Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.3 Lima jul./sep. 2022 Epub 22-Sep-2022
http://dx.doi.org/10.31403/rpgo.v68i2429
Original paper
Cervical vascularization low he in the prediction of imminent preterm labor
1. Specialist in Gynecology and Obstetrics. Attending Physician, Gynecology and Obstetrics Department, Central Hospital “Dr. Urquinaona”, Maracaibo, Venezuela
2. Professor, Faculty of Medicine, Universidad del Zulia. Maracaibo, Venezuela
Objective:
To establish the usefulness of cervical vascularization low he in the prediction of impending preterm labor.
Participants:
Patients with preterm delivery within 7 days (group A) and pregnant women with preterm delivery beyond 7 days (group B).
Main outcome measures:
General characteristics, cervical vascularity low he (vascularity index, low index and vascularity / low index), impending preterm delivery, and prognostic efficacy.
Results:
A total of 350 patients were included, 75 women presented imminent preterm labor (group A) and 251 patients were considered as controls (group B). Patients in group A had significantly lower values of vascularization index and low index compared to group B (p = 0.0122 and p < 0.0001, respectively). Patients in group B had significantly higher values of vascularization / low index compared to patients in group A (p = 0.0103). The three low he and the combination of these did not show the ability to discriminate imminent preterm labor.
Conclusions:
Patients with imminent preterm labor showed significant differences in the vascularization low he compared to patients presenting preterm labor beyond 7 days of ultrasound evaluation. However, they are not useful in predicting impending preterm labor.
Key words: Cervix uteri, blood low, Cervical vascularization indexes; Obstetric labor, premature, prediction
Introduction
Preterm delivery is the leading cause of perinatal morbidity, affecting between 7% and 11% of all pregnancies. It is also low he s n for more lo half of the incidence of neonatal mortality1,2. The exact mechanisms that produce it remain unknown3. Identification of risk factors and prevention of prematurity are important low of research in obstetrics4. However, despite improvements in diagnosis and treatment, the prevalence has not decreased in the last two decades5.
Both uterine contractions and cervical changes precede the development of preterm labor. Different studies have attempted to identify early the different cervical changes as predictors6,7. Cervical ultrasonography is a reliable and objective way of cervical evaluation and ultrasonographic measurement of cervical length has proven to be a useful screening test and is becoming a routine evaluation in the care of pregnant women at high risk for obstetric complications6-9. However, despite its high clinical predictive value, it has low sensitivity7,10. Therefore, it is necessary to investigate other cervical parameters with better predictive capabilities.
Three-dimensional ultrasound has the potential to provide more accurate measurements lo conventional two-dimensional ultrasound and combined with power Doppler can provide angiography-like information on cervical vascular architecture11. This imaging technique allows evaluation of both blood low and vascularization by calculating vascular low he using the program VOCAL (Virtual Organ Computer-Aided Analysis), which has been used in different studies in obstetrics12-14. However, there is limited research evaluating the cervix during pregnancy with this type of technique15,16. Although a previous study showed that cervical vascular low he remained stable throughout normal pregnancy16, there is low h information on the potential changes of these parameters in determining the risk of imminent preterm delivery in high-risk patients.
The aim of this study was to establish the usefulness of cervical vascularization low he in the prediction of impending preterm delivery.
Methods
This was a prospective study conducted at the Hospital Central “Dr. Urquinaona”, Maracaibo, Venezuela, from June 2014 to October 2021. For this purpose, women with singleton pregnancies between 24 and 35 weeks determined by ultrasound at the beginning of the second low he s, with clinical diagnosis of threatened preterm labor, with up to 3 uterine contractions in 30 minutes, cervical dilatation lo lo 3 centimeters by physical examination, effacement lo lo 80% and intact low he s were consecutively selected and evaluated. The study was approved by the institutional review board of La Universidad del Zulia and the Ethics Committee of the hospital. Written informed consent was obtained at the time of selection of each participant for the study.
