Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.2 Lima abr./jun. 2022 Epub 06-Jul-2022
http://dx.doi.org/10.31403/rpgo.v68i2412
Brief communication
Intrapartum endotracheal intubation in fetuses with airway obstruction. Two first cases of EXIT surgery at Hospital Rebagliati - EsSalud
1. Hospital Nacional Edgardo Rebagliati Martins, EsSalud, Lima, Peru
Two cases of pregnant women in the third trimester of gestation referred for management of fetal cervical tumor with airway obstruction are presented. The cases were scheduled for EXIT (ex-utero intrapartum treatment), fetal surgery which allowed controlled intrapartum orotracheal intubation avoiding the period of hypoxia and potential asphyxia that would occur with the conventional neonatal procedure. The neonates were subsequently operated on by head and neck surgeons for reduction of the cervical mass. It is suggested to consider this procedure in cases where severe airway obstruction is suspected and to refer them to centers that have a fetal surgery unit with a multidisciplinary medical team.
Key words: Lymphangioma; cervical; Teratoma; cervical; Surgery; fetal; EXIT surgical procedure
Introduction
Lymphangioma and cervical teratoma are the two most frequent fetal cervical tumors that cause severe airway obstruction and are associated with high neonatal mortality and morbidity1. The difficulty occurs at birth, as it is impossible to perform endotracheal intubation due to the obstructed airway. It is a real clinical challenge and many cases of neonatal death by asphyxia have been reported due to failure of orotracheal intubation2,3.
The EXIT technique (ex-utero intrapartum treatment) was designed in the 90's with the purpose of securing the neonatal airway in complicated cases4. The surgical and anesthetic technique allows oxygenation through the umbilical cord and placental circulation with the fetus exposed, to allow more time for endotracheal intubation5. To be able to perform it, an exact balance of a multidisciplinary team is needed.
Case reports
Case 1
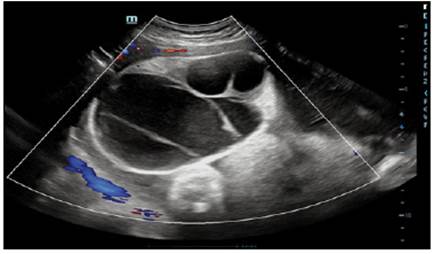
A 28-year-old primipara was referred from a private center at 36 weeks of gestation for presenting a fetal cervical tumor and airway obstruction, with significant growth in the last weeks. Ultrasound showed a multicystic cervical tumor measuring 169 x 118 mm, with severe airway obstruction and concomitant polyhydramnios (Figure 1).
Following a medical round with fetal medicine, obstetrics-gynecology, neonatology, head and neck surgery and anesthesiology, the EXIT surgery was scheduled urgently, as the patient went into labor. Anesthesia consisted in general inhalation anesthesia with dexamethasone premedication and intravenous induction with fentanyl, propofol and rocuronium. During the EXIT procedure, a maximum sevoflurane minimum alveolar concentration (MAC) of 2 was achieved to help relax the uterus and achieve adequate uteroplacental circulation. Pfannenstiel incision and Kerr hysterotomy were performed to exteriorize only the upper half of the fetus. Continuous irrigation of the uterine cavity with tempered 0.9% NaCl and clinical monitoring of the fetal heart rate was performed. The cystic tumor involved the entire anterior and lateral compartment of the fetal neck. Neonatology attempted to access the airway by endotracheal intubation, without success due to the large tumor mass, so the head and neck surgery team performed decompression of the tumor by aspiration of the cystic content, after which endotracheal intubation and cord ligation were performed (Figure 2). The total time of the utero-placental bypass was 21 minutes and the fetal heartbeat remained constant throughout the procedure.
After removal of the newborn, a safe airway was considered pertinent and a tracheostomy was performed following placement of an umbilical venous catheter, to provide analgesia with fentanyl and midazolam. The newborn weighted 3710 gram and was transferred to the neonatal ICU.
After six days he underwent excisional surgery by head and neck surgery. The pathology result was a lymphangioma. The evolution was unfortunately torpid, with recurrence of lymph filling and involvement of deep planes with subsequent sepsis and neonatal death.
Case 2
27-year-old pregnant woman referred from a private center at 37 weeks of gestation for presenting a fetal cervical lump and suspected airway obstruction. Ultrasound showed a cystic/solid cervical tumor measuring 12 x 9 cm with extension to the upper third of the thorax. The ultrasound and MRI findings are shown in Figure 3. The EXIT protocol was initiated by convening the multidisciplinary team according to case 1 described. The presence of an anterior and right lateral cervical tumor was noted. Endotracheal intubation was successful on the third attempt after partial decompression of the mass by aspiration by the head and neck surgery team (Figure 4).

Figure 3 Case 2: Ultrasound findings of fetal cervical tumor (cystic-solid) and fetal resonance highlighting deep plane involvement.
