Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.3 Lima jul./sep. 2022 Epub 22-Sep-2022
http://dx.doi.org/10.31403/rpgo.v68i2434
Case report
Management of monochorionic monoamniotic twin pregnancy: literature review and case report
1. Staff Physician, Maternal Fetal Medicine Unit, Clínica Delgado AUNA, Lima, Peru
2. Staff Physician, Instituto Peruano de Medicina y Cirugía Fetal, Lima, Peru
In view of the presentation of a case of monochorionic monoamniotic twin pregnancy, the literature on its diagnosis and management was reviewed by electronic search in the Medline, OVID, Cochrane, and PubMed databases between 1966 and 2019. The key words used in the inquiry were: pregnancy, twins, monoamniotic, cord entanglement. There is a high risk of sudden fetal death in monoamniotic twins caused by entanglement of the umbilical cords, so timely diagnosis of chorionicity and amnionicity in twin pregnancy by ultrasonography may provide guidance for close fetal surveillance and thus improve obstetric outcome.
Key words: Chorion; Amnion; Pregnancy; Twins; monozygotic; Umbilical cord; Fetal death
Introduction
The prevalence of dizygotic twins varies between populations, whereas the prevalence of monozygotic twins is relatively stable worldwide.
Monoamniotic twins account for approximately 0.01 % of spontaneously conceived pregnancies and 5 % of monochorionic twin pregnancies. Monoamniotic twins include conjoined or Siamese twins, with an incidence of 1 in 50.000 pregnancies1.
Monoamniotic twin pregnancies are the least common type and have many of the same complications as biamniotic monochorionic twin pregnancies (e.g., feto-fetal transfusion syndrome). However, monoamniotic twin pregnancy is characterized by increased risks of congenital anomalies2,3 and umbilical cord intertwining with potential sudden fetal death4.
In twin pregnancy, the post-fertilization division of the zygote determines the type of chorionicity and amnionicity. Monoamniotic monochorionic placentation occurs when that division occurs between days 8 to 12 post-fertilization. In comparison, biamniotic twins are the result of division between day 4 and 7 for monochorionic placentation and between day 1 and 3 for dichorionic placentation.
The factors responsible for the timing of embryo splitting are unknown. The use of assisted reproductive techniques appears to play a role, as in vitro fertilization increases the frequency of monozygotic twinning.
In some studies, manipulation of the zona pellucida, which is performed with intracytoplasmic sperm injection and assisted hatching, increased the frequency of monoamniotic twins5.
Ultrasonography is an effective prenatal diagnostic tool to determine amnionicity and chorionicity. This is of utmost importance, because monochorionic twins have a shared fetoplacental circulation, which puts them at risk for serious pregnancy-specific complications, such as feto-fetal transfusion syndrome (FFTS), twin anemia-polycythemia sequence (TAPS), and selective fetal growth restriction (selective IUGR)6.
These complications increase the risk of neurological morbidity and perinatal mortality in monochorionic twins compared to dichorionic twins. Also, prenatal identification of monochorionic monoamniotic twins (MCMA) is critical, because monoamnionicity carries a higher risk of adverse perinatal outcomes compared to biamnionicity7.
In expert hands, the optimal time to determine chorionicity and amnionicity is in the first trimester after seven weeks, with a sensitivity ≥ 98 %, while in the early second trimester the sensitivity is 90 %8-10.
The identification of two separate placentas is a very reliable indicator of dichorionic twins. This indicator is generally only useful in early pregnancy, as separated placentas often appear fused later in gestation.
The intergemellar membrane is absent in a monoamniotic monochorionic twin pregnancy, so great care must be taken to confuse this condition with a biamniotic monochorionic twin pregnancy complicated with severe FFTS, where the intergemellar membrane is completely folded over the donor fetus, making it almost impossible to visualize ultrasonographically.
The observation of a triangular projection of tissue extending between the layers of the intergemellar membrane from the placenta (lambda sign) determines the diagnosis of diamniotic bicornuate twin pregnancy11.
On the other hand, diamniotic monochorionic twin pregnancy is appreciated sonographically with the T-sign, which refers to the appearance of the thin intergemellar membrane composed of two amniotic layers when it detaches from the placenta at a 90-degree angle12.
There are additional findings, such as the visualization of a single vitelline vesicle with two fetal poles, strongly suggesting the presence of monoamniotic twins13,14. However, the diagnosis should always be corroborated by 12-week ultrasonography15,16.
