Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.2 Lima abr./jun. 2022 Epub 06-Jul-2022
http://dx.doi.org/10.31403/rpgo.v68i2419
Case report
Postpartum hypervascular placental polyp
1Specialist in Gynecology and Obstetrics. Obstetrics and Gynecology Service, Hospital Central "Dr. Urquinaona", Maracaibo, Zulia State, Venezuela
Placental polyp is a tumor of placental tissue retained within the endometrial cavity. These retained placental tissue fragments, especially those of the hipervascular type, are a possible cause of acute bleeding for an indefinite period after abortion or delivery. These retained placental tissue fragments, composed predominantly of necrotic and hyalinized chorionic villi, give it its hipervascular condition and can cause profuse, life-threatening hemorrhage and require immediate intervention based on the correct differential diagnosis. We present a case of a 45-year-old woman with genital bleeding. The last pregnancy had been 6 years ago. Ultrasonography revealed an intrauterine and echogenic tumor measuring 3 x 2 x 1 centimeters with multiple cystic spaces inside. She underwent successful hysteroscopy-guided resection, and the pathological diagnosis was hipervascular placental polyp. Although rare, placental polyp should be considered as one of the causes of postpartum genital bleeding.
Key words: Placenta; polyp; hemorrhage.
INTRODUCTION
Placental polyp is a tumor arising from placental fragments within the uterine cavity after abortion or childbirth1,2. Clinical history and physical examination, together with serum concentrations of human chorionic gonadotropin and color Doppler ultrasonography, allow an accurate diagnosis of this clinical entity. Conservative treatment can be practiced with hysteroscopic resection, while hysterectomy is indicated in cases of incoercible vaginal bleeding3. A case of postpartum hypervascular placental polyp is presented.
CASE REPORT
This was a 45-year-old patient, gestation 3, para 3, who consulted for presenting vaginal bleeding in moderate to abundant quantity, bright red in color without clots, of approximately 4 days of evolution. She had a history of bleeding 3 months earlier, so a commercial pregnancy test was performed with negative results and ultrasound findings reported endometrial hyperplasia. She had her menarche at 13 years of age with regular menstrual intervals lasting 3 to 5 days. The last menstrual period had been 6 months prior to the present illness. Both deliveries had been vaginal, the last one 6 years ago, without complications. The patient denied any important personal or family history.
On physical examination on admission the patient was conscious with moderate cutaneous-mucosal pallor, afebrile (36.7ºC), hydrated, and oriented, with blood pressure of 110/65 mmHg, heart rate of 102 beats per minute and respiratory rate of 19 breaths per minute. The abdomen was soft, depressible, non-painful, with no palpable tumors. The external genitalia were normal, normal vagina with intrapelvic uterus, without adnexal tumors or pain on movement. On speculoscopy, the external cervical os was closed and smooth with evidence of moderate genital bleeding.
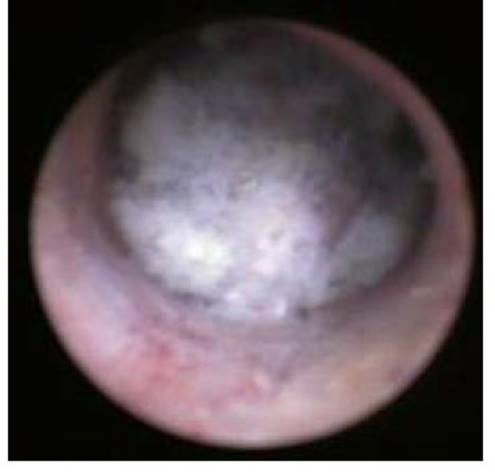
Laboratory test results showed hemoglobin of 9.1 g/dL, hematocrit of 29%, with white count of 9,600 cells/mL, neutrophils 73% and lymphocytes 26%. The chorionic gonadotropin determination was 90 IU/L. Transvaginal ultrasound showed intrauterine and echogenic tumor of 3 x 2 x 1 centimeters with multiple hypoechogenic spaces inside and pedicle of 1 x 1 centimeter without endometrial involvement (Figure 1). The Doppler ultrasound study showed peripheral vascularization with pulsatility index of 0.35 and resistance of 0.29. In view of the findings, the possibility of placental polyp was considered.