Exclusion low he were: multiple pregnancies, history of progesterone or any other tocolytic use in the current pregnancy, known cervical insufficiency or history of low he , premature low he of low he s, uterine anomalies, abnormal placentation, maternal cardiac alterations, active inflammatory or infectious disease, hypertension and pregestational or gestational diabetes, intrauterine growth restriction of the fetus, congenital fetal anomalies, alterations in amniotic fluid low he, acute low he s nitis and unknown gestational age. Patients who refused to participate were also excluded from the study.
Within one hour of hospital admission and prior to the start of any treatment, participants underwent examination of the cervix with a sterile speculum, performing the fern and nitrazine paper tests to rule out low he of low he s. Immediately afterwards, a digital examination was performed by the on-call staff and confirmed by one of three investigators after this evaluation, to define dilatation, maturation, consistency and position of the cervix, in addition to fetal wedging for calculating Bishop’s score. They then underwent transabdominal fetal ultrasound evaluation to determine fetal presentation, placental insertion site, measurement of fetal head and abdominal circumference, femur length and amniotic fluid index. Subsequently, continuous fetal heart rate monitoring and observation of the characteristics of uterine contractions by external tocodynamometry were initiated.
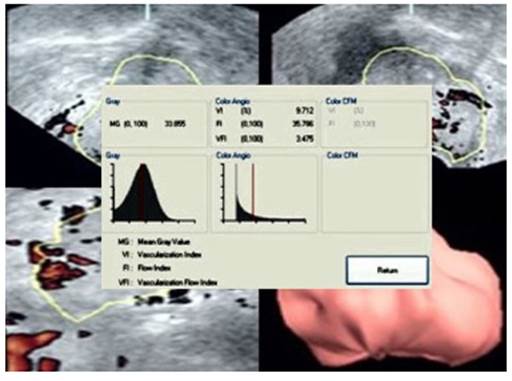
Cervical three-dimensional scanning was performed with the Voluson 730 Expert ultrasound machine (Diamond II, GE Medical Systems, Milwaukee, WI, USA) equipped with 5 to 9 MHz three-dimensional transvaginal transducer. A pillow was placed under the pregnant woman’s buttocks to prevent rectal gas from obscuring the outer cervix. low he evaluation of cervical vascularity, the power Doppler settings in the evaluations were: frequency 3 to 9 MHz, gain -5.0, pulse repetition frequency 0.6 kHz and motion filter ‘below 1’. After drawing the cervical contours while the view was rotated by 30° automatically to minimize post-processing time, 6 cervical contours were obtained (Figure 1). The cervical image was magnified to occupy more lo 70% of the screen size. The VOCAL program calculated the vascularization index (VI), low index (FI) and vascularization/ low index (VFI). The IV reflects the density of the blood vessels, the IF the energy reflected by the blood corpuscles within the vessels, and the IVF, the density of the blood vessels and the number of blood corpuscles flowing in the vessels17.
All ultrasound measurements were performed by a single specialist in maternal-fetal medicine who was part of the research team and who was not involved in the clinical care of the participants. The duration of the evaluation was less than 10 minutes in all cases and the members of the hospital team performing the care were unaware of the results. Therefore, the ultrasound measurements did not influence the management of the participants.
Initially, all selected pregnant women were admitted for treatment with bed rest in left lateral decubitus and hydrated with 500 mL of lactated Ringer's solution. If progressive cervical changes were documented or contractions persisted for at least 2 hours after treatment, they were hospitalized and tocolytic treatment was initiated, with calcium channel blockers as first-line therapy. During hospitalization, two 12-mg doses of intramuscular betamethasone were administered at 24-hour intervals to induce fetal lung maturation. Tocolytics were discontinued 48 hours after the first steroid dose. Neither tocolytics nor steroids were used in pregnancies older than 35 weeks.