Finally, ultrasonographic detection of umbilical cord entanglement is pathognomonic for monoamniotic twins and can be seen as early as the late first trimester17,18.
Regarding complications, monochorionic monoamniotic twin pregnancy, like diamniotic monochorionic twin pregnancy, may present with FFTS, selective IUGR, preterm delivery and, particularly, the unique complication of monoamniotic pregnancies, such as umbilical cord entanglement.
The high mortality rate of monoamniotic twins has been related to sudden death because of such umbilical crosslinking. Intermittent occlusion of the umbilical blood vessels may be associated with neurological morbidity, whereas prolonged occlusion may be lethal19.
Monoamniotic twins have a high mortality rate, which has been reported in up to 50% of cases. Monoamniotic twins have a high risk of congenital malformations, reaching a frequency of 38-50 %, usually affecting only one twin20,21.
Monoamniotic twin pregnancy should be managed in a specialized center, as it requires close surveillance.
Given the high frequency of congenital malformations in this group of twins, it is essential to perform a specialized ultrasound between 12 and 14 weeks of gestation and a detailed morphological ultrasound between 16 and 18 weeks22.
The antenatal management plan should include monitoring of fetal well-being, so ultrasound surveillance is recommended every 2 weeks after week 2423.
Umbilical artery Doppler evaluation should be performed at least weekly. Abnormal Doppler ultrasound findings vary in severity from the presence of a diastolic notch to absent or reverse diastole24. The presence of such a notch may reflect hemodynamic alterations in the fetal-placental circulation secondary to narrowing of the umbilical vessels involved in umbilical entanglement25.
Regarding in-hospital versus home or outpatient surveillance, the MONOMONO study evaluated the difference in obstetric outcome between the two types of surveillance. 195 pregnant women with an uncomplicated monoamniotic twin gestation (390 fetuses) were included. Of these, 75 (38.5 %) were managed as inpatients and 120 (61.5 %) as outpatients. The overall perinatal loss rate was 10.8 % (42/390), with a peak fetal mortality rate of 4.3 % (15/348) occurring at 29 weeks' gestation. On that basis, there was no statistically significant difference in fetal mortality rates between inpatient management initiated at 26 weeks compared with outpatient surveillance26.
Elective cesarean termination of monoamniotic gestations at 32-33 weeks is recommended to avoid potential sudden death due to cord entanglement and extreme prematurity27. Neonatal outcomes are reasonably good at 32 weeks for infants cared for in well-equipped neonatal intensive care units28. If the fetus has not had pulmonary maturation before 28 weeks because of threatened preterm delivery, administration of a new course of antenatal corticosteroids is recommended at the time of hospital admission.
Case report
We present the case of a 37-year-old female patient with type 2 diabetes mellitus in glycemic control with diet and hypothyroidism under treatment with levothyroxine, managed in a maternal-fetal medicine unit of a private hospital.
Her first trimester ultrasound determined a monochorionic monoamniotic twin gestation and her noninvasive prenatal genetic testing was reported as normal, with both female fetuses.
On second trimester morphologic ultrasound, the anatomy of both fetuses was normal, as was their growth. Also, sonographic signs of umbilical cord entanglement were already identified.
At 28 weeks, during ultrasound surveillance, the diagnosis of intrauterine growth restriction was established in both fetuses (Figure 1) and umbilical cord entanglement was evident (Figures 2 and 3). The Doppler spectral representation of the umbilical artery showed a protodiastolic notch (Figure 4), so the diagnosis of 28-week monochorionic monoamniotic twin pregnancy complicated with IUGR in both fetuses, umbilical cord entanglement, history of previous cesarean section, hypothyroidism and pregestational diabetes was established.
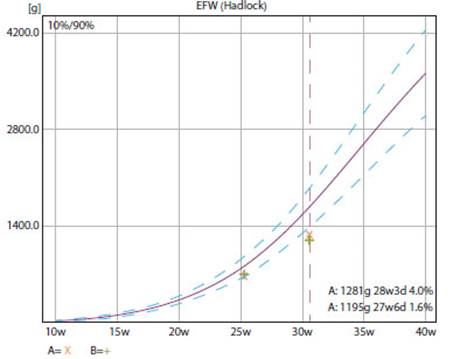
Figure 1 Graph of the growth pattern of both fetuses. A downward growth curve is shown with fetus A at percentile 4 and fetus B at percentile 2.
