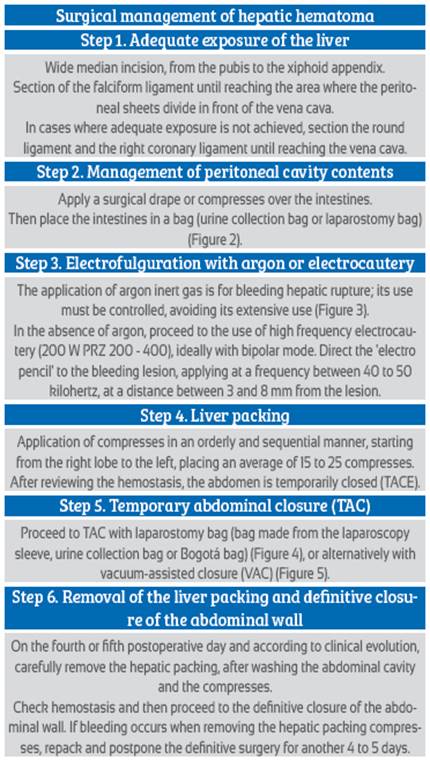
Of the 53 pregnant women, conservative management was performed in three cases (5.7%) and in 50 patients (94.3%) it was necessary to perform some surgical intervention. The surgical intervention consisted of salvage laparotomy or damage control surgery, the basic surgery being hepatic packing (50 cases; 94.3%), followed by temporary abdominal closure (TAC) (Tables 3 and 4) (Figure 2).
Table 3 Procedures in the surgical management of hepatic hematoma in pregnant women with preeclampsia with severity criteria and HELLP syndrome.
Source: Own elaboration
Of the 53 pregnant women, conservative management was performed in three cases (5.7%) and in 50 patients (94.3%) it was necessary to perform some surgical intervention. The surgical intervention consisted of salvage laparotomy or damage control surgery, the basic surgery being hepatic packing (50 cases; 94.3%), followed by temporary abdominal closure (TAC) (Tables 3 and 4) (Figure 2).
Prior to liver packing, 10 patients (18.9%) received argon electrofulguration (Figure 3), to control a bleeding liver lesion. In two patients (3.8%) with persistent hepatic bleeding in napa, the first management consisted in the placement of collagen mesh and/or absorbent collagen sponge, basically used for small lesions, and then continued with hepatic packing. In one patient (1.9%) with a persistent bleeding lesion and poor response to electrocautery fulguration, hepatic suture was performed in a ruptured hepatic segment, and then continued with hepatic packing. In 37 cases (69.8%), after liver packing, temporary closure of the abdomen was performed with a laparostomy bag (Bogota bag) (Figure 4), which was fixed to the aponeurotic tissue or to the skin. In ten patients (18.9%), after initial surgical management and hepatic packing, the TAC was performed with vacuum-assisted closure (VAC), which was replaced on some occasions between 48 and 72 hours after hepatic packing (Table 4) (Figure 5).
Of the 47 patients (94.3%) who underwent TAC, a laparostomy bag was used in 37 patients and a CAV system in 10 patients. These patients were reoperated in most cases between the 4th and 5th day after liver packing. In the first three years of management of this type of patients, three of them underwent abdominal wall closure after liver packing; these women had a torpid evolution, as they developed compartment syndrome and multiorgan failure as a complication, ending days later with the death of two of them.
In the 17 years reported in the present study, survival was achieved in 81% of the cases.
Discussion
In the period studied, there have been 53 cases of ruptured and unruptured hepatic subcapsular hematoma, a rare entity whose pathophysiology has not been elucidated. There were 342,000 deliveries in that period, giving an incidence of subcapsular hematoma of 1 in 6,450 deliveries. This was higher than that published by Karateke, of 1 in 40,000 to 250,000 deliveries10, and could be explained by the fact that our study was performed in a national reference facility.
The highest number of cases was in women younger than 35 years, which represented 60% of the total number of cases and whose mean age was 32 years. This was similar to the findings of Grand'Maison11 with a median age of 29 years and Escobar7, who found a median age of 32 years. Regarding parity, multiparous women were more than twice as likely to be multiparous as nulliparous women, 70% versus 30%. This differs from the review by Dubey et al12, in which primiparas were the majority group with 56% of the cases. However, it coincides with the findings of Vigil et al8, where the majority group was multiparous with 57% of the cases.
