Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.3 Lima jul./sep. 2022 Epub 22-Sep-2022
http://dx.doi.org/10.31403/rpgo.v68i2431
Original paper
Usefulness of intraoperative sentinel node palpation in breast cancer: a cross-sectional study
1. Physician Mastologist Universidad CES, Msc Epidemiology and Public Health VIU, Cancer Research Group IDC, Medellin, Colombia.
Objective:
To determine the usefulness of intraoperative palpation and macroscopic characteristics of the sentinel lymph node in breast cancer in predicting its involvement on microscopic examination.
Methods:
Descriptive cross-sectional study with secondary analysis of a surgeon's personal registry between May 1, 2018, and October 31, 2020, at a referral center in Medellin, Colombia. Women with breast cancer without clinical axillary involvement taken to surgery for sentinel node biopsy were included. Demographic, clinical and paraclinical data were collected and analyzed using descriptive statistics.
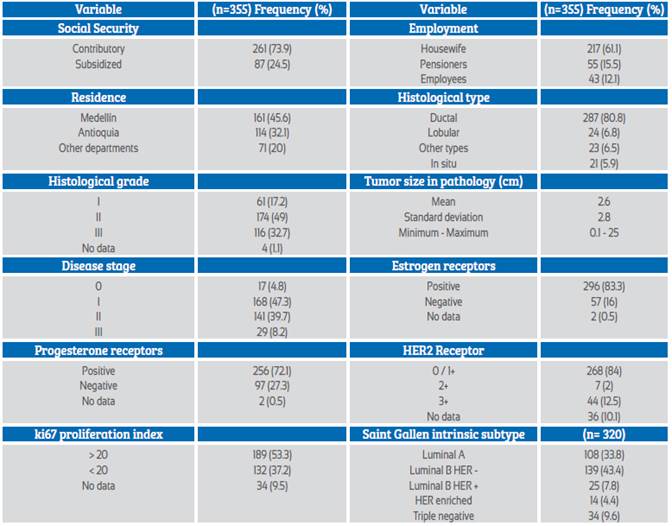
Results:
Of 355 patients who underwent sentinel node biopsy for breast cancer, the sentinel node detection rate was 98.3 % (n= 347). A higher probability of being affected was found in patients who underwent mastectomy (ORa= 4.61; 95% CI: 1.07-19.81), when the consistency of the node was hard or semi-hard (ORa= 3.90; 95% CI: 2.00-7.62) and when the shape of the node was lobulated or irregular (ORa= 12.98; 95% CI: 2.10-80.19). In contrast, it was less likely to be affected when it had received neoadjuvant chemotherapy (ORa= 0.11; 95% CI: 0.02-0.57).
Conclusion:
The evaluation of macroscopic features during sentinel node technique for axillary staging can predict its involvement on microscopic examination.
Key words: Breast neoplasms; Sentinel lymph node
Introduction
According to Globocan, in 2020 there were 2,261,419 new cases of breast cancer worldwide1. In Colombia, for the same year, the incidence was 15,509 cases, occupying the first place for cancer in women with 25.7 %2. This makes breast cancer a matter of public health interest, due to the increase in incidence and associated mortality3.
The axillary nodes receive the lymphatic drainage of the breast and are affected by metastatic tumor deposits from the primary tumor, this being one of the most important prognostic factors. The traditional treatment has been axillary lymphadenectomy of levels 1 and 2, being considered the most accurate method for evaluation and control of regional tumor dissemination4.
Giuliano et al.5, in 1990, described sentinel node biopsy, based on the fact that tumor cells migrate in an orderly manner through the lymphatic tracts. Therefore, the sentinel node is the first to be affected by metastasis, being able to predict the involvement of other nodes in the lymphatic chain and being a less invasive method with less associated morbidity.
Clinically palpable axillary lymph nodes are considered a sign of regional metastasis and represent a contraindication for performing sentinel node biopsy6. Clinical examination of the axilla by palpation is inaccurate, even when performed by an experienced surgeon. In the studies of Lang et al.7 and Voogd et al.8, when the axilla was considered to be unaffected, it was affected in 44 % and 34 % of cases, respectively. Intraoperative palpation of the axilla and sentinel node or other suspicious nodes can predict possible involvement and reduce the false negative rate9.