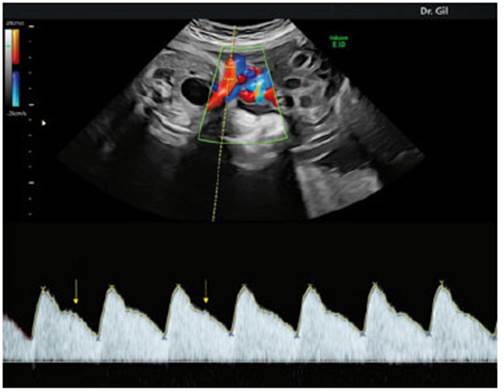
Figure 4 Doppler study of the umbilical artery showing protodiastolic notch (yellow arrow) due to umbilical compression by cord entanglement.
In-hospital management for antenatal surveillance was decided. During hospitalization at the maternity center, strict electronic fetal monitoring was performed 3 times a day and Doppler ultrasound, evaluating blood flow in the umbilical artery, middle cerebral artery, and venous ductus twice a week.
It was decided to terminate the pregnancy at 32 weeks and 4 days after administering 2 cycles of pulmonary maturity inducers and neuroprotection with magnesium sulfate the night before surgery.
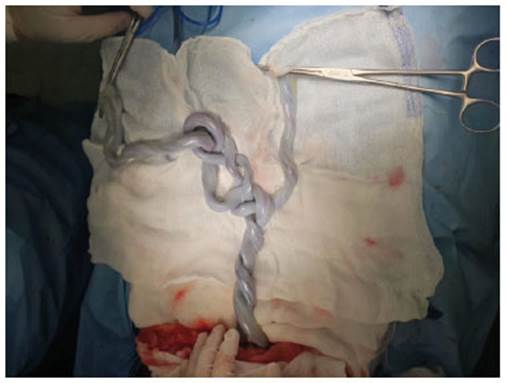
The cesarean section was performed without complications, obtaining two female newborns with immediate crying and weights of 1,750 and 1,560 grams and Apgar of both babies of 8 at one minute and 9 at 5 minutes, having as the most important finding the presence of intertwined umbilical cords and with two true knots between them (Figures 5 and 6).

Figure 6 Postnatal evaluation showing the proximity between the placental insertions of the umbilical cords.
The patient was discharged on the third post-cesarean day with favorable evolution. The twins remained hospitalized in the neonatal ICU for 27 days in an incubator without major respiratory distress. During their hospitalization they gained weight and achieved spontaneous suction, being discharged with weights of 2,100 and 2,040 grams.
Discussion
Perinatal mortality is the most important complication of monoamniotic placentation, either due to sudden fetal death secondary to umbilical cord entanglement or due to fetal growth disturbances and prematurity.
Umbilical cord entanglement is one of the main causes of fetal death in these pregnancies, which occurs due to the proximity of the placental insertions of the umbilical cords.
The key point in the management of twin pregnancies is the timely ultrasound diagnosis of chorionicity and amnionicity, since once these are determined, an antenatal surveillance plan can be implemented, thus reducing perinatal morbidity and mortality.
The present case is important because it shows how a monochorionic monoamniotic twin gestation complicated with IUGR and umbilical cord entanglement can be successfully managed in a tertiary level center, both prenatally and postnatally.
It is important to highlight the permanent fetal surveillance in complicated monoamniotic twin pregnancies and the resolution of the pregnancy by elective cesarean section at 32-33 weeks after pulmonary maturation and fetal neuroprotection.
In the present communication, in-hospital surveillance was decided due to the diagnosis of IUGR in both fetuses and the presence of notch in the spectral Doppler wave of the umbilical artery, which is an indicator of funicular compression.
Delivery in a well-equipped neonatal intensive care unit is associated with a low risk of neonatal mortality or severe morbidity.
Finally, the available evidence is insufficient to allow a strong recommendation on the optimal gestational age for planned delivery of these pregnancies, but this case clearly demonstrates that individual maternal and fetal management should be individualized for each pregnant woman.