The patient underwent hysteroscopic guided resection with subsequent uterine curettage under anesthesia. The tumor measured approximately 6 x 6 x 3 centimeters with a polypoid characteristic and a wide base fixed to the posterofundal uterine wall (Figure 2), which was removed in its entirety. The patient tolerated the procedure well. During the postoperative period there were no complications, and she was discharged on the second postoperative day.
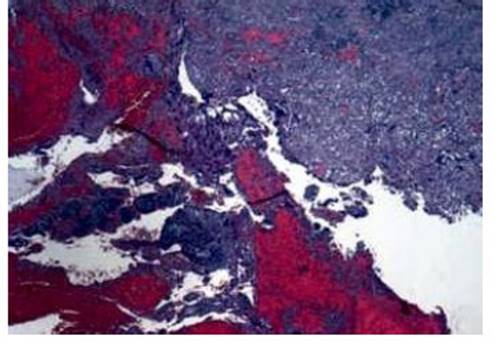
Microscopic section of the lesion fragments revealed immature placental tissues without necrotic areas with chorionic villi with fibrosis, small portions of cytotrophoblast and abundant syncytiotrophoblast with hemorrhages, without necrotic areas and prominent large caliber blood vessels (Figure 3). Fragments of endometrium in proliferative phase with abundant glands were observed. The final histopathologic report was decidual and immature placental tissue and secretory endometrium.
DISCUSSION
Placental polyps were first described in 1884, in a case occurring 12 years after delivery3. Retention of placental tissue fragments, particularly those of the hypervascular type, is a common cause of vaginal bleeding during the puerperium
Postpartum hypervascular placental polyp and occasionally months or years after abortion or delivery, whose main characteristic is profuse hemorrhage requiring the use of blood products, hysteroscopic resection and hysterectomy to avoid death. It may occur in about 0.25% of pregnancies4,5.
They occur most frequently after therapeutic or induced abortion and spontaneous delivery, and there are only a few case reports published in the literature after spontaneous abortion3. Other risk factors identified include Müllerian abnormalities contributing to abnormal placentation and in patients with a history of placental accreta combined with uterine atony6,7. There are also reports describing that they can arise from the placental insertion site and in patients with a history of pelvic radiation treatment during childhood8,9. Pregnancies obtained by assisted reproductive techniques are also associated with the occurrence of the condition, as one review noted that these patients have 20 times the risk of placental polyps compared to controls. This may be due to endometrial disorders leading to abnormal placentation, with altered decidualization and abnormal trophoblast invasion. In addition, excessive exposure to gonadotropin, estrogens and progestins may also induce morphological and structural changes that alter endometrial gene expression10.
Due to their potentially life-threatening nature, clinical suspicion and prompt and early diagnosis is essential to avoid hemorrhagic complications caused by placental polyps. Clinical manifestations include genital bleeding (up to 72% of cases) and pelvic pain, but some cases may be asymptomatic and detected by ultrasound. The pathogenic mechanisms causing the bleeding are the preservation of the brush border of the syncytiotrophoblast (together with the presence of placental phosphatase) which maintains the anticoagulant properties of the villi. This occurs in cases of post-abortion hemorrhage. The thromboplastic properties of necrotic villi with epithelial debris also play an important role in genital hemorrhage5.
