Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.3 Lima jul./sep. 2022 Epub 22-Sep-2022
http://dx.doi.org/10.31403/rpgo.v68i2438
Case report
Uterine lipoleiomyoma
1. Physician specialist in Gynecology and Obstetrics, Obstetrics and Gynecology Service, Hospital Central "Dr. Urquinaona", Maracaibo, Zulia State, Venezuela
Lipoleiomyoma is a rare benign uterine neoplasm whose incidence varies between 0.03%-0.2%. This tumor is considered a benign variant of typical uterine leiomyomas. It consists of a variable proportion of mature adipocytes and smooth muscle cells. The etiology may be related to estrogen deficiency occurring after the menopausal transition; it usually appears in obese perimenopausal or menopausal women. The symptomatology is nonspecific, and most are diagnosed incidentally. We present a case of uterine lipoleiomyoma in a 45-year-old patient who consulted for abdominal pain. Ultrasonography showed a tumor in the anterior wall of a homogeneous and well-defined uterus. During laparotomy, a yellowish tumor with a soft texture was found. Total hysterectomy plus oophorosalpingectomy was performed. The anatomopathologic diagnosis was uterine lipoleiomyoma.
Key words: Lipoleiomyoma; Uterine tumor; Adipocytes; Smooth muscle tumor
Introduction
Primary uterine lipomatous tumors are infrequent and generally benign. Histologically, these tumors include pure lipomas, lipoleiomyomas, and fibrolipomyomas1,2. Uterine lipoleiomyoma, a variant of leiomyoma, has an incidence of approximately 0.03%-0.2% of all uterine tumors3. It is composed of variable amounts of mature adipocytes and smooth muscle cells and its most common location is the uterine corpus, as intramural growths. It has also been described in the cervix, ovaries and retroperitoneum and most cases have been reported in menopausal women4. They are difficult to diagnose clinically and can be confused with mature ovarian teratoma, well-differentiated liposarcoma and atypical lipoma2,3. Symptomatology is similar to atypical leiomyomas, and they do not require treatment if they are asymptomatic1,4. A case of uterine lipoleiomyoma is presented.
Case report
A 45-year-old woman, nulligesta, consulted for presenting hypogastric pain of 15 days of evolution accompanied by increased abdominal volume and menometrorrhagia for approximately 6 months. The patient reported menarche at 15 years of age with menstrual cycles of 5 to 6 days and an interval of 26 days. She denied medical and surgical history of importance.
Physical examination revealed an enlarged uterus with a hard, mobile, and non-painful tumor that reached two centimeters below the umbilical scar, compatible with an 18-week pregnancy. There were no palpable adenopathies or visceromegaly. The gynecological examination revealed no abnormalities of the vulva, vagina, and cervix. The rest of the physical examination was within normal limits.
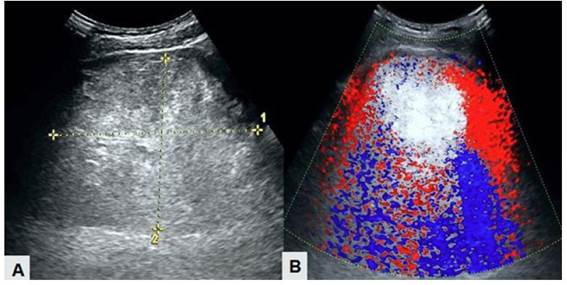
Ultrasound showed an enlarged uterus with a 10-millimeter endometrium, which contained a homogeneous, hyperechoic, well-defined tumor measuring 26 x 22 x 15 centimeters on its anterior wall, suggesting the possibility of uterine leiomyoma. Both adnexa had a normal appearance. Doppler evaluation revealed low vascularization of the lesion (Figure 1). Computed tomography images were like those on ultrasound with predominantly fatty component within the lesion. The tumor displaced the urinary bladder, rectum, and other abdominopelvic structures. Routine test results, including tumor markers, were within normal limits. In view of the findings, the patient was scheduled for surgery.