The aim of the present study was to describe the intraoperative morphological characteristics of the sentinel lymph node during its biopsy for breast cancer, the sociodemographic characteristics of the patients and to determine the correlation with the microscopic study, in a reference center in Medellin, Colombia.
METHODS
A descriptive cross-sectional study was developed in women with breast cancer taken to surgery with sentinel node biopsy attended in a referral center in Medellín, Colombia, between May 1, 2018 and October 31, 2020, through secondary sources of information settled in the personal record of a surgeon.
Patients with histological diagnosis of infiltrating breast carcinoma without axillary clinical involvement by physical examination and ultrasound and taken to surgery for sentinel node biopsy were identified. Patients with incomplete clinical history or with data loss greater than 10 % were excluded and, in the case that the axilla was clinically affected and confirmed with biopsy and in the metastatic stage, consecutive sequential sampling was performed. We obtained 355 records that met the inclusion criteria.
During all sentinel lymph node biopsy procedures, the surgeon evaluated the macroscopic characteristics of the sentinel lymph node intraoperatively and ex vivo. The variables of clinical interest were defined and dichotomized as follows: 1) Size: smaller than 2 cm (normal) vs larger than 2 cm (abnormal); 2) Consistency: soft (normal) vs hard or semi-hard (abnormal); 3) Shape: reniform or oval (normal) vs lobulated or irregular (abnormal); 4) Capsule: smooth (normal) vs irregular (abnormal); 5) Adhesion: non-adherent (normal) vs adherent (abnormal); 6) Perinodal fat: no inflammatory changes (normal) vs with inflammatory changes (abnormal).
The following variables were measured: age, insurance, occupation, residence, histologic type and grade, tumor, node and metastasis (TNM) staging, estrogen and progesterone receptors, human epidermal growth factor receptor 2 (HER2), ki67 antigen, type of breast surgery, sentinel node technique, number of resected and affected sentinel nodes, laterality, axillary level, axillary emptying, size, shape, consistency, adherence and perinodal involvement of the sentinel node.
After standardization of the research protocol, the information was collected, tabulated and verified by the researcher in a database in Excel® format. Descriptive analysis of the sociodemographic and clinical variables was performed. Absolute frequencies and percentages, mean and standard deviation were calculated, according to the nature and distribution of the variables. Normal distribution was validated using the Shapiro Wilk goodness-of-fit test. Bivariate analysis was performed with the chi2 test to establish the association between sentinel node involvement and the independent variables of clinical interest. For hypothesis testing, a confidence interval of 95% and a significance level of 5% was established.
The association between the presence or absence of lymph node involvement and suspicious macroscopic morphologic findings was estimated by means of the crude odds ratio (OR), assessing the magnitude of the association with its respective confidence interval. The latter was evaluated by means of an explanatory multivariate logistic regression model with the enter method, constructed with the variables that were significant in the bivariate analysis, and those that met the Hosmer Lemeshow criterion (p < 0.25) in the univariate analysis. SPSS statistics software version 23 was used.
Regarding ethical aspects, the present study is considered a risk-free study, according to the classification set forth in Article 11 of Resolution No. 008430 of 1993 (issued by the Colombian Ministry of Health), and complies with international standards, the Declaration of Helsinki and the ethical guidelines for biomedical research prepared by the Council for International Organizations of Medical Sciences -CIOMS.