The obstetric morbidity most associated with cases of subcapsular hepatic hematoma was preeclampsia with signs of severity in 97% of the cases, and HELLP syndrome in 68%. Dubey et al12 found that the main associated cause was HELLP syndrome in 75%, and severe preeclampsia in only 20%. This difference may be due to differences in population characteristics and care times, since most of the data come from studies carried out in developed countries.
The majority of gestations were terminated by cesarean section (87%), a figure higher than that reported by Araujo et al13, with a rate of 60%, but close to that found in the review by Dubey et al12 of 82%. These differences in time could be explained by the greater knowledge we now have about how catastrophic the evolution of HELLP syndrome or preeclampsia with signs of severity can be, and physicians no longer decide to wait longer for the occurrence of a vaginal delivery.
Hepatic rupture occurred more frequently in the postpartum period, with 62%. However, in the series of Araujo et al13 they found only 10%; a slightly higher figure was reported by Henríquez et al14, with 29% of the diagnoses in the puerperium.
Recognition of the symptoms may raise suspicion of this condition. However, these are nonspecific and, in some cases, overlapping. Upper abdominal pain was present in 42%, being the most frequent; this was related to hepatic ischemia. Headache was present in 26% of cases, which could be due to hypertension and hypovolemia. Upper abdominal pain and headache were frequent symptoms reported in other studies15,16. On the other hand, this study found that 43% of cases had no symptoms, higher than the 27% found by Gonzales et al17.
The alteration of the ancillary tests was mainly manifested in hemoglobin, with a median value of 9 g/dL; the median platelet count was 109,358/mL. Araujo et al13 found lower figures, with median hemoglobin of 7.8 g/dL and platelets 91,300/mL. Glutamic oxaloacetic transaminase (GOT) and glutamic-pyruvic transaminase (GPT) were found to be elevated, with medians of 1,258 U/L and 872 U/L, respectively; this is in agreement with most published series8,12. Indirect bilirubin is an approximate marker of hemolysis; the mean in our study was 1.6 g/dL, similar to that found by Gonzales et al17.
Due to the low incidence of the pathology, management is not standardized; however, it has been found that surgery significantly reduces mortality8. This includes embolization of the hepatic artery, ligation of the hepatic artery and tamponade and drainage of the hepatic lesion, which will allow control of bleeding9,18. In the present study, the main treatment was hepatic packing in 94% of the cases, which was accompanied by the use of direct argon fulguration in 19%, collagen mesh and suture, both in 3.8%. In the review by Dubey et al12, this technique was used in 52% of patients. In other studies, occlusion of the hepatic artery, either by surgical ligation or by embolization through interventional radiology, was the main way of resolving the condition11. However, the results were hit and miss during pregnancy, with complications such as elevated liver enzymes and acute gangrenous cholecystitis. Hepatic packing has been associated with 82% survival10.
In the world literature, there are several surgical approaches in cases of ruptured and non-ruptured hepatic subcapsular hematoma. However, the published series include very few patients, which makes it difficult to determine which surgical techniques are most commonly used. The five series reviewed in the world literature with the largest number of cases include only three to eight18-22.
The characteristics of the liver of a pregnant and/or postpartum woman with severe preeclampsia and HELLP syndrome are different from those of a non-pregnant woman. These characteristics are the presence of physiological hepatomegaly, greater venous and arterial congestion and greater circulatory flow3,6,7. For these reasons, the patients attended in the present study underwent hepatic packing, with temporary closure of the abdomen, either with a laparostomy bag or with a vacuum-assisted closure system.
The review by Dubey et al13 reports that the main complications were acute respiratory distress syndrome (29%), renal failure (10%) and abscess (14%). Whereas, the main complications observed in our study were multiple organ failure, hypovolemic shock, acute renal failure and disseminated intravascular coagulation and sepsis, many of them overlapping. On the other hand, mortality in our patients was 19%, very similar to the world literature (17%), despite the limited resources and tools for the management of this pathology9,23. The present study presents the largest case report on the management of ruptured and unruptured subcapsular hematoma found in the world literature.
With respect to the limitations of this communication, they correspond to those of a retrospective study in the collection of information. However, these data pertain to patients with a complete medical history, with supervision of data collection.