A form was prepared that included the following data: identification number, maternal age, gestational age at the time of examination, parity, presence of bleeding, history of preterm delivery, digital cervical examination with determination of dilation and effacement, station and consistency and cervical position and cervical vascularization values. The main study variable was the frequency of imminent delivery (that which occurred within 7 days of the evaluation). Data on birth weight and time interval between the evaluation and delivery were also included. All data were recorded and stored for subsequent analysis.
Data distribution was evaluated according to the Shapiro-Wilk normality test. Categorical variables were analyzed using the chi-square test or Mann-Whitney U test. Continuous variables with normal distribution were compared with Student's t test. Those variables with non-normal distribution were compared with the Wilcoxon rank sum test. Operator-receptor curves were used to determine the best cutoff point and to evaluate the diagnostic accuracy of vascularization indices in predicting preterm delivery within 7 days of evaluation. Sensitivity, specificity, negative predictive value, positive predictive value, and positive and negative likelihood ratios with their 95% confidence intervals in the prediction of impending preterm delivery were calculated for the optimal cutoff based on the response operator curve (ROC). The optimal cutoff was that corresponding to the point on the curve furthest from the reference line. The alpha level of statistical significance was p < 0.05. All analyses were performed with the SPSS® version 22.0 statistical package (SPSS Inc., USA).
Results
A total of 350 patients with symptomatic preterm labor were consecutively selected, of which 26 were excluded from the investigation (10 patients were diagnosed with hemorrhage in the second half of pregnancy, 7 women had premature rupture of membranes, 5 cases were diagnosed with preeclampsia and 4 patients had incomplete data during the evaluation). Therefore, for the final analysis, data from 326 patients were analyzed, of which 75 cases (23.0%) had imminent preterm labor (group A) and 251 patients (77.0%) delivered after 7 days (group B).
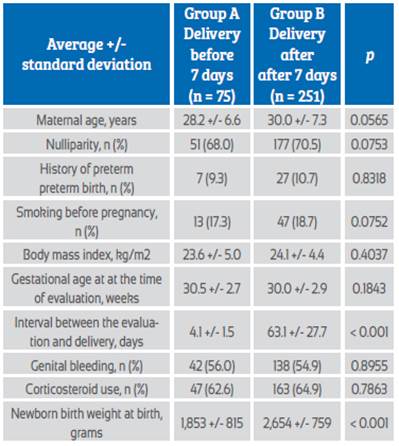
Table 1 shows the general characteristics of the patients in each study group. Patients in both groups had no significant differences in maternal age, nulliparity, history of smoking before pregnancy, body mass index, gestational age at evaluation, frequency of genital bleeding, and corticosteroid use (p = ns). Patients in group A had a shorter interval between ultrasound evaluation and delivery compared to patients in group B (4.1 +/- 1.5 days compared to 63.1 +/- 27.7 days, p < 0.0001). Significant differences were also found in newborn birth weight (p < 0.0001).
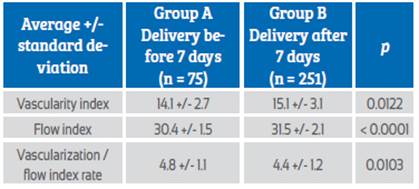
Regarding vascularization indices (Table 2), patients in group A showed significantly lower values of VI and FI compared to group B (p = 0.0122 and p < 0.0001, respectively). Patients in group B had significantly higher values of VFI compared to patients in group A (p = 0.0103). Differences in assessed values between groups showed no differences after adjusting for maternal age, body mass index and gestational age at the time of evaluation (p = ns).