Results
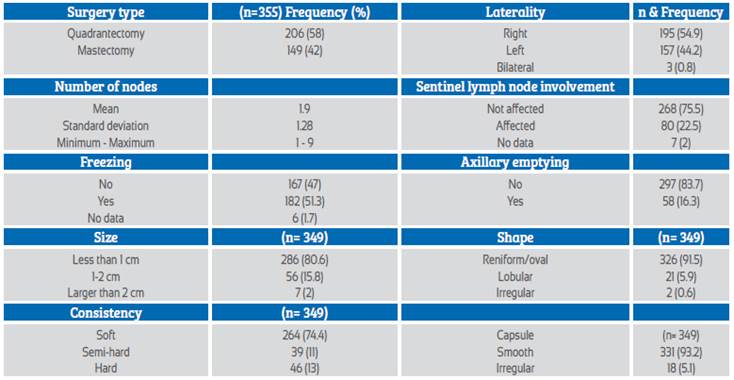
During the 30-month period, 554 axillary surgeries, 355 sentinel node biopsies (66 %) and 199 lymphadenectomies (34 %) were performed in the referral center. The mean age of the patients was 60.2 years (SD 12.6), the most frequent histological type was ductal (80.7 %, n=285), and according to TNM classification 47.3 % (n=168) corresponded to stage I, being the most frequent. Table 1 shows the sociodemographic characteristics, histology, classification, TNM stage and immunohistochemistry.
Table 1 Sociodemographic characteristics, histology, classification, TNM stage and immunohistochemistry.
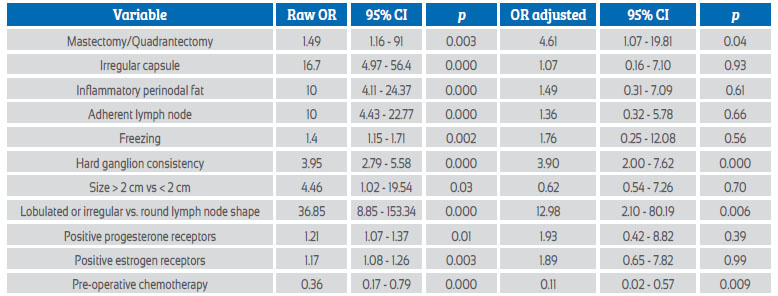
The most frequent type of surgery was quadrantectomy in 58 % (n=206); radio-guided sentinel node technique was performed in 97.9 % (n=337) of the cases, with a detection rate of 98 % (n= 348). Intraoperative evaluation of the axilla consisting of palpation of all sentinel nodes showed that the most frequent size found was less than 1 cm (80.6 %, n= 289); only 2 % (n= 7) were larger than 2 cm. Lobular and irregular shape were found in 5.9 % and 0.6 %, respectively, while consistency as a marker of lymph node involvement in the hard and semi-hard category was present in 24 % (Table 2).
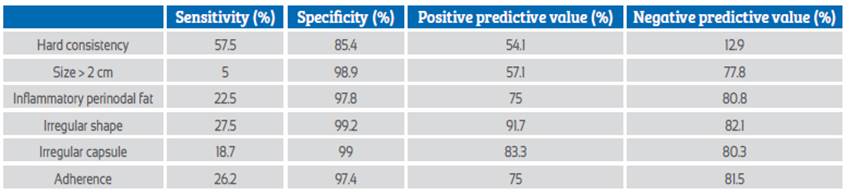
The cut-off values for sensitivity, specificity and predictive values for each morphological feature of the sentinel lymph node are shown in Table 3.
Table 3 Sensitivity, specificity, predictive values of intraoperative sentinel lymph node characteristics.
In the bivariate analysis significant statistical differences were found for the macroscopic characteristics evaluated, together with other variables of clinical interest, which were introduced in the multivariate analysis, finding that there is a greater probability that the sentinel lymph node was affected in patients who underwent mastectomy (aOR= 1.07-19.81), when the consistency of the node was hard or semi-hard (aOR= 3.90; 95% CI: 2.00-7.62) and when the shape of the node was lobulated or irregular (aOR= 12.98; 95% CI: 2.10-80.19). In contrast, it was less likely to be affected when the patient had received neoadjuvant chemotherapy (aOR= 0.11; 95% CI: 0.02 to 0.57) (Table 4).
Discussion
Radioisotope sentinel node biopsy is a widely accepted and reliable surgical method for nodal staging of breast cancer, included in the American Society of Clinical Oncology clinical practice guideline published in 20176. Intraoperative sentinel node evaluation can identify and select patients requiring lymphadenectomy and avoid a second surgical procedure.