The total time of placental uterine bypass was 20 minutes. The fetal heartbeat, verified by ultrasound, remained constant during the procedure. The male newborn weighed 3260 grams and was transferred to the neonatal intensive care unit after the described airway approach. After twenty days he underwent excisional surgery by head and neck surgery, verifying infiltration from the right parotid region and floor of the mouth to the superior mediastinum and involving large vessels and nerve plexuses. The pathology result was a grade 2 immature teratoma, for which he was referred to pediatric oncohematology and is currently receiving satisfactory chemotherapy management (Figure 5).
Discussion
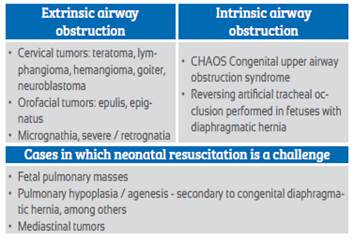
Fetal cervical tumors represent a rare pathology that can cause severe airway obstruction with fatal consequences for an otherwise healthy newborn. Once diagnosed, it is necessary to determine the extent of the mass and the level of airway compromise by ultrasound in expert hands and, if feasible, to complement with fetal MRI6. Although EXIT has several indications, the main one is when airway obstruction is suspected (Table 1).
The next step is to convene a multidisciplinary team composed of physicians specialized in fetal medicine, anesthesiologists, neonatologists, specialists in fetal airway management (head and neck surgeons, otolaryngologists, or pulmonologists) and nurses specialized in surgical center and neonatology5-7. Planning is fundamental and receiving this case in a tertiary center allowed us to have the necessary human and logistic tools. Mean gestational age considered in systematic reviews for delivery is 35 weeks, due to the high incidence of premature rupture of membranes or preterm delivery that occurs due to secondary polyhydramnios, as occurred in case 1, which limited the MRI study. Emergency surgeries should be avoided, due to the need of adequate implementation of the procedure8-10.
Once human resources and logistics have been secured, an intervention plan for the management of a difficult airway must be in place and known by each member of the team. Cruz and collaborators mention that such management should be planned from the least to the most invasive procedures, such as the need for tracheostomy, which according to a recent systematic review reaches 20%10 and was necessary in case 1.
The EXIT procedure is a surgery based on the maintenance of maternal-fetal circulation (utero-placental bypass) during cesarean delivery, which allows the necessary time to achieve a safe airway through procedures ranging from orotracheal intubation to excision of the obstructive lesion itself. In both cases the participation of head and neck surgeons was required for decompression by tumor aspiration, due to the difficulty in accessing the airway.
The anesthetic technique is aimed at avoiding uterine contractions and placental abruption and maintaining fetal respiration. General anesthesia is indispensable. In both cases, for the inhibition of fetal respiration we proceeded to induction with general anesthesia reinforced with fentanyl, propofol and rocuronium. Once the fetal extraction was performed only up to half of the dorsum, keeping the rest of the body in utero, the inhibition of contractions was achieved with an inhalation anesthetic (sevoflurane). Currently, it has been proven that the administration of halogenated anesthetics at analgesic doses of 0.5 to 1 CAM with or without N2O does not have a major impact on the neonate or on uterine contraction2. Regarding fetal cardiac monitoring, ultrasound and clinical monitoring have been described. In case 1 clinical monitoring was chosen due to the urgency of the case, while for case 2 the registry was under ultrasound guidance. To avoid intrauterine compression of the umbilical cord, the umbilical cord was irrigated with tempered NaCl 0.9/oo by means of a Nélaton probe. During the EXIT procedure, one of the main complications is hysterotomy bleeding, for which it is necessary to perform clamping of the angles. The use of surgical clamps has been described11; in our case, foester clamps were used in the angles.
Regarding access to the airway, in most cases endotracheal intubation is difficult due to tumor obstruction12,13. In both cases, it could not be achieved in the first attempt due to the large tumor mass, so head and neck surgery decompressed the tumor by aspiration of its liquid content. Cases of instability of the cannula have been described making it necessary to secure the airway; in case 1, tracheostomy was performed due to a drop in saturation despite intubation.
In the management of a congenital tumor that compromises access to the airway, it is very important to have a multidisciplinary team and the necessary materials to avoid the morbidity and mortality associated with this scenario3,6. Although both patients were referred late, the intervention was possible thanks to the optimal and satisfactory organization of the entire surgical team. Referral of these cases to a tertiary center with resolution capacity should be made as soon as the diagnosis is made, in order to implement the case protocol, which includes a complete fetal morphological study, mapping of the extension and invasion of the lesion by ultrasound and magnetic resonance imaging, if necessary, and convene the multidisciplinary team for the performance of a scheduled procedure. We believe it is convenient to add this case to those already reported in the national literature2,3,14, as well as to disseminate that this specialized procedure is currently performed by the fetal surgery unit of our hospital in EsSalud. It is necessary to promote and strengthen timely diagnosis and referral to ensure timely and comprehensive care of both the mother and the newborn.
