Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.1 Lima ene./mar. 2022 Epub 24-Feb-2022
http://dx.doi.org/10.31403/rpgo.v68i2392
Case Report
Cotyledonoid dissecting leiomyoma of the uterus
1. Department of Obstetrics and Gynecology, Hospital Central "Dr. Urquinaona", Maracaibo, Zulia State, Venezuela
Benign smooth muscle tumors are the most common tumors in the female genital tract. Cotyledonoid dissecting leiomyoma of the uterus is a rare variant of benign leiomyoma, which presents unusual growth patterns and shares some features with other variants of dissecting leiomyoma. It has an unusual growth pattern characterized by intramural dissection within the myometrium and with similar appearance of its extrauterine components to placental cotyledons. Its sarcomatoid appearance and unusual character give the impression of malignancy. The diagnosis is made by the characteristic histopathologic findings of the lesion. A case of cotyledonoid dissecting leiomyoma of the uterus is presented.
Key words: Cotyledonoid dissecting leiomyoma; Uterine neoplasms; Muscle; smooth
Introduction
Benign smooth muscle tumors are common in the female genital tract. Myoma variants account for approximately 10% of cases1. Leiomyomas with unusual growth pattern include both diffuse, intravenous uterine leiomyomatosis and leiomyoma with vascular invasion, benign metastatic, parasitic, disseminated peritoneal, dissecting, and with perinodular hydropic degeneration2.
Cotyledonoid dissecting leiomyoma (CDL) of the uterus, also known as Sternberg's tumor, is an extremely rare but benign variant of uterine fibroids. It is characterized by the presence of reddish, spongy, bulbous and exophytic extrauterine nodules, similar to the placental maternal face and with a tendency to expand into neighboring structures. Approximately 50 cases have been reported to date2-3. Although it is a benign neoplasm, the macroscopic appearance and unusual growth pattern may be similar to malignant lesions4. A case of cotyledonoid dissecting leiomyoma of the uterus is presented.
Case report
This is a 50-year-old female patient, gestation 2, para 2, who was referred to the gynecology office for presenting menorrhagia and bladder urgency accompanied by paresthesia of both lower limbs, of several months' duration. The patient had been diagnosed with uterine myomatosis for 9 years. She reported that both deliveries were spontaneous and without complications. She denied the use of hormone replacement therapy, alcohol consumption, smoking, illegal drug use and medical or family history of importance.
On physical examination, the abdomen was soft and depressible, with a soft and mobile tumor. On inspection, the cervix and vagina were normal. Vaginal examination showed the presence of a lesion corresponding to the posterior aspect of the uterus.
Ultrasound found an enlarged uterus with several subserosal uterine fibroids and a heterogeneous, exophytic lesion with irregular margins arising from the posterior aspect of the uterus and measuring 8 x 7 x 6 centimeters, extending towards the right adnexa and fundus of the pouch of Douglas (Figure 1). The cervix was short, the vaginal walls were lax and both adnexa were free. Doppler evaluation assessed low intratumoral resistance index. Abdomino-pelvic tomography images showed a lobulated mass arising from the right posterolateral uterine wall, with attenuation values similar to soft tissue and extending to the right fornix and right adnexa. There was no evidence of ascites, peritoneal thickening or abdominopelvic lymphadenopathy. The presumptive preoperative diagnosis was gastrointestinal stromal tumor.
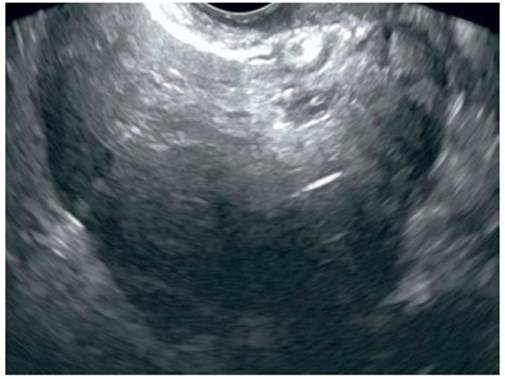
Figure 1 Ultrasound image of a heterogeneous, exophytic lesion with irregular margins arising from the posterior aspect of the uterus, extending towards the right adnexa.