Chorionic gonadotropin concentrations are useful in the differential diagnosis with other intrauterine conditions, such as gestational trophoblastic disease. However, they are not useful in other conditions, such as retained ovarian debris, placenta accreta or arteriovenous malformations11. Typical ultrasound findings show endometrial tumor that may be polypoid, solid, cystic, or heterogeneous, with multiple scattered anechoic areas of variable size. Doppler ultrasound is useful to detect hypervascular lesions. In addition, it allows examining the implantation site, blood supply and planning the extraction10. MRI shows similar results to Doppler ultrasound but is more expensive and difficult to use. However, it can identify the degree of myometrial involvement and monitor size after expectant management. Computed tomography angiography allows evaluation of neovascularization, especially in patients in whom conservative treatment is considered to preserve fertility, since it allows selective catheterization of the vessel supplying the tumor12.
From the clinical point of view, placental polyps can be divided into two types: acute and chronic. Acute polyps usually appear days or weeks after the abortion or delivery, while chronic polyps are not detected for months or even years4. The present case can be classified as chronic type polyps because the vaginal bleeding occurred 6 years after vaginal delivery at term. However, there are three types of polyps based on histological and immunohistochemical findings: with preserved villi, clusters of degenerated villi and isolated cotyledons. Those that appear after delivery have more fibrosis, while those that occur after abortion contain more syncytiotrophoblasts and cytotrophoblasts.
Hypervascularization is due to the ability of the syncytiotrophoblast to stimulate neovascularization after the end of pregnancy. Initially degeneration appears with appearance of fibrin deposits and inflammatory changes, whereby the tissue forms a polyp that is interlaced with large caliber blood vessels. Then there is infiltration of blood into the tissue leading to further accumulation of fibrin and blood clots8. Partially hyalinized and thrombosed vessels cannot contract, leading to hemorrhage, and the enzymatic activity of syncytiotrophoblast and its local anticoagulant effect further accentuate the tendency to hemorrhage4,13,14. This differentiates placental polyps from placental remnants, since the polyp adheres to the endometrium and invades the Nitabuch's layer, firmly including the myometrium8.
There is no consensus regarding the treatment of placental polyps. However, with the advance of diagnostic and therapeutic procedures, there is evidence of success of conservative management with chemotherapy, hysteroscopic resection and uterine artery embolization or the combination of these procedures15. Hysteroscopic resection is the alternative to traditional sharp curettage since it allows complete resection with direct visualization and a low rate of complications. Its success rate is close to 95%. Arterial embolization decreases the blood supply and minimizes the risk of hemorrhage when performed before hysteroscopic resection. However, embolization may increase the risk of placental accreta in subsequent pregnancies and negatively affect ovarian reserve. In addition, because of the risks of uterine ischemia and infection, it may not be an option in patients who desire new pregnancies5. Methotrexate chemotherapy is promising, as it reduces the blood supply to the polyp prior to hysteroscopic resection. Methotrexate not only stops cell division, but also decreases syncytiotrophoblast activity, directly inhibiting neovascularization10.
In conclusion, hypervascular placental polyps are a cause of genital bleeding after spontaneous abortion, months after induced abortion or years after spontaneous vaginal delivery. Clinical history, physical examination, along with chorionic gonadotropin concentrations and Doppler ultrasonography aid in the diagnosis of this condition. Treatment options for those cases with incoercible genital bleeding include use of methotrexate, hysteroscopic resection, embolization of the arteries and/or hysterectomy.