Figure 1. Ultrasound images of uterine lipoleiomyoma. A) Homogeneous hyperechogenic and well-defined tumor. B) Doppler ultrasound showing low vascular flow within the tumor.
During laparotomy, a 20 x 18 x 8 centimeter yellowish, soft-textured tumor was observed protruding into the abdominal cavity. Total hysterectomy with bilateral oophorosalpingectomy was performed. There was no evidence of lymphadenopathy, and the pelvic organs were macroscopically normal. Transoperative blood loss was minimal, and the surgery was completed without complications.
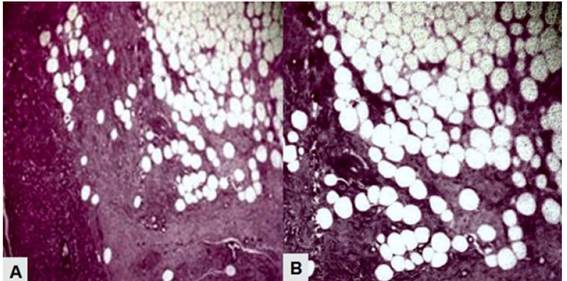
On macroscopic examination, the uterus showed a smooth, subserosal, homogeneous, grayish-white tumor with internal yellow areas on cross-section (Figure 2). Both ovaries and fallopian tubes were normal. Histological study of the specimen showed a large cellular proliferation of mature adipose predominance without cellular atypia, together with smooth muscle cells and large intercellular edema (Figure 3). The adipocytes were mature and without evidence of lipoblasts, mitosis, necrosis or angiomatosis. On immunohistochemistry, the cells were positive for smooth muscle actin but negative for HMB-45. The endometrium showed simple hyperplastic changes without atypia. The anatomopathologic diagnosis was uterine lipoleiomyoma.
Figure 2. Macroscopic image of uterine lipoleiomyoma.
Figure 3. Microscopic image of uterine lipoleiomyoma. A) Proliferation of spindle-shaped smooth muscle cells mixed with mature adipocytes (Hematoxylin-eosin stain, 10X). B) Mature adipocytes without cellular atypia mixed with smooth muscle cells (Hematoxylin-eosin stain, 40X).
The patient had an uncomplicated postoperative period and was discharged on the third day of surgery. After 12 months of follow-up there was no evidence of tumor recurrence.
Discussion
Uterine lipomatous tumors are divided into 3 groups: pure lipomas (composed of mature adipose tissue), lipoleiomyomas (composed of a mixture of smooth muscle cells and mature adipose tissue) and malignant liposarcomas5. Lipoleiomyoma of the uterus was first described as soft tissue myolipoma in 19911. Like the typical leiomyoma, it is a benign and well-defined lesion, but with a large amount of adipose tissue4-6.
The pathogenesis of lipoleiomyoma is unknown. Lipomatous metaplasia or pluripotent mesenchymal cells have been proposed as hypotheses to explain its origin. Some authors have also proposed vascular proliferation like that observed in renal angiomyolipomas as a possible cause7,8. However, fatty metaplasia is the most accepted theory, since the tumors lack lipoblasts, adipocyte atypia or smooth muscle cells and necrosis.
The clinical manifestations of lipoleiomyoma are uncertain due to its low incidence. Unlike typical leiomyomas that tend to occur predominantly in women of reproductive age and diminish at menopause, these tumors are very slow growing, largely asymptomatic, and continue to grow after menopause9. Therefore, lipoleiomyoma is most common in perimenopausal and menopausal women between 50 and 70 years of age5,6. In general, most patients are asymptomatic, and the diagnosis is made incidentally. However, some present with symptoms similar to typical leiomyomas of comparable size, such as abdomino-pelvic discomfort, heaviness, and genital bleeding2-4. In cases of acute and persistent abdominal pain, the possibility of torsion should be considered10.
Patients with uterine lipoleiomyomas usually have associated metabolic disorders, such as dyslipidemia, diabetes mellitus, or hypothyroidism. These metabolic disorders, together with estrogen deficiency occurring in the peri- or menopausal period, seem to promote abnormal intracellular storage of lipids in adipocytes within the tumor. However, the precise reason for this association is still unknown11. This hypothesis is consistent with the advanced age of most patients at the time of diagnosis3. However, the present case did not present any of the metabolic disorders mentioned.