In the study by Carmon et al.10, which included 290 patients, 30.7 % (n= 89) had sentinel node involvement; the mean number of sentinel nodes removed was 2.6, similar to the present study where 23.1 % (n = 80) had sentinel nodes involved, and an average of 1.9 nodes were removed.
In the study by Krag et al.11, using a 99mTc-labeled sulfur colloid, the intraoperative identification of the sentinel lymph node was 82%; in the present study a detection rate of 98% was found. Despite the obvious advantages of this technique, the possibility of false negative results is the main limitation, which may be caused by lymphatic blockage of the sentinel node and uptake in neighboring nodes; it is advisable to try to improve the detection rate12.
Infiltrated sentinel nodes generally increase in size and firmness. In this way they can be detected by intraoperative palpation, even when there is no uptake by the radiopharmaceutical13. For this reason, removal of suspicious palpable lymph nodes (increased in size and consistency) has been recommended, with no demonstrated increased consumption of time or resources10,14.
In the study by Serrano et al.13, intraoperative palpation identified when axillary nodes were affected in 10% (n= 5/50), reducing the occurrence of false negatives. On the other hand, the study by Pluta et al.14 in a group of 34 patients identified 6% of affected lymph nodes that were not detected in the lymphoscintigraphy. And Martin et al.15, with the same strategy managed to reduce the false negative rate from 12% to 4%.
In intraoperative palpation of the axilla, Carmon et al.10 found that 7 cases were suspected of being affected, and in the microscopic study this was confirmed in 5 cases, which made it possible to identify 71% of the affected lymph nodes. In the present study, intraoperative palpation made it possible to identify 57.5%, with a specificity of 85.4%, and false negatives were 12.9% when the lymph node was hard.
In the study of Serrano et al.13, out of a total of 168 patients 19 % (n= 32) had suspicious nodes (hard and enlarged); out of a total of 50 nodes evaluated, 5 nodes (10 %) were affected by tumor. In the present study, out of a total of 355 patients studied 85 (23.9 %) had hard sentinel lymph nodes, of which 46 (57.5 %) were affected by metastases.
It is noteworthy that in the present study 57.3 % had suspicious adenopathies (hard lymph nodes) and microscopic confirmation of carcinoma involvement, and that on physical examination of the axilla all were classified as N0, which implies that axillary palpation is imprecise and presents difficulties in the evaluation of the deep axillary planes. On the other hand, 45.9 % of the cases had suspicious intraoperative features, but were not affected after microscopic study. This high percentage is possibly associated with reactive or inflammatory changes post biopsy. It is important to perform an ultrasound evaluation to objectify these adenopathies and thus differentiate those suspicious lymph nodes that require a biopsy to confirm the presence of neoplastic infiltration16.
As strengths of the study, it is the first in the Latin American literature that explores the usefulness of intraoperative palpation and analyzes different morphological findings in sentinel lymph node biopsy in breast cancer. As limitations, it is found that the evaluation of the nodes by palpation requires experience, which makes its reproducibility difficult.
In conclusion, the evaluation of macroscopic characteristics during the sentinel lymph node technique for axillary staging can predict its involvement in the microscopic examination.