REFERENCES
1. Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: Final Data for 2018. Natl Vital Stat Rep. 2019;68(13):1-47. PMID: 32501202 [ Links ]
2. Hack KE, Derks JB, Schaap AH, Lopriore E, Elias SG, Arabin B, Eggink AJ, Sollie KM, Mol BW, Duvekot HJ, Willekes C, Go AT, Koopman-Esseboom C, Vandenbussche FP, Visser GH. Perinatal outcome of monoamniotic twin pregnancies. Obstet Gynecol. 2009 Feb;113(2 Pt 1):353-60. doi: 10.1097/AOG.0b013e318195bd57. PMID: 19155906 [ Links ]
3. Heyborne KD, Porreco RP, Garite TJ, Phair K, Abril D; Obstetrix/Pediatrix Research Study Group. Improved perinatal survival of monoamniotic twins with intensive inpatient monitoring. Am J Obstet Gynecol. 2005 Jan;192(1):96-101. doi: 10.1016/j.ajog.2004.06.037. PMID: 15672009 [ Links ]
4. Sebire NJ, Snijders RJ, Hughes K, Sepulveda W, Nicolaides KH. The hidden mortality of monochorionic twin pregnancies. Br J Obstet Gynaecol. 1997 Oct;104(10):1203-7. doi: 10.1111/j.1471-0528.1997.tb10948.x. PMID: 9333002 [ Links ]
5. Sills ES, Tucker MJ, Palermo GD. Assisted reproductive technologies and monozygous twins: implications for future study and clinical practice. Twin Res. 2000 Dec;3(4):217-23. doi: 10.1375/136905200320565184. PMID: 11463142 [ Links ]
6. Dubé J, Dodds L, Armson BA. Does chorionicity or zygosity predict adverse perinatal outcomes in twins? Am J Obstet Gynecol. 2002 Mar;186(3):579-83. doi: 10.1067/mob.2002.121721. PMID: 11904627 [ Links ]
7. Ishii K. Prenatal diagnosis and management of monoamniotic twins. Current Opinion in Obstetrics & Gynecology. 2015 Apr;27(2):159-64. DOI: 10.1097/gco.0000000000000160. PMID: 25689237 [ Links ]
8. Emery SP, Bahtiyar MO, Dashe JS, Wilkins-Haug LE, Johnson A, Paek BW, Moon-Grady AJ, Skupski DW, O'Brien BM, Harman CR, Simpson LL. The North American Fetal Therapy Network Consensus Statement: prenatal management of uncomplicated monochorionic gestations. Obstet Gynecol. 2015 May;125(5):1236-43. doi: 10.1097/AOG.0000000000000723. PMID: 25932853 [ Links ]
9. Lee YM, Cleary-Goldman J, Thaker HM, Simpson LL. Antenatal sonographic prediction of twin chorionicity. Am J Obstet Gynecol. 2006 Sep;195(3):863-7. doi: 10.1016/j.ajog.2006.06.039 [ Links ]
10. Wan JJ, Schrimmer D, Taché V, Quinn K, Lacoursiere DY, James G, Benirschke K, Pretorius DH. Current practices in determining amnionicity and chorionicity in multiple gestations. Prenat Diagn. 2011 Jan;31(1):125-30. doi: 10.1002/pd.2663 [ Links ]
11. Maruotti GM, Saccone G, Morlando M, Martinelli P. First-trimester ultrasound determination of chorionicity in twin gestations using the lambda sign: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2016 Jul;202:66-70. doi: 10.1016/j.ejogrb.2016.04.023 [ Links ]
12. Dias T, Arcangeli T, Bhide A, Napolitano R, Mahsud-Dornan S, Thilaganathan B. First-trimester ultrasound determination of chorionicity in twin pregnancy. Ultrasound Obstet Gynecol. 2011 Nov;38(5):530-2. doi: 10.1002/uog.8956 [ Links ]
13. Levi CS, Lyons EA, Dashefsky SM, Lindsay DJ, Holt SC. Yolk sac number, size and morphologic features in monochorionic monoamniotic twin pregnancy. Can Assoc Radiol J. 1996 Apr;47(2):98-100. PMID: 8612093 [ Links ]
14. Bromley B, Benacerraf B. Using the number of yolk sacs to determine amnionicity in early first trimester monochorionic twins. J Ultrasound Med. 1995 Jun;14(6):415-9. doi: 10.7863/jum.1995.14.6.415 [ Links ]