Imaging diagnosis of lipoleiomyoma is challenging, as it can sometimes resemble both a typical leiomyoma and a mature ovarian teratoma, depending on its location8,12. The characteristic ultrasound image is of a well-defined heterogeneous lesion containing hyperechoic areas due to adipose tissue. Therefore, accurate diagnosis depends on the correct identification of the tumor components7. Magnetic resonance imaging and computed tomography allow the determination of the location of the tumor and the nature of its contents4. Although some features in the different imaging modalities may suggest the possible diagnosis of these tumors, the precise diagnosis is based on histopathological findings13.
Lipoleiomyomas present characteristic histological findings, as they are composed of adipocytes, hyperplastic smooth muscle cells and fibrous tissue. The combination of mature adipocytes and smooth muscle cells is necessary to correctly assign this condition3. Among lipoleiomyomas, the distribution of the adipose component is highly variable and ranges from uniform distribution within the tumor to focal concentrations in small areas. Therefore, there is no specific percentage of mature adipocytes to confirm the diagnosis. On the other hand, tumors with few microscopic foci of adipose tissue are similar to typical leiomyomas, while those with large amounts of adipose components have yellowish coloration and lobulated cut surface5.
The differential diagnosis of uterine lipoleiomyomas includes benign cystic teratoma, malignant degeneration of cystic teratoma, non-teratomatous ovarian lipomatous tumor, benign pelvic lipomas, liposarcomas and lipoblastic lymphadenopathies14. An association has been described between uterine lipomatous tumors with both endometrial carcinomas and lipoleiomyosarcomas arising from uterine lipoleiomyomas11.
Small, asymptomatic lipoleiomyomas are managed similarly to typical leiomyomas. Surgery is only indicated in larger lesions that produce compression to neighboring organs and/or menstrual alterations3,4. They have an excellent prognosis, since, to date, there are no reports of tumor recurrence after hysterectomy. Long-term follow-up of patients has shown that these tumors are benign, with no evidence of recurrence and are not associated with mortality, if diagnosed as a single pelvic pathology4. However, there are reports of lipoleiomyomyosarcomas arising from uterine lipoleiomyomas and cases of intravenous lipoleiomyomatosis, so patients should undergo frequent clinical and pathologic evaluations to detect any coexisting gynecologic neoplasms15.
In conclusion, uterine lipoleiomyomas are extraordinarily rare, with clinical manifestations similar to typical leiomyomas. They are usually asymptomatic, so diagnosis can be difficult. In case of diagnostic doubt in the ultrasound evaluation, computed tomography and/or magnetic resonance imaging allow differentiation of the adipose component within the tumor. The definitive diagnosis is based on anatomopathologic findings that show the presence of mature adipose tissue and smooth muscle cells in different proportions without cellular atypia. Surgery is only indicated to alleviate the associated symptoms.
