Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.4 Lima oct./dic 2022 Epub 30-Nov-2022
http://dx.doi.org/10.31403/rpgo.v68i2448
Original paper
Biventricular performance index of the fetal heart
1. MD, PhD, DHC Universidad de Carabobo, Valencia, Venezuela.
2. Physician and Surgeon, Specialist in Obstetrics and Gynecology, Centro Policlínico Valencia, Venezuela.
5. Specialist in Obstetrics and Gynecology, Fetal Cardiologist, Cardiology Unit, Fundación Universitaria de Cardiología Porto Alegre, RS, Brazil.
7. Physician and Surgeon, Specialist in Fetal Cardiology, Fetal Cardiologist, Cardiology Unit, Fundación Universitaria de Cardiología Porto Alegre, RS, Brazil
8. MD, Associate Professor, Division Chair Maternal Fetal Medicine, Section Head Fetal Diagnosis and Therapy, Department of Obstetrics and Gynecology, Mayo Clinic School of Medicine, Rochester, Minnesota, USA.
Objectives:
To propose a biventricular performance index based on the average values of the duration of the cardiac cycle of each of the ventricles, to determine the variable included in the study with the most significant statistical correlation, to establish reference values that allow the work of each ventricle to be identified according to this variable, and to obtain a balanced biventricular output index.
Methodology:
Prospective and cross-sectional study in fetuses of 168 pregnant women, in pregnancies between 16 and 38 weeks without maternal-fetal pathologies. Flow velocity waves were obtained from both atrioventricular valves and the total systole-diastole cycle time was calculated in milliseconds for each valve. Averages, standard deviation, and Z-score were calculated of the systolic-diastolic time for each ventricle and the individual ventricular performance index (VPI) were calculated by dividing the value obtained by the fetal heart rate (FHR). The average value of both was obtained and this, when divided by the heart rate, made it possible to obtain the biventricular performance index (BPI) to establish the correlation between this, the fetal heart rate and gestational age.
Results:
Systolic-diastolic time values in milliseconds for the right ventricle were 420.8 (SD ±28.3) and for the left ventricle 418.8 (SD ±26.3), with no statistically significant differences (p<0.371). The correlation with the FHR was negative for both ventricles: (-0.491 and -0.553; p<0.05). The mean biventricular time was 418.37 ms (±20.59) and the correlation with gestational age was 0.48 (p<0.05); the correlation with FHR was negative, -0.50 (p<0.05).The BPI showed values of 2.8 (extremes 2.4 (P5) and 3.4 (P95)). The correlation between BPI and FHR was 0.78 (p<0.05) and of lesser degree with gestational age (0.27; p<0.05).
Conclusions:
It was demonstrated that the systolic-diastolic times of each ventricle did not differ from each other and were negatively correlated with fetal heart rate. It was shown that it is possible to evaluate the fetal cardiac cycle of each ventricle by means of the ventricular performance index as well as to qualify with the biventricular performance index the combined cardiac output as balanced.
Key words: Echography; fetal; Heart function tests; fetal; Ultrasonography; Echocardiography Doppler
Introduction
The fetal cardiac output is accomplished through two different circulations that are coupled in a parallel circuit, with different hemoreologic characteristics, whereas in extrauterine life and after the closure of the ductus arteriosus, foramen ovale and umbilical circulation, the so-called pulmonary and systemic networks are coupled in a series system. Studies show a broad consensus that the fetal heart, in both the human and lamb models1, exhibits right-sided dominance, with the majority (52-65%) of cardiac output being carried by the right ventricle (RV) and most of it being shunted through the ductus arteriosus into the systemic circulation. Therefore, it is reasonable to say that in the fetus the RV is a systemic ventricle responsible for perfusion of the fetal body and placenta through an infra-isthmic circulation, while the left ventricle is cerebral and systemic with predominantly supra-isthmic circulation, although both circulations converge downstream in the descending aorta.