Hematology, renal and liver function, electrolytes, urine test and coagulation profile were within normal limits. CA-125 concentrations were 40 IU/L (normal value less than 35 IU/L). The rest of the tumor markers (chorionic gonadotropin, CA19-9, carcinoembryonic antigen and alpha-fetoprotein) were within normal limits. In view of the findings the case management was discussed with the patient and it was decided to perform surgery.
During the gynecological laparotomy, an enlarged, myomatous uterus was found, together with an extrauterine tumor, soft, mucoid in appearance, with multiple nodules resembling placental cotyledons, originating from the posterior uterine face and extending towards the right broad ligament, pelvic cavity and pouch of Douglas, but without affecting it. The ovaries and bowel loops appeared normal. Frozen section of the lesion suggested smooth muscle neoplasia without cytologic atypia. Total abdominal hysterectomy with bilateral salpingo-oophorectomy, omentectomy and appendectomy were performed.
On anatomopathologic evaluation, the extrauterine tumor measured 8 × 7 x 6 centimeters and protruded from the posterior uterine wall, with multiple deep red nodules that were similar in appearance to the placental maternal face. The nodules were rubbery, reddish, and solid, ranging from 0.5 to 2 centimeters in diameter, and were closely connected by fibrous tissue (Figure 2). Cross sections showed multinodular proliferation of smooth muscle tissue with a cotyledonous architecture.
Histological examination found that the nodules were of variable size, of muscle fascicles with hydropic changes, rich vascularization and marked hyalinized degeneration, separated by abundant intercellular collagen fibers. Smooth muscle cell fascicles showed disorganized and swirling appearance with slightly enlarged nuclei (Figure 3). Intratumoral vessels were congested and dilated. There was no evidence of atypia, mitosis or necrosis suggestive of malignant changes. On immunohistochemical staining, stromal cells were positive for desmin and smooth muscle actin in tumor cells. Vimentin was positive in intermediate fibrous septa, including vessel walls, and was only focally positive in tumor cells. The Ki67 proliferation index was 2%. The myometrium was diffusely thickened without nodular lesions, and no alterations were found in the fallopian tubes. In view of the findings, the definitive diagnosis was CDL of the uterus without evidence of malignancy.
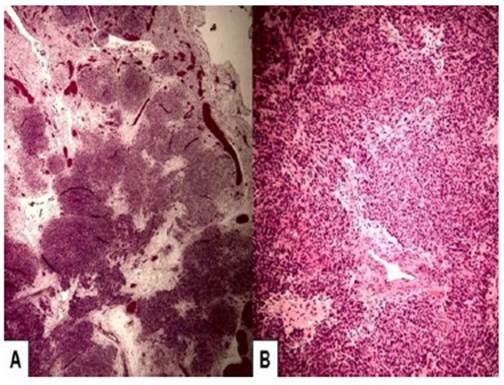
Figure 3 Microscopic image of cotyledonoid dissecting leiomyoma of the uterus. A) Nodules of different sizes separated by lax fibrous tissue with multiple blood vessels. B) Smooth muscle cells arranged in intertwined fascicles with a disorganized and whirling appearance. Hematoxylin - eosin staining.
The patient presented satisfactory recovery during the postoperative period and was discharged three days after surgery. She was monitored with regular postoperative visits at the outpatient clinic, with no evidence of recurrence during the 18 months of postoperative follow-up.
Discussion
Uterine leiomyomas are the most frequent uterine tumors observed between the third and sixth decades of life. Typical uterine fibroids present a typical, well-circumscribed and uniformly expansive growth pattern5. CDL (also known as Sternberg's tumor) is an extremely rare variant of dissecting leiomyoma characterized by unusual, exophytic (placental-like), reddish growth pattern with extension into adjacent tissues. To date, less than 50 cases have been described5,6.