REFERENCES
1. Yadav S, Maheswari B, Sagar N, Mallya V, Khurana N, Gupta S. Broad ligament lipoleiomyoma masses: Two curious cases masquerading as ovarian carcinomas. Sultan Qaboos Univ Med J. 2017;17(4):e477-e480. https://dx.doi.org/10.18295/squmj.2017.17.04.018 [ Links ]
2. Schaefer SL, Strong AL, Bahroloomi S, Han J, Whisman MK, Wilkowski JM, et al. Large intraperitoneal lipoleiomyoma in a pre-menopausal woman: a case report. World J Surg Oncol. 2021;19(1):144. https://dx.doi.org/10.1186/s12957-021-02256-9 [ Links ]
3. Alsaif JM, Alali ZS, Elsharkawy T, Ahmed A. Uterine lipoleiomyoma: a case report and review of literature. Cureus. 2021;13(12):e20297. https://dx.doi.org/10.7759/cureus.20297 [ Links ]
4. Saraf P, Thirunavukkarasu B, Kathuria P, Solanki V. Lipoleiomyoma: incidental finding in a postmenopausal woman. Int J Gynecol Cancer. 2021;31(7):1092-94. https://dx.doi.org/10.1136/ijgc-2021-002657 [ Links ]
5. Yuan Y, Chen L, Zhao T, Yu M. Pathogenesis, diagnosis and treatment of uterine lipoleiomyoma: A review. Biomed Pharmacother. 2021;142:112013. https://dx.doi.org/10.1016/j.biopha.2021.112013 [ Links ]
6. Bosoteanu M, Voda RI, Orasanu CI, Aschie M, Enciu M, Baltatescu GI. A case of giant mesenchymal uterine tumor: Lipoleiomyoma. Am J Case Rep. 2022;23:e934913. https://dx.doi.org/10.12659/AJCR.934913 [ Links ]
7. Wahal SP, Mardi K. Lipoleiomyoma of uterus and lipoma of broad ligament--a rare entity. J Cancer Res Ther. 2014;10(2):434-6. https://dx.doi.org/10.4103/0973-1482.136682 [ Links ]
8. Ando T, Kato H, Furui T, Morishige KI, Goshima S, Matsuo M. Uterine smooth muscle tumours with hyperintense area on T1 weighted images: differentiation between leiomyosarcomas and leiomyomas. Br J Radiol. 2018 Apr;91(1084):20170767. https://dx.doi.org/10.1259/bjr.20170767 [ Links ]
9. Jamoulle JF, Brisbois D. Lipoleiomyoma: rare tumor of the uterus. Rev Med Liege. 2020;75(3):137-9 [ Links ]
10. Tavernaraki E, Athanasiou S, Ampatzis P. Spontaneous uterine leiomyoma torsion: A challenging differential diagnosis for radiologists. Eur J Case Rep Intern Med. 2020 Jun 23;7(9):001586. https://dx.doi.org/10.12890/2020_001586 [ Links ]
11. Novellas S, Bafghi A, Caramella T, Chevallier A, Bongain A, Chevallier P, et al. Uterine lipoleiomyoma: atypical MR imaging features. J Radiol. 2008;89(12):1941-3. https://dx.doi.org/10.1016/s0221-0363(08)74791-7 [ Links ]
12. Chandawale SS, Karia KM, Agrawal NS, Patil AA, Shetty AB, Kaur M. Uterine lipoleiomyoma and lipoma: a rare unique case report with review of literature. Int J Appl Basic Med Res. 2018;8(3):193-195. https://dx.doi.org/10.4103/ijabmr.IJABMR_119_17 [ Links ]
13. Nazir HM, Mehta S, Seena CR, Kulasekaran N. Uterine Lipoleiomyoma: A Report of Two Cases. J Clin Imaging Sci. 2017;7:26. https://dx.doi.org/10.4103/jcis.JCIS_13_17 [ Links ]
14. Rampersad FS, Verma S, Diljohn J, Persad V, Persad P. Uterine Lipoleiomyoma Presenting With Pelvic Pain in a Post-Menopausal Woman. Cureus. 2021;13(5):e14929. https://dx.doi.org/10.7759/cureus.14929 [ Links ]
15. Oh SR, Cho YJ, Han M, Bae JW, Park JW, Rha SH. Uterine Lipoleiomyoma in Peri or Postmenopausal Women. J Menopausal Med. 2015;21(3):165-70. https://dx.doi.org/10.6118/jmm.2015.21.3.165 [ Links ]
Statement of ethical issues
Ethical responsibilities: Protection of persons. We, the authors, declare that the procedures followed conformed to the ethical standards of the committee on responsible human experimentation and in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentiality: The authors declare that we have followed the protocols of the Hospital Central "Dr. Urquinaona" on the publication of patient data.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Funding: The authors certify that we have not received financial support, equipment, personnel, or in-kind support from individuals, public and/or private institutions for the conduct of the study.
Received: April 18, 2022; Accepted: May 11, 2022











 texto en
texto en