The normal fetal heart rate varies from 110 to 160 beats per minute and works on the subject state that the placental bed provides low systemic vascular resistance and absorbs more than 40% of the combined cardiac output of both ventricles2-4. Flow through the ductus arteriosus accounts for two-thirds of the cardiac output supplying the lower half of the body and placenta. The outflow from the left ventricle is directed to the subclavian, coronary and carotid arteries, supplying the upper extremities, cardiac muscle and brain. The amount of blood entering the pulmonary circulation varies during pregnancy, increasing from just over 10% of the combined cardiac output at mid-gestation to about 25% at 30 weeks gestation4. The meeting of both flows occurs at the isthmus of the aorta and where hemodynamically the balance of biventricular output would be represented5,6.
The cardiac cycle comprises two phases that can be evaluated by Doppler flowmetry, a filling or diastolic phase with two times E and A and an emptying or systolic phase that occurs through the ventriculoarterial connections. It is possible to add the timing of these two phases that go from one isovolumetric relaxation time to the next, to obtain the integral time of the cardiac cycle in each ventricle. This would highlight the interdependence of the work of both, their close relationship with the heart rate, and in the case of the fetal heart we could assess whether or not the work, whose expenditure is combined, is in perfect equilibrium.
Impaired cardiac function can often be the first sign of fetal pathology associated with hemodynamic decompensation7-9. Therefore, the development of sensitive methods for the quantification of fetal cardiac function is of extreme importance10-12, and it should be considered that it is a combined cardiac output and that the individualized evaluation of the work of each ventricle departs from this concept.
Over the years, techniques and parameters have been proposed for the purpose of quantitative evaluation of fetal cardiac function13-20. Most were first developed in the evaluation of the adult heart and adapted to the fetus.
Our objective is to propose a performance index of systolic-diastolic function that includes both ventricles of the fetal heart individually and integrated at a single time point linked to the dependent variable with the highest degree of correlation, easily obtained and that could inform about the existence of a combined output in perfect balance.
Methods
This is a mixed, prospective, and cross-sectional study of the fetuses of 168 pregnant women between 16-38 weeks, without comorbidities, fetal anomalies or growth alterations, in which data were obtained to define the population: age of the pregnant woman, number of pregnancies, gestational age by date of last menstrual period or otherwise based on ultrasonographic study of the first 10 weeks.
The echocardiographic study in each fetus allowed us to obtain transvalvular (tricuspid and mitral) Doppler flow waves (Figure 1). The time in milliseconds was obtained from the beginning of the isovolumetric relaxation time (IVRT) of the atrioventricular wave to the same point of the following wave, referred to as the systolic-diastolic time (SDT). 3 to 5 waves were included in the sweep to facilitate the accuracy of the measurements, as illustrated in Figure 1.
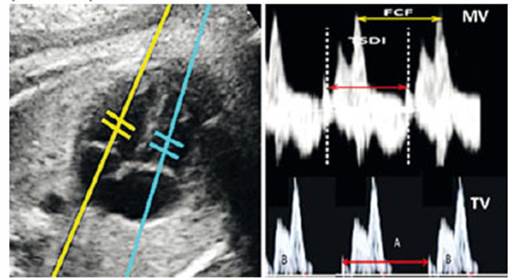
Figure 1 Doppler flow wave of the mitral valve (MV) and tricuspid valve (TV), measurement of the systolic-diastolic time index (TS DI) (red arrow).
For statistical analysis, SPSS for Windows (version 8.0, SPSS Inc.) and De Vore calculator21 were used to determine the percentage of one study group with 5th or 95th centile values included in the other, using the mean and standard deviation (SD) of the results of both ventricles. Data were expressed for each ventricle as the mean, standard deviation (SD ±), Z-score and percentiles. The value of the systolic-diastolic times of each ventricle was calculated, divided by the FHR to obtain the ventricular performance index (VPI) for each, and then the mean of both was calculated dividing the result by the average FHR to obtain the biventricular performance index (BVPI). Inferential statistical tests were used to compare the systolic-diastolic time values and univentricular and biventricular performance indexes with gestational age (GA) and fetal heart rate (FHR). Finally, a cubic model curvilinear correlation test was applied between gestational age (GA) and fetal heart rate (FHR) as independent variables and the biventricular integral performance index (BVPI) as dependent variable, in order to evaluate the degree of association and significance between both variables. The results are presented in tables and graphs adjusted to the design, accompanied by a speedometer with percentile values to facilitate the location of the proposed indexes.