The proposed mechanism of development of CDL is by extension from the uterine wall to the pelvic cavity. Myometrial and stromal glandular cells are trapped in the connective tissue of the intramural component of the tumor, leading to congestion and hydropic changes7. There are three types of uterine CDL. The first appears as an exophytic lesion of multinodular tissue protruding from the uterine surface, similar to the placenta. The second type is an intramural dissecting tumor that is confined to the uterus. These two types share similar histopathologic features. The third type is pure cotyledonal leiomyoma, which is not associated with intramural lesion or dissection8. The case presented corresponded to the first type.
Clinically, the symptomatology of uterine CDL is abnormal uterine bleeding and abdominal or pelvic lump, the latter usually discovered accidentally. The size can range from 10 to 41 centimeters9. Some tumors appear as large fungiform lesions with wide extension into the broad ligaments and pelvic cavity. Due to their low frequency, they can be mistaken for malignant tumors3.
CDL has features similar to typical myoma on imaging studies. On ultrasound, the tumor appears lobulated and more voluminous compared to the typical leiomyoma. However, imaging is not useful for diagnosis10. Three-dimensional ultrasound can be useful in specifically describing the characteristics of the nodules11. On T2-weighted magnetic resonance images, the tumor is less heterogeneous than sarcomatous lesions, with isointense myometrial-like images on T1-weighted images10.
Pathologic evaluation shows that the CDL is composed of smooth muscle with a dissecting growth pattern. The extrauterine cotyledonary extension is characterized by nodules of muscle fascicles of variable size surrounded by collagen fibers, with hydropic changes and high vascularization. The neoplastic smooth muscle cells form disorganized fascicles in contrast to the organized pattern of conventional leiomyomas12. More than 90% of cases have a dissecting component with infiltrating, sinus-like tongues extending at least 5 millimeters into the surrounding tissue1,10.
The vessels are dilated and congested within the extrauterine nodules, while these are round and sometimes hyalinized in the intramural portion. Approximately 20% of cases present vascular invasion; however, it does not change the benign clinical course of the disease4. All reported cases have benign behavior despite pathological prognostic factors, such as lymphovascular invasion10,13. Unlike other malignant lesions, CDL does not show signs of mitotic activity, nuclear atypia, cellular pleomorphism or necrosis13.
Differential diagnoses include hydropic leiomyoma, leiomyoma with perinodular hydropic degeneration, myxoid leiomyoma, intravenous leiomyomatosis, low-grade endometrial stromal sarcoma, perivascular epithelioid cell tumors and leiomyosarcoma10. Although intravenous leiomyomatosis may be multinodular and involve the broad ligament, the exophytic component is not congestive and intravascular growth is common14. Multinodularity of the extrauterine component and hydropic connective tissue changes are common in both CDLs and in some leiomyomas with perinodular hydropic degeneration; but the latter does not have a macroscopic appearance similar to placental cotyledons15.
The standard treatment for CDL of the uterus is hysterectomy, although some cases have been treated conservatively. However, there is one report of tumor recurrence in a single case initially treated conservatively by myomectomy and removal of the extrauterine tumor13. To date, no cases of metastasis have been described, which would support the fact of the benign nature of this variant of leiomyoma.
In conclusion, cotyledonoid dissecting leiomyoma of the uterus is a rare variant of leiomyoma. It is a rare benign tumor with multiple placental maternal face-like nodules, different from the typical leiomyoma. Its sarcomatoid appearance and unusual character give the impression of malignancy. The standard treatment is hysterectomy, as conservative treatment may be associated with tumor recurrence.