REFERENCES
1. Ösgünen TF, Gülec ÜK, Evrüke IC, Demir SC, Büyükkurt S, Yapicioglu H, Ískit S. Fetal oropharyngeal and neck tumors: Determination of the need for ex-utero intrapartum treatment procedure. Balkan Med J. 2015 Apr 1;32(2):221-5. doi: 10.5152/balkanmedj.2015.150096 [ Links ]
2. Alegría-Guerrero R, Ventura-Laveriano W. Linfangioma cervical: intubación exútero intraparto EXIT. Rev Peru Investig Matern Perinat. 2019;7(1):62-7. doi:10.33421/inmp.2018110 [ Links ]
3. Huerta-Sáenz I, Elías-Estrada J. Linfangioma cervical fetal: diagnóstico prenatal y resultado perinatal. Rev Peru Ginec Obstet. 2012;58(4):347-50. doi:10.31403.rpgo.v58i52 [ Links ]
4. Ore Acevedo J, Alvarado Zelada J. Procedimiento EXIT para tumores y quistes de cabeza y cuello. Prog Obstet Ginecol. 2018;61(6):589-93. Recuperado de: https://medes.com/publication/142194 [ Links ]
5. Abraham RJ, Sau A. A review of the EXIT (Ex utero Intrapartum Treatment) procedure. J Obstet Gynaecol. 2010 Jan;30(1):1-5. doi: 10.3109/01443610903281656 [ Links ]
6. Cruz-Martínez R, Méndez A. Técnica EXIT (Ex Utero Intrapartum Treatment): indicaciones, limitaciones, riesgos y evolución a la técnica de intubación traqueal fetal endoscópica (FETI). Ginecol Obstet Mex. 2015;83:58-65. PMID: 26016317. [ Links ]
7. Bence CM, Wagner AJ. Ex utero intrapartum treatment (EXIT) procedures. Semin Pediatr Surg. 2019;28(4):150820. doi:10.1053/j.sempedsurg.2019.07.003 [ Links ]
8. Liao AY, Levin B, Daniel M, Chan L, Cooper MG, Birman CS. Emergency EXIT: an urgent ex utero intrapartum tracheostomy for giant fetal neck mass. ANZ J Surg. 2013;83(9):684-5. doi: 10.1111/ans.12316 [ Links ]
9. Lo RH, Mohd NKN, Abdullah K, Aziz A, Mohamad I. Ex utero intrapartum treatment (EXIT) of gigantic intrapartum lymphangioma and its management dilemma - A case report. Medeni Med J. 2020;35(2):161-5. doi: 10.5222/MMJ.2020.06992 [ Links ]
10. Novoa RH, Quintana W, Castillo-Urquiaga W, Ventura W. EXIT (ex utero intrapartum treatment) surgery for the management of fetal airway obstruction: A systematic review of the literature. J Pediatr Surg. 2020;55(7):1188-95. doi: 10.1016/j.jpedsurg.2020.02.011 [ Links ]
11. Ogamo M, Sugiyama T, Maeda Y, Kusaka H, Utsunomiya H, Tsubouchi M, Uchida K, Sasaki N, Mitani Y, Komada Y, Toyoda N. The ex utero intrapartum treatment (EXIT) procedure in giant fetal neck masses. Fetal Diagn Ther. 2005 May-Jun;20(3):214-8. doi: 10.1159/000083908 [ Links ]
12. Butler CR, Maughan EF, Pandya P, Hewitt R. Ex utero intrapartum treatment (EXIT) for upper airway obstruction. Curr Opin Otolaryngol Head Neck Surg. 2017 Apr;25(2):119-26. doi: 10.1097/MOO.0000000000000343 [ Links ]
13. García-Díaz L, Chimenea A, de Agustín JC, Pavón A, Antiñolo G. Ex-Utero Intrapartum Treatment (EXIT): indications and outcome in fetal cervical and oropharyngeal masses. BMC Pregnancy Childbirth. 2020 Oct 7;20(1):598. doi: 10.1186/s12884-020-03304-0 [ Links ]
14. Ventura Laveriano W. Huertas Tacchino E. Intubación endotraqueal intraparto en un feto con hernia diafragmática. A propósito de la primera cirugía fetal EXIT (ex-utero intrapartum treatment) en el Perú. Rev Peru Ginec Obstet. 2015;61(4):417-21. Doi: 10.31403/rpgo.v61i1874 [ Links ]
Cite as: Huerta Sáenz IH, Elías Estrada JC, Arce Villavicencio R, Carbajal Peves M, Romero Chauca CJ, Manosalva Lozano G. Intrapartum endotracheal intubation in fetuses with airway obstruction. Two first cases of EXIT surgery at Hospital Rebagliati - EsSalud. Rev Peru Ginecol Obstet. 2022;68(2). DOI: https://doi.org/10.31403/rpgo.v68i2412
Received: January 21, 2022; Accepted: February 25, 2022











 texto en
texto en