Results
The mean age of the patients was 28 years (SD ±6), 72 primigravidae (42.9%), 90 with 2-3 (53.6%) gestations and 6 with more than 3 (3.6%), without medical or gestational comorbidities, with fetuses without anomalies and with growth curve appropriate to gestational age. Gestational age was between 16-38 weeks. Figure 2 shows the distribution according to mean, standard deviation, percentiles and Z-score of the values of systolic-diastolic times of both ventricles (SDTRV, SDTLV), the average time between both (MBVT) and the biventricular performance index (BVPI). The mean and dispersion values of the systolic-diastolic times of both ventricles expressed in milliseconds were 420.8±28.3 for the right ventricle and 418.8±26.3 for the left ventricle. Only 5% and 3% of the left ventricular values were below 1.65 ZS (<P5) and above this value +1.65 (>P95) of the values referred to the right ventricle. The biventricular performance index values were 2.87 (P50), 2.28 (P5) and 3.58 (P <95).
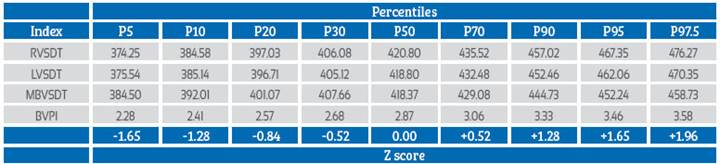
Figure 2 Distribution according to mean, standard deviation, percentiles and Z-score of the values of systolic-diastolic times of both ventricles (RVSDT and LVS DT), mean biventricular systolic-diastolic time (MBVSDT) and biventricular performance index (BVPI). Only 5% and 3% of LVS DT values are located below 1.65 ZS (<P5) and above this value +1.65 (>P95), with respect to RVSDT values (paired samples Student's t, t=0.899, p=0.371, NS). RVSDT: right ventricular systolic-diastolic time, LVS DT: left ventricular systolic-diastolic time, MBVS DT: mean biventricular systolic-diastolic time. BVPI=MBVSDT/FHR: mean biventricular systolic-diastolic time / fetal heart rate.
Figure 3 shows the mean values and their respective 95%CI for right ventricular systolic-diastolic time, left ventricular systolic-diastolic time and average. When comparing the mean values and their dispersion measures (SD) of the systolic-diastolic times of each ventricle with the mean time value of both by Student's t-test of the three paired samples, no statistically significant differences were found, t=0.98 (NS). The correlation between the systolic-diastolic time (SDT) of each ventricle with gestational age, although significant (p<0.05), was low (Spearman's r=0.34 for the right ventricle and 0.30 for the left ventricle). The correlation between the systolic-diastolic time of each ventricle and FHR was negative, -0.491 for the right and -0.553 for the left, both significant (p<0.05). In view of this dependence and the non-difference between ventricular SD times, we proceeded to calculate the mean biventricular time (MBVT) with values of 418.37 (SD±20.59), whose correlation with gestational age was 0.48 and with FHR -0.50 (p<0.05).