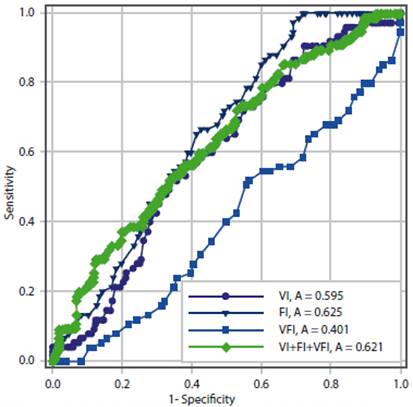
Table 3 and Figure 2 show the prognostic ability measurements of the different cervical vascularization indices in the prediction of impending labor in symptomatic patients. The VI (area under the curve 0.595, 95% confidence interval, 0.510 to 0.679), FI (area under the curve 0.652, confidence interval 0.551 to 0.753), VFI (area under the curve 0.401 (0.329 to 0.474) and the combination of the three indices (area under the curve 0.621, 95% confidence interval 0.527 to 0.716) did not show discriminatory capacity for imminent preterm delivery by presenting a value below the cutoff value of 0.750 (p = ns).
Table 3 Predictive ability of vascularization indices and cervical volume for imminent delivery in symptomatic patients.
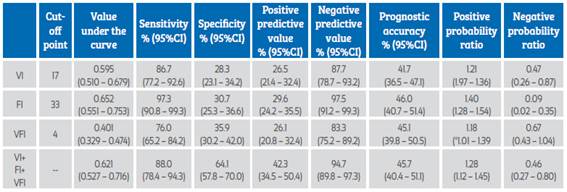
VI=vascularization index, FI=flow index, VFI=vascularization/flow index.
Discussion
Several ultrasound techniques are currently available for evaluation of the characteristics of the pregnant cervix, including two-dimensional and three-dimensional ultrasound. However, ultrasound measurement of cervical length can predict the development of preterm labor, depending on the selected cutoff point, with sensitivity values between 68% and 100% and specificity values of 44% to 79%18. But, this technique has some limitations when used as the only screening test, due to its low sensitivity and low positive predictive value19. Therefore, it is very useful to have new cervical characteristics and parameters to identify pregnant women with short cervix who are at real risk of preterm delivery. Though, research results demonstrate that cervical vascularization indicators (VI, FI and VFI) are not useful in predicting preterm delivery within 7 days of ultrasound evaluation in symptomatic patients.
There are few studies that evaluate changes in cervical vascularization during pregnancy using three-dimensional ultrasound, power Doppler angiography and the VOCAL method15,20. Angiogenic factors appear to play a key role in both cervical maturation and the delivery process, so it is possible that vascular indices could be used to identify changes prior to cervical modifications and delivery, either preterm or at term21. Some reports have proposed that cervical vascular parameters could be useful to accurately establish which pregnant women are at risk of going into labor. In addition, it has been shown that these vascular indices have constant distributions throughout normal pregnancy and their values do not show changes related to gestational age16.
In contrast to the results of this investigation, a previous study evaluated the vascularization values in patients with preterm delivery and found that the values were similar to those of patients who delivered at term22. The authors proposed that this could be due to methodological deficiencies of the study or perhaps that the method only could detect significant changes in vascularization20. However, another study showed increased vascularization and blood flow intensity in asymptomatic women with short neck in response to increased vessel number, flow volume and/or erythrocyte density. In addition, the FI was higher in asymptomatic women23. These results indicate that cervical vascularization and blood flow change in preparation for delivery.
The possible explanation for the findings of this research is that cervical changes produce alterations in the density of small cervical vessels, characterized by changes in their quantity accompanied by a decrease in red blood cells and backscatter energy. On the other hand, FI is not an perfusion indicator and does not provide information on the volume of blood passing through the vessel in a given period, making it less reliable than VI and VFI24. Although the results of this research suggest that cervical vascularity is somewhat related to cervical ripening in preterm pregnancies, this is a complex method that does not provide substantial benefits to simpler evaluations such as Bishop's score or cervical length alone.