Conclusions
In the study population there were 53 cases of hepatic subcapsular hematoma in patients with preeclampsia with severity criteria and HELLP syndrome, with an incidence of 1.65 cases x 10,000 deliveries and a mortality of ten cases (19%). The identification of hepatic rupture/hematoma should be suspected in those pregnant women with preeclampsia with severity criteria who present symptoms of epigastric pain, headache, sudden pallor and hypotension, either in the prepartum period, but more frequently in the postpartum period. Laparotomy and liver packing along with volume replacement contribute to the management of patients with hepatic subcapsular hematoma, which should be performed promptly in unstable patients.
It is recommended that pregnant women receive adequate prenatal care from the first trimester of gestation, in order to identify pregnant women at higher risk of preeclampsia, who should be referred to a health facility with a higher level of maternal and neonatal resolution capacity, in order to prevent severe maternal morbidity and maternal and perinatal mortality.
REFERENCES
1. Alkema L, Chou D, Hogan D, Zhang S, Moller A, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario- based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet Lond Engl. 2016;387(10017):462-74. Doi: 10.1016/S0140-6736(15)00838-7 [ Links ]
2. Ditisheim A, Sibai BM. Diagnosis and management of HELLP syndrome complicated by liver hematoma. Clin Obstet Gynecol. 2017;60(1):190-7. doi: 10.1097/GRF.0000000000000253 [ Links ]
3. Pavlis T, Aloizos S, Aravosita P, Mystakelli C, Petrochilou D, Dimopoulos N, et al. Diagnosis and surgical management of spontaneous hepatic rupture associated with HELLP syndrome. J Surg Educ. 2009;66(3):163-7. Doi: 10.1016/j.jsurg.2009.04.001 [ Links ]
4. Agarwal A, Joy D, Das P, Dash NR, Srivastava DN, Madhusudhan KS. Hemorrhage and rupture of an unusual benign liver lesion in pregnancy: A case report. J Clin Exp Hepatol. 2021;11(2):260-3. Doi: 10.1016/j.jceh.2020.07.004 [ Links ]
5. Marsh FA, Kaufmann SJ, Bhabra K. Surviving hepatic rupture in pregnancy-a literature review with an illustrative case report. J Obstet Gynaecol. 2003;23(2):109-13. Doi: 10.1080/0144361031000074583 [ Links ]
6. Pérez M, Sáez V. Hematoma subcapsular hepático. Grave complicación del embarazo. Medisur [Internet]. 2010 [citado 2021 Oct 12];8(6):445-51. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1727-897X2010000600008&lng= es [ Links ]
7. Sibai BM, Ramadan MK, Usta I, Salama M, Mercer BM, Friedman SA. Maternal morbidity and mortality in 442 pregnancies with hemolysis, elevated liver enzymes, and low platelets (HELLP syndrome). Am J Obstet Gynecol. 1993;169(4):1000-6. Doi: 10.1016/0002-9378(93)90043-I [ Links ]
8. Vigil-De Gracia P, Ortega-Paz L. Pre-eclampsia/eclampsia and hepatic rupture. Int J Gynecol Obstet. 2012;118(3):186-9. Doi: 10.1016/j.ijgo.2012.03.042 [ Links ]
9. Escobar Vidarte MF, Montes D, Pérez A, Loaiza-Osorio S, Nieto J. Hepatic rupture associated with preeclampsia, report of three cases and literature review. J Matern Fetal Neonatal Med. 2019;32(16):2767-73. Doi: 10.1080/14767058.2018.1446209 [ Links ]
10. Karateke A, Silfeler D, Karateke F, Kurt R, Guler A, Kartal I. HELLP Syndrome complicated by subcapsular hematoma of liver: A case report and review of the literature. Case Rep Obstet Gynecol. 2014;2014:e585672. Doi: 10.1155/2014/585672 [ Links ]
11. Grand'Maison S, Sauvé N, Weber F, Dagenais M, Durand M, Mahone M. Hepatic rupture in hemolysis, elevated liver enzymes, low platelets syndrome. Obstet Gynecol. 2012;119(3):617-25. Doi: 10.1097/AOG.0b013e318245c283 [ Links ]