REFERENCES
1. Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, Znaor A, Bray F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019 Apr 15;144(8):1941-53. doi: 10.1002/ijc.31937 [ Links ]
2. World Health Organization (WHO). International Agency for Research on Cancer. Cancer fact sheets. Colombia, Globocan 2020. Ginebra, Suiza: World Health Organization; 2020. Acceso 6 de enero de 2021. Disponible en https://gco.iarc.fr/today/data/factsheets/ populations/170-colombia-fact-sheets.pdf [ Links ]
3. World Health Organization (WHO). Cáncer de mama: prevención y control. Ginebra, Suiza: World Health Organization. Acceso 26 de enero de 2021. Disponible en https://www.who.int/ topics/cancer/breastcancer/es/ [ Links ]
4. Tyagi NK, Dhesy-Thind S. Clinical practice guidelines in breast cancer. Curr Oncol. 2018 Jun;25(Suppl 1):S151-S160. doi: 10.3747/co.25.3729 [ Links ]
5. Giuliano AE, Kirgan DM, Guenther JM, Morton DL. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 1994 Sep;220(3):391-8; discussion 398-401. doi: 10.1097/00000658-199409000-00015 [ Links ]
6. Lyman GH, Somerfield MR, Bosserman LD, Perkins CL, Weaver DL, Giuliano AE. Sentinel Lymph Node Biopsy for Patients With Early-Stage Breast Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol. 2017 Feb 10;35(5):561-4. doi: 10.1200/JCO.2016.71.0947 [ Links ]
7. Lanng C, Hoffmann J, Galatius H, Engel U. Assessment of clinical palpation of the axilla as a criterion for performing the sentinel node procedure in breast cancer. Eur J Surg Oncol. 2007 Apr;33(3):281-4. doi: 10.1016/j.ejso.2006.09.032 [ Links ]
8. Voogd AC, Coebergh JW, Repelaer van Driel OJ, Roumen RM, van Beek MW, Vreugdenhil A, Crommelin MA. The risk of nodal metastases in breast cancer patients with clinically negative lymph nodes: a population-based analysis. Breast Cancer Res Treat. 2000 Jul;62(1):63-9. doi: 10.1023/a:1006447825160 [ Links ]
9. Choi YJ, Kim JH, Nam SJ, Ko YH, Yang JH. Intraoperative identification of suspicious palpable lymph nodes as an integral part of sentinel node biopsy in patients with breast cancer. Surg Today. 2008;38(5):390-4. doi: 10.1007/s00595-007-3653-y [ Links ]
10. Carmon M, Olsha O, Rivkin L, Spira RM, Golomb E. Intraoperative palpation for clinically suspicious axillary sentinel lymph nodes reduces the false-negative rate of sentinel lymph node biopsy in breast cancer. Breast J. 2006 May-Jun;12(3):199-201. doi: 10.1111/j.1075-122X.2006.00241.x [ Links ]
11. Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Costantino JP, Ashikaga T, Weaver DL, Mamounas EP, Jalovec LM, Frazier TG, Noyes RD, Robidoux A, Scarth HM, Wolmark N. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010 Oct;11(10):927-33. doi: 10.1016/S1470-2045(10)70207-2 [ Links ]
12. Feng J, Bernacki EG. Intraoperative cytologic evaluation of sentinel lymph nodes in patients with breast carcinoma by scrape preparation. Diagn Cytopathol. 2008 Nov;36(11):790-3. doi: 10.1002/dc.20895 [ Links ]
13. Serrano Vicente J, Infante de la Torre JR, Domínguez Grande ML, García Bernardo L, Durán Barquero C, Rayo Madrid JI, et al. Optimización de la biopsia selectiva de ganglio centinela en el cáncer de mama mediante palpación axilar intraoperatoria. Rev Esp Med Nucl. enero de 2010;29(1):8-11. Spanish. doi: 10.1016/j.remn.2009.09.003 [ Links ]
14. Pluta P, Nejc D, Piekarski J, Pasz-Walczak G, Jakubik J, Berner A, et al. Intraoperative palpation of the axilla as a part of sentinel node biopsy in breast cancer patients. Nowotwory. 2008;58:92e-4e [ Links ]
15. Martin RC, Derossis AM, Fey J, Yeung H, Yeh S, Akhurst T, et al. Intradermal isotope injection is superior to intramammary in sentinel node biopsy for breast cancer. Surgery. 2001;130:432-8. doi: 10.1067/msy.2001.116412. PMID: 11562666 [ Links ]
16. Vidal-Sicart S, Rioja Martín ME. Detección gammagra´fica e intraoperatoria del ganglio centinela en el cáncer de mama. Rev Esp Med Nucl. 2009;28:41-3. Spanish. doi: 10.1016/s0212-6982(09)70220-4. PMID: 19232181 [ Links ]
Received: May 24, 2022; Accepted: August 08, 2022











 texto en
texto en