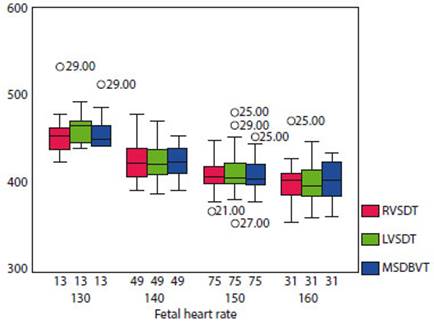
Figure 3 Box plot with the mean values and their respective 95%CI of RVS DT (right ventricular systolic-diastolic time), LVS DT (left ventricular systolic-diastolic time), and MS DBVT (average, correlation of biventricular systolic-diastolic time), as a function of GA R2=0.48 (NS ), with FHR R²= - 0.50 (p<0.05). Correlation of mean biventricular systolic-diastolic time (MS DBVT ) with GA = 0.39, p<0.05 and with FHR = - 0.52, p<0.05 (see Figure 4).
The biventricular performance index (BVPI) calculated by the formula biventricular averaging time divided by FHR (BVT/FHR) showed a highgrade bivariate correlation with FHR values (0.78, p<0.05) and a low-grade correlation with GA (0.27). The inverse model curvilinear correlation test between fetal heart rate (FHR) as the independent variable and biventricular performance index (BVPI) as the dependent variable yielded the predictive equation values (b0=-1.4377 and b1=629.457), with an R² of 0.771, p<0.05) (Figure 4).
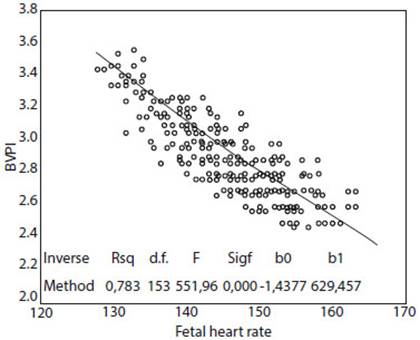
Figure 4 Dispersogram of BVPI values as a function of mean FHR for the time of the study. Correlation inverse method R²=0.783, p<.005.
Figure 5 shows a speedometer-type graph that allows us to locate both the ventricular performance index and the biventricular performance index according to percentiles. Values located in the green zone would show balance and, in case of imbalance, alert (yellow) and red (alarm). If the values for each ventricle are different but are located in the green zone, they should be considered adequate; if the calculation was made for the VBPI and it is located in the green zone, it is equivalent to balanced cardiac output; if in the yellow zone, it is a danger of imbalance; and in red, evident imbalance.
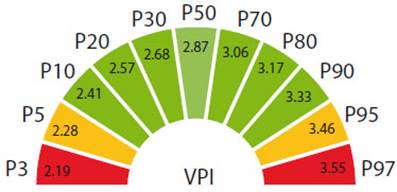
Figure 5 Speedometer-type graph (VPI: ventricular performance index) that gathers values according to percentiles and allows quick orientation to locate the SDT/FHR values for each ventricle in case of adjusted values (green zone) or in case of imbalance, alert (yellow) and alarm (red). If the values for each ventricle are different but are in the green zone, these values should be considered as adequate; if the calculation was made for the VPI and is in the green zone, it is equivalent to balanced cardiac output; in the yellow zone it is danger of imbalance and red, evident imbalance.
Discussion
There have been many and varied strategies for the evaluation of fetal cardiac output22-29. Their advantages and disadvantages have been insisted upon, and several alternatives have been proposed27. In addition, some of them present certain limitations, such as modalities that evaluate only univentricular systolic or diastolic function, formulas with difficulties in their application that limit their diffusion, the requirement of advanced technology that is not available to all those who use ultrasonography and, finally, the evaluation of the efficiency and efficacy of the techniques with reference to their usefulness in clinical decision making. Filling (diastole) and ejection (systole) times can be measured by Doppler flowmetry30-35, obtaining ventricular filling waves (E and A) and ejection waves through the sigmoid valves (ET).
Ventricular or diastolic filling is biphasic and comprises the period beginning with the isovolumetric relaxation time (IVRT) and ending with AV valve closure (sum of E and A waves), which means that the result of diastolic function is the sum of IVRT + E/A time.