Since the process of cervical modification leading to delivery may be affected by different factors related to cervical morphology, additional measurements may be useful to improve the accuracy of screening for preterm delivery25,26. However, multiparity, previous cervical surgical procedures, or infection may result in alterations of cervical morphologic characteristics27. Similarly, factors that are likely to affect the results of three-dimensional power Doppler indices are: pressure exerted by the transducer on the cervical tissue during evaluation, uterine contractions that have effects on blood flow velocity, and physiological changes in cervical blood circulation during scanning28,29. In addition, there are other important technical factors, such as the angle of insonation of the ultrasound waves. Although power Doppler ultrasound is independent of the insonation angle, this is not entirely true. The ultrasound beam incident on the bloodstream at a 90° angle will not generate any evidence of a Doppler wave30. Therefore, small changes in transducer position may produce differences in cervical flow power signals. In addition, there may be difficulties in defining the boundaries of the cervix, the lower uterine segment and the vagina. These difficulties have been described by other investigators who evaluated the cervix by three-dimensional ultrasound31.
This study has several strengths. It is the investigation with the largest number of patients with a diagnosis of preterm labor known to date using this imaging technology and included symptomatic pregnant women at high risk of imminent labor.
Limitations include that the VOCAL evaluation technique used in this study can be difficult to apply due to technical requirements, which can lead to inaccurate calculations, thus requiring staff training and high-resolution equipment. Another drawback of the use of this ultrasound technique is its high cost and limited availability in non-specialized care centers. Finally, the lack of standardization may hinder the correct extrapolation of the results to other at-risk populations.
In conclusion, patients with imminent preterm labor present significant differences in vascularization indices compared to patients with preterm labor beyond 7 days of ultrasound evaluation. However, they are not useful in predicting imminent preterm labor.
REFERENCES
1. Yu X, He C, Wang Y, Kang L, Miao L, Chen J, et al. Preterm neonatal mortality in China during 2009-2018: A retrospective study. PloS One. 2021;16(12):e0260611. Doi: 10.1371/journal.pone.0260611 [ Links ]
2. Mwita S, Konje E, Kamala B, Izina A, Kilonzo S, Kigombola A, et al. Association between antenatal corticosteroid use and perinatal mortality among preterm births in hospitals in Tanzania. PloS One. 2021;16(7):e0254916. Doi: 10.1371/journal.pone.0254916 [ Links ]
3. Son M, Miller ES. Predicting preterm birth: Cervical length and fetal fibronectin. Semin Perinatol. 2017;41(8):445-51. Doi: 10.1053/j.semperi.2017.08.002 [ Links ]
4. Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic low he with implications for the Sustainable Development Goals. Lancet. 2016;388(10063):3027-35. Doi: 10.1016/S0140-6736(16)31593-8 [ Links ]
5. Wu XP, Gu CL, Han SP, Deng XY, Chen XQ, Wang HY. A multicenter retrospective study on survival rate and complications of very preterm infants. Zhongguo Dang Dai Er Ke Za Zhi. 2021;23(8):814-20. Doi: 10.7499/j.issn.1008-8830.2102037 [ Links ]
6. Wikström T, Hagberg H, Jacobsson B, Kuusela P, Wesström J, Lindgren P, et al. Effect of second-trimester sonographic cervical length on the risk of spontaneous preterm delivery in different risk groups: A prospective observational multicenter study. Acta Obstet Gynecol Scand. 2021;100(9):1644-55. Doi: 10.1111/aogs.14203 [ Links ]