REFERENCES
1. Sonmez FC, Tosuner Z, Karasu AFG, Arici DS, Dansuk R. Cotyledonoid dissecting leiomyoma with symplastic features: case report. Rev Bras Ginecol Obstet. 2017;39(8):436-40. doi: 10.1055/s-0037-1604057 [ Links ]
2. Xu T, Wu S, Yang R, Zhao L, Sui M, Cui M, et al. Cotyledonoid dissecting leiomyoma of the uterus: A report of four cases and a review of the literature. Oncol Lett. 2016;11(4):2865-8. doi: 10.3892/ol.2016.4314 [ Links ]
3. Jamal I, Gupta RK, Sinha RK, Bhadani PP. Cotyledonoid dissecting leiomyoma: an uncommon form of a common disease. Obstet Gynecol Sci. 2019;62(5):362-6. doi: 10.5468/ogs.2019.62.5.362 [ Links ]
4. Parker WH, Turner R, Schwimer S, Foshag L. Massive cotyledenoid leiomyoma treated with uterine-conserving surgery. F S Rep. 2020;1(3):314-6. doi: 10.1016/j.xfre.2020.07.007 [ Links ]
5. Smith CC, Gold MA, Wile G, Fadare O. Cotyledonoid dissecting leiomyoma of the uterus: a review of clinical, pathological, and radiological features. Int J Surg Pathol. 2012;20(4):330-41. doi: 10.1177/1066896912450315 [ Links ]
6. Roth LM, Reed RJ, Sternberg WH. Cotyledonoid dissecting leiomyoma of the uterus. The Sternberg tumor. Am J Surg Pathol. 1996;20(12):1455-61. doi: 10.1097/00000478-199612000-00004 [ Links ]
7. Saeed AS, Hanaa B, Faisal AS, Najla AM. Cotyledonoid dissecting leiomyoma of the uterus: a case report of a benign uterine tumor with sarcomalike gross appearance and review of literature. Int J Gynecol Pathol. 2006;25(3):262-7. doi: 10.1097/01.pgp.0000186542.19434.ea [ Links ]
8. Aleksandrovych V, Bereza T, Sajewicz M, Walocha JA, Gil K. Uterine fibroid: common features of widespread tumor (Review article). Folia Med Cracov. 2015;55(1):61-75. [ Links ]
9. Kim NR, Park CY, Cho HY. Cotyledonoid dissecting leiomyoma of the uterus with intravascular luminal growth: a case study. Korean J Pathol. 2013;47(5):477-80. doi: 10.4132/KoreanJPathol.2013.47.5.477 [ Links ]
10. Xu T, Wu S, Yang R, Zhao L, Sui M, Cui M, et al. Cotyledonoid dissecting leiomyoma of the uterus: A report of four cases and a review of the literature. Oncol Lett. 2016;11(4):2865-8. doi: 10.3892/ol.2016.4314 [ Links ]
11. Raga F, Sanz-Cortés M, Casañ EM, Burgues O, Bonilla-Musoles F. Cotyledonoid dissecting leiomyoma of the uterus. Fertil Steril. 2009;91(4):1269-70. doi: 10.1016/j.fertnstert.2008.08.131 [ Links ]
12. Weissferdt A, Maheshwari MB, Downey GP, Rollason TP, Ganesan R. Cotyledonoid dissecting leiomyoma of the uterus: a case report. Diagn Pathol. 2007;2:18. doi: 10.1186/1746-1596-2-18 [ Links ]
13. Roth LM, Kirker JA, Insull M, Whittaker J. Recurrent cotyledonoid dissecting leiomyoma of the uterus. Int J Gynecol Pathol. 2013;32(2):215-20. doi: 10.1097/PGP.0b013e318257dff4 [ Links ]
14. Yu X, Fu J, Cao T, Huang L, Qie M, Ouyang Y. Clinicopathologic features and clinical outcomes of intravenous leiomyomatosis of the uterus: A case series. Medicine (Baltimore). 2021;100(1):e24228. doi: 10.1097/MD.0000000000024228 [ Links ]
15. Akkour K, Alhulwah M, Alqahtani N, Arafah MA. A giant leiomyoma with massive cystic hydropic degeneration mimicking an aggressive neoplasm: A challenging case with a literature review. Am J Case Rep. 2021;22:e929085. doi: 10.12659/AJCR.929085 [ Links ]
Statement on ethical issues
Ethical responsibilities: Protection of persons. We, the authors, declare that the procedures followed conformed to the ethical standards of the committee on responsible human experimentation and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality: The authors declare that we have followed the protocols of the Hospital Central "Dr. Urquinaona" on the publication of patient data.
Privacy rights and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Funding: The authors certify that we have not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the conduct of the study.
Received: August 03, 2021; Accepted: December 27, 2021; pub: August 22, 2022











 texto en
texto en 