12. Dubey S, Rani J. Hepatic rupture in preeclampsia and HELLP syndrome: A catastrophic presentation. Taiwan J Obstet Gynecol. 2020;59(5):643-51. Doi: 10.1016/j.tjog.2020.07.003 [ Links ]
13. Araujo ACPF, Leao MD, Nobrega MH, Bezerra PFM, Pereira FVM, Dantas EMM, et al. Characteristics and treatment of hepatic rupture caused by HELLP syndrome. Am J Obstet Gynecol. 2006;195(1):129-33. Doi: 10.1016/j.ajog.2006.01.016 [ Links ]
14. Henríquez-Villaseca MP, Catalán-Barahona A, Lattus-Olmos J, Vargas-Valdebenito K, Silva-Ruz S. Ruptured subscapular liver hematoma in context of HELLP syndrome. Rev Med Chil. 2018;146(6):753-61. Doi: 10.4067/s0034-98872018000600753 [ Links ]
15. Colín-Cortes HM, Ruvalcaba-Carrillo R, Olivares-Revilla DM, Yáñez-Torres J de JO, Flores-Rodríguez JL, Rodríguez-Figueroa N, et al. Hematoma subcapsular hepático en síndrome de HELLP: reporte de dos casos. Ginecol Obstet México. 2018;86(06):412-9. Doi: https://doi.org/10.24245/gom.v86i6.2048 [ Links ]
16. Cruz-Santiago J, Meza-Jiménez G, Ayala-López EA, Velázquez- García JA, Moreno-Ley PI, Robledo-Meléndez A, et al. Ruptura hepática en el síndrome de HELLP. Revisión del tratamiento quirúrgico. Cir Gen. 2020;42(1):31-7. doi: 10.35366/92709 [ Links ]
17. Gonzales Carrillo OM, Llanos Torres CD, De la Peña Meniz W. Hematoma hepático subcapsular en síndrome HELLP en un hospital de referencia de Lima. Rev Peru Ginecol Obstet. 2017;63(2):171-81. http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S2304-51322017000200004&lng= es [ Links ]
18. Corinna W, Pereira P, Neeser E, Flesch I, Rodegerdts E, Becker H. Subcapsular liver hematoma in HELLP syndrome: Evaluation of diagnostic and therapeutic options - A unicenter study. Am J Obstet Gynecol. 2004;9(1):106-12. Doi: https://doi.org/10.1016/j.ajog.2003.08.029 [ Links ]
19. Merchant SH, Mathew P, Vanderjagt TJ, Howdieshell TR, Crookston KP. Recombinant factor VIIa in management of spontaneous subcapsular liver hematoma associated with pregnancy. Obstet Gynecol. 2004;103(2):1055-8. doi: 10.1097/01.AOG.0000127943.68645.96 [ Links ]
20. Nunes J, Turner M, Fulcher A. Abdominal imaging features of HELLP syndrome: A 10-year retrospective review. Am J Roentgenol. 2005;185:1205-10. Doi: https://www.ajronline.org/doi/10.2214/AJR.04.0817 [ Links ]
21. El Youssoufi S, Nsiri A, Salmi S, Miguil M. Liver rupture in peripartum: about 8 cases. J Gynecol Obstet Biol Reprod. 2007;36(1):57-61. doi: 10.1016/j.jgyn.2006.09.003 [ Links ]
22. Pavlis T, Aloizos S, Aravosita P, Mystakelli C, Petrochilou D, Dimopoulos N, Gourgiotis S. Diagnosis and surgical management of spontaneous hepatic rupture associated with HELLP syndrome. J Surg Educ. 2009;66(3):163-7. doi: 10.1016/j.jsurg.2009.04.001 [ Links ]
23. Gupta A, Joseph SR, Jeffries B. Managing a rare complication of HELLP syndrome in Australia: Spontaneous liver haematoma in pregnancy. Aust N Z J Obstet Gynaecol. 2021;61(2):188-94. Doi: 10.1111/ajo.13318 [ Links ]
The present publication is original and has not been previously published in another institution and/or scientific journal. The present study has been approved by the Institutional Ethics Committee and has the permission of the institution
Funding: The authors certify that we have not received specific financial support, equipment or materials from individuals, public and/or private institutions for the conduct of this study
Received: December 30, 2021; Accepted: January 22, 2022; pub: February 22, 2022











 texto en
texto en