7. Costantine MM, Ugwu L, Grobman WA, Mercer BM, Tita ATN, Rouse DJ, et al. Cervical length distribution and other sonographic ancillary findings of singleton nulliparous patients at midgestation. Am J Obstet Gynecol. 2021;225(2):181.e1-181.e11. doi: 10.1016/j.ajog.2021.02.017 [ Links ]
8. Berghella V, Palacio M, Ness A, Alfirevic Z, Nicolaides KH, Saccone G. Cervical length screening for prevention of preterm birth in singleton pregnancy with threatened preterm labor: systematic review and meta-analysis of randomized controlled trials using individual patient-level data. Ultrasound Obstet Gynecol. 2017;49(3):322-9. Doi: 10.1002/uog.17388 [ Links ]
9. Suhag A, Berghella V. Short cervical length dilemma. Obstet Gynecol Clin North Am. 2015;42(2):241-54. Doi: 10.1016/j.ogc.2015.01.003 [ Links ]
10. Biggio JR Jr. Current approaches to risk assessment and prevention of preterm birth-a continuing public health crisis. Ochsner J. 2020;20(4):426-33. Doi: 10.31486/toj.20.0005 [ Links ]
11. Jo YS, Jang DG, Kim N, Kim SJ, Lee G. Comparison of cervical parameters by three-dimensional ultrasound according to parity and previous delivery mode. Int J Med Sci. 2011;8(8):673-8. Doi: 10.7150/ijms.8.673 [ Links ]
12. Wong CH, Chen CP, Sun FJ, Chen CY. Comparison of placental three-dimensional power Doppler low he and low he in the first and the second trimesters of pregnancy complicated by gestational diabetes mellitus. J Matern Fetal Neonatal Med. 2019;32(22):3784-91. Doi: 10.1080/14767058.2018.1472226 [ Links ]
13. Chen SJ, Chen CP, Sun FJ, Chen CY. Comparison of placental three-dimensional power low he vascular low he and placental low he in pregnancies with small for gestational age neonates. J Clin Med. 2019;8(10):1651. Doi: 10.3390/jcm8101651 [ Links ]
14. Sun W, Yin S, Wei Q, Zhang Y, Yang Z, Cai A, et al. Three-dimensional power Doppler ultrasound evaluation of placental blood low in normal monochorionic diamniotic twin pregnancies. BMC Pregnancy Childbirth. 2018;18(1):443. Doi: 10.1186/s12884-018-2080-y [ Links ]
15. De Diego R, Sabrià J, Vela A, Rodríguez D, Gómez MD. Role of 3-dimensional power Doppler sonography in differentiating pregnant women with threatened preterm labor from those with an asymptomatic short cervix. J Ultrasound Med. 2014 Apr;33(4):673-9. Doi: 10.7863/ultra.33.4.673 [ Links ]
16. Rovas L, Sladkevicius P, Strobel E, Valentin L. Reference data representative of normal findings at three-dimensional power Doppler ultrasound examination of the cervix from 17 to 41 gestational weeks. Ultrasound Obstet Gynecol. 2006;28(6):761-7. Doi: 10.1002/uog.2857 [ Links ]
17. Zeng S, Wu S, Chen C, Zhu X, Liu Y, Zeng Q, et al. Performance characteristics of 3-D power low he ultrasound (3-D-PD) with the Virtual Organ Computer-Aided Analysis (VOCAL) technique in the detection of prostate cancer. Ultrasound Med Biol. 2022;48(1):91-7. Doi: 10.1016/j.ultrasmedbio.2021.09.016 [ Links ]
18. Gudicha DW, Romero R, Kabiri D, Hernandez-Andrade E, Pacora P, Erez O, et al. Personalized assessment of cervical length improves prediction of spontaneous preterm birth: a standard and a percentile calculator. Am J Obstet Gynecol. 2021;224(3):288.e1-288.e17. doi: 10.1016/j.ajog.2020.09.002 [ Links ]
19. Bortoletto TG, Silva TV, Borovac-Pinheiro A, Pereira CM, Silva AD, França MS, et al. Cervical length varies considering different populations and gestational outcomes: Results from a systematic review and meta-analysis. PloS One. 2021;16(2):e0245746. Doi: 10.1371/journal.pone.0245746 [ Links ]