15. Bishop DK. Yolk-sac number in monoamniotic twins. Obstet Gynecol. 2010 Aug;116 Suppl 2:504-7. doi: 10.1097/AOG.0b013e3181d99268 [ Links ]
16. Murakoshi T, Ishii K, Matsushita M, Shinno T, Naruse H, Torii Y. Monochorionic monoamniotic twin pregnancies with two yolk sacs may not be a rare finding: a report of two cases. Ultrasound Obstet Gynecol. 2010 Sep;36(3):384-6. doi: 10.1002/uog.7710 [ Links ]
17. Perlman EJ, Stetten G, Tuck-Müller CM, Farber RA, Neuman WL, Blakemore KJ, Hutchins GM. Sexual discordance in monozygotic twins. Am J Med Genet. 1990 Dec;37(4):551-7. doi: 10.1002/ajmg.1320370427 [ Links ]
18. Shahabi S, Donner C, Wallond J, Schlikker I, Avni EF, Rodesch F. Monoamniotic twin cord entanglement. A case report with color flow Doppler Ultrasonography for antenatal diagnosis. J Reprod Med. 1997 Nov;42(11):740-2. PMID: 9408875 [ Links ]
19. Rossi AC, Prefumo F. Impact of cord entanglement on perinatal outcome of monoamniotic twins: a systematic review of the literature. Ultrasound Obstet Gynecol. 2013 Feb;41(2):131-5. doi: 10.1002/uog.12345 [ Links ]
20. Van Mieghem T, Abbasi N, Shinar S, Keunen J, Seaward G, Windrim R, Ryan G. Monochorionic monoamniotic twin pregnancies. Am J Obstet Gynecol MFM. 2022 Mar;4(2S):100520. doi: 10.1016/j.ajogmf.2021.100520 [ Links ]
21. Rodis JF, McIlveen PF, Egan JF, Borgida AF, Turner GW, Campbell WA. Monoamniotic twins: improved perinatal survival with accurate prenatal diagnosis and antenatal fetal surveillance. Am J Obstet Gynecol. 1997 Nov;177(5):1046-9. doi: 10.1016/s0002-9378(97)70012-7 [ Links ]
22. Kagan KO, Gazzoni A, Sepulveda-Gonzalez G, Sotiriadis A, Nicolaides KH. Discordance in nuchal translucency thickness in the prediction of severe twin-to-twin transfusion syndrome. Ultrasound Obstet Gynecol. 2007 May;29(5):527-32. doi: 10.1002/uog.4006 [ Links ]
23. Allen VM, Windrim R, Barrett J, Ohlsson A. Management of monoamniotic twin pregnancies: a case series and systematic review of the literature. BJOG. 2001 Sep;108(9):931-6. doi: 10.1111/j.1471-0528.2001.00216.x [ Links ]
24. Su LL. Monoamniotic twins: diagnosis and management. Acta Obstet Gynecol Scand. 2002 Nov;81(11):995-1000. doi: 10.1034/j.1600-0412.2002.811101.x [ Links ]
25. Abuhamad AZ, Mari G, Copel JA, Cantwell CJ, Evans AT. Umbilical artery flow velocity waveforms in monoamniotic twins with cord entanglement. Obstet Gynecol. 1995 Oct;86(4 Pt 2):674-7. doi: 10.1016/0029-7844(95)00210-i [ Links ]
26. MONOMONO Working Group. Inpatient vs outpatient management and timing of delivery of uncomplicated monochorionic monoamniotic twin pregnancy: the MONOMONO study. Ultrasound Obstet Gynecol. 2019 Feb;53(2):175-183. doi: 10.1002/uog.19179 [ Links ]
27. Van Mieghem T, De Heus R, Lewi L, Klaritsch P, Kollmann M, Baud D, Vial Y, Shah PS, Ranzini AC, Mason L, Raio L, Lachat R, Barrett J, Khorsand V, Windrim R, Ryan G. Prenatal management of monoamniotic twin pregnancies. Obstet Gynecol. 2014 Sep;124(3):498-506. doi: 10.1097/AOG.0000000000000409 [ Links ]
28. Manuck TA, Rice MM, Bailit JL, Grobman WA, Reddy UM, Wapner RJ, Thorp JM, Caritis SN, Prasad M, Tita AT, Saade GR, Sorokin Y, Rouse DJ, Blackwell SC, Tolosa JE; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Preterm neonatal morbidity and mortality by gestational age: a contemporary cohort. Am J Obstet Gynecol. 2016 Jul;215(1):103.e1-103.e14. doi: 10.1016/j.ajog.2016.01.004 [ Links ]
Received: July 22, 2022; Accepted: August 08, 2022











 texto en
texto en