REFERENCES
1. Matsubara S, Takahashi H, Suzuki T. Retained placenta accreta with marked vascularity, uterine artery pseudoaneurysm, and placental polyp: overlapping clinical entities? Arch Gynecol Obstet. 2018;297(1):269-70. doi: 10.1007/s00404017-4589-0 [ Links ]
2. Ishihara T, Kanasaki H, Oride A, Hara T, Kyo S. Differential diagnosis and management of placental polyp and uterine arteriovenous malformation: Case reports and review of the literature. Womens Health (Lond). 2016;12(6):538-43. doi: 10.1177/1745505717692590 [ Links ]
3. Shiina Y. Overview of neo-vascular lesions after delivery or miscarriage. J Clin Med. 2021;10(5):1084. doi: 10.3390/jcm10051084 [ Links ]
4. Goda M, Suzuki T, Adachi H. Placental polyp with arteriovenous malformation treated with a gonadotropin-releasing hormone antagonist. BMJ Case Rep. 2021;14(9):e244664. doi: 10.1136/bcr-2021-244664 [ Links ]
5. Behnamfar F, Zadeh FM, Hashemi L. A case of placental polyp after normal vaginal delivery. J Res Med Sci. 2014;19(7):680-2. PMC4214030. PMID: 25364371 [ Links ]
6. Jiménez JS, Gonzalez C, Alvarez C, Muñoz L, Pérez C, Muñoz JL. Conservative management of retained trophoblastic tissue and placental polyp with diagnostic ambulatory hysteroscopy. Eur J Obstet Gynecol Reprod Biol. 2009;145(1):89-92. doi: 10.1016/j.ejogrb.2009.04.001 [ Links ]
7. Sorano S, Fukami T, Goto M, Imaoka S, Ando M, To Y, et al. Choosing the uterine preservation surgery for placental polyp determined by blood flow evaluation: A retrospective cohort study. Ann Med Surg (Lond). 2017 Sep 28;23:13-6. doi: 10.1016/j.amsu.2017.09.008 [ Links ]
8. Di Serio M, Capozzi VA, Berretta R, Marcato C, Dall'Asta A, Frusca T. Conservative treatment for hypervascularised placental polyp with secondary haemoperitoneum: a case report. Acta Biomed. 2021;92(S1):e2021157. doi: 10.23750/abm.v92iS1.9559 [ Links ]
9. Watanabe N, Tsutsui J, Kakiuchi S, Jwa SC, Takahashi H, Kato N, et al. Intra-abdominal bleeding during pregnancy, preterm delivery, and placental polyp in a long-term survivor of neuroblastoma: A case report. Obstet Gynecol Int. 2009;2009:564567. doi: 10.1155/2009/564567 [ Links ]
10. Baba T, Endo T, Ikeda K, Shimizu A, Morishita M, Kuno Y, et al. Assisted reproductive technique increases the risk of placental polyp. Gynecol Endocrinol. 2013;29(6):611-4. doi: 10.3109/09513590.2013.788636 [ Links ]
11. Shanthi V, Rao NM, Lava nya G, Krishna BA, Mohan KV. Placental polyp a rare case report. Turk Patoloji Derg. 2015;31(1):77-9. doi: 10.5146/tjpath.2014.01226 [ Links ]
12. Shiina Y, Itagaki T, Ohtake H. Hypervascular retained product of conception: Characteristic magnetic resonance imaging and possible relationship to placental polyp and pseudoaneurysm. J Obstet Gynaecol Res. 2018;44(1):165-70. doi: 10.1111/jog.13481 [ Links ]
13. Woo J, Kahn B. Enhanced myometrial vascularity: case presentation and review. Fertil Steril. 2021;116(3):912-4. doi: 10.1016/j.fertnstert.2021.05.097 [ Links ]
14. O'Leary M, Sanders AP. Enhanced myometrial vascularity-the time has come for individualized treatment of focal uterine pathology. Fertil Steril. 2021;116(3):691-2. doi: 10.1016/j.fertnstert.2021.06.059 [ Links ]
15. Mori M, Iwase A, Osuka S, Kondo M, Nakamura T, Nakahara T, et al. Choosing the optimal therapeutic strategy for placental polyps using power Doppler color scoring: Transarterial embolization followed by hysteroscopic resection or expectant management? Taiwan J Obstet Gynecol. 2016;55(4):534-8. doi: 10.1016/j.tjog.2014.12.016 [ Links ]
Declaration of ethical aspects
Ethical responsibilities: Protection of persons. We the authors declare that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Confidentiality of data: The authors declare that we have followed the protocols of the Hospital Central "Dr. Urquinaona" on the publication of patient data.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Funding: The authors certify that we have not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the realization of the study.
Received: November 19, 2021; Accepted: March 01, 2022











 texto en
texto en