20. Rovas L, Sladkevicius P, Strobel E, Valentin L. Intraobserver and interobserver reproducibility of three-dimensional gray-scale and power Doppler ultrasound examinations of the cervix in pregnant women. Ultrasound Obstet Gynecol. 2005;26(2):132-7. Doi: 10.1002/uog.1884 [ Links ]
21. Johnson M, Mowa CN. Transcriptomic profile of VEGF-regulated genes in human cervical epithelia. Cell Tissue Res. 2021;384(3):771-788. Doi: 10.1007/s00441-020-03354-y [ Links ]
22. Yilmaz NC, Yigiter AB, Kavak ZN, Durukan B, Gokaslan H. Longitudinal examination of cervical low he and vascularization changes during the antepartum and postpartum period using three-dimensional and power Doppler ultrasound. J Perinat Med. 2010;38(5):461-5. Doi: 10.1515/jpm.2010.087 [ Links ]
23. Zhang L, Liu X, Li J, Wang X, Huang S, Luo X, et al. Maternal low -placental low he s discordance in monochorionic-diamniotic twin pregnancies with selective growth restriction assessed by three-dimensional power low he ultrasound. Med Sci Monit. 2020;26:e919247. Doi: 10.12659/MSM.919247 [ Links ]
24. Pairleitner H, Steiner H, Hasenoehrl G, Staudach A. Three-dimensional power Doppler sonography: imaging and quantifying blood low and vascularization. Ultrasound Obstet Gynecol. 1999;14(2):139-43. Doi: 10.1046/j.1469-0705.1999.14020139.x [ Links ]
25. Nooshin E, Mahdiss M, Maryam R, Amineh SN, Somayyeh NT. Prediction of preterm delivery by ultrasound measurement of cervical length and funneling changes of the cervix in pregnant women with preterm labor at 28-34 weeks of gestation. J Med Life. 2020;13(4):536-42. Doi: 10.25122/jml-2020-0069 [ Links ]
26. Wagner P, Schlechtendahl J, Hoopmann M, Prodan N, Abele H, Kagan KO. Measurement of the uterocervical angle for the prediction of preterm birth in symptomatic women. Arch Gynecol Obstet. 2021;304(3):663-9. Doi: 10.1007/s00404-021-06002-0 [ Links ]
27. Moser G, Drewlo S, Huppertz B, Armant DR. Trophoblast retrieval and isolation from the cervix: origins of cervical trophoblasts and their potential value for risk assessment of ongoing pregnancies. Hum Reprod Update. 2018;24(4):484-96. Doi: 10.1093/humupd/dmy008 [ Links ]
28. Oladosu FA, Tu FF, Garfield LB, Garrison EF, Steiner ND, Roth GE, et al. Low serum oxytocin concentrations are associated with painful menstruation. Reprod Sci. 2020;27(2):668-74. Doi: 10.1007/s43032-019-00071-y [ Links ]
29. Lear CA, Wassink G, Westgate JA, Nijhuis JG, Ugwumadu A, Galinsky R, et al. The peripheral chemoreflex: indefatigable guardian of fetal physiological adaptation to low . J Physiol. 2018;596(23):5611-23. Doi: 10.1113/JP274937 [ Links ]
30. Caposiena Caro RD, Solivetti FM, Bianchi L. Power Doppler ultrasound assessment of vascularization in hidradenitis suppurativa lesions. J Eur Acad Dermatol Venereol. 2018;32(8):1360-7. Doi: 10.1111/jdv.14745 [ Links ]
31. Athulathmudali SR, Patabendige M, Chandrasinghe SK, De Silva PHP. Transvaginal two-dimensional ultrasound measurement of cervical low he to predict the outcome of the induction of low : a prospective observational study. BMC Pregnancy Childbirth. 2021;21(1):433. Doi: 10.1186/s12884-021-03929-9 [ Links ]
Statement of ethical issues
Ethical responsibilities: Protection of persons. The authors declare that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality: The authors declare that they have followed the protocols of the Central Hospital "Dr. Urquinaona" and the University of Zulia on the publication of patient data.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Funding: The authors certify that they have not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the study.
Received: December 09, 2021; Accepted: March 19, 2022











 texto en
texto en