The systolic period begins with the isovolumetric contraction time (IVCT) and ends with sigmoid valve closure, ending the ejection time (ET). Consequently, systolic function corresponds to the sum of IVCT + ET. Therefore, the cardiac cycle corresponds to the sum of systolic time and diastolic time. The dependence between both functions is obvious -there is a close correlation between preload and afterload- and if an integral index is sought to evaluate both functions, the totality of the times should be taken into account and not as the TEI does33,34, which only takes into account a relationship between ejection time and filling time (TE/TLL) and not the total duration of the cycle. Thus, to evaluate systolic-diastolic performance, it is necessary to know the total time of both functions for each ventricle, the correlation between them and whether there are significant differences between these times, as well as their dependence on the variables of gestational age and heart rate. The whole would make it possible to establish an index that indicates biventricular balance, a strategy that we have not found in the literature consulted2-39.
Only the mitral valve (but not the tricuspid one) flow velocity waveform allows us to observe filling and ejection at the same time due to the position of the pulmonary artery; obviously, the time between two filling waves represents the systolic time.
The fraction of filling and emptying times in both ventricles has been evaluated separately35 and in a low-risk population, finding that FHR is the only determining factor. These authors conclude that FHR influences both filling and emptying times, and that the gestational age-estimated weight ratio determines it to a low degree in ejection; therefore, accurate evaluation of filling and emptying time should include FHR.
From this point of view, the methodology we propose, which includes the evaluation of the systolic-diastolic time of each ventricle, the average value of both times, and obtaining the performance index as a function of heart rate, could be useful for the evaluation of balanced biventricular work, without ignoring the fact that the right ventricle accounts for the greatest proportion of the combined cardiac output and is the most prone to show restrictive changes in adverse hemoreologic circumstances such as intergemellar transfusion syndrome36 and restricted fetal growth37,38, circumstances in which the usefulness of the proposed strategy should be demonstrated and which will be the subject of future studies.
Likewise, taking into account the concept of the helical architecture of the myocardium described by Torrent-Guasp39, where the contraction of the basal loop (right segment) leads to emptying of the right ventricle (RV) while the apical loop of the left segment acts on the atrioventricular junction to expel the volume acquired by the left ventricle, it is to be assumed that any involvement that modifies a segment of the cardiac anatomy should cause differences between the systolic and diastolic times of the affected segment, and when compared with the reference times for normal hearts and contrasted with the heart rate, this difference would be more markedly evident.
We propose a strategy for the evaluation of fetal cardiac work of easy execution, reference values and formula for the calculation of the uni- and biventricular performance index, based on a population of low-risk fetuses. Future studies are warranted to confirm the usefulness of evaluating ventricular systolic-diastolic times of the fetal heart, individually, in their average value or by means of a biventricular performance index such as the one proposed, in these and other fetal conditions. The work does not include a comparison of the strategy with other tools used to evaluate fetal cardiac function or cases with pathologies that could have repercussions on the values of the parameters evaluated, leaving these objectives for future research.
In the present study it was possible to demonstrate that it is possible to evaluate the fetal cardiac cycle of both ventricles by means of a biventricular performance index derived from the average time of systolic-diastolic intervals of both ventricles divided by the variable fetal heart rate, which allows inferring the existence of a combined cardiac output in perfect equilibrium. The mitral valve flow velocity waveform allows us to observe filling and ejection at the same time, but not the tricuspid waveform, due to the position of the pulmonary artery. But, obviously, the time between two filling waves represents the systolic time. The proposed technique would obviate the need to obtain separate right ventricular filling and ejection times.
We consider that it is an accessible tool using standard ultrasound equipment without relying on off-line post-processing, and that it should be able to predict cardiac dysfunction before clinical signs of hemodynamic redistribution or hydrops appear. And it is here that our results allow us to point out that the biventricular performance index under normal conditions is inversely associated (decrease) with fetal heart rate significantly, and to a lesser degree with gestational age. And, values below or above the expected limits for one or both ventricles, or of the biventricular performance index, could detect failures in the performance of the fetal heart under adverse circumstances.
REFERENCES
1. Rudolph AM. Circulatory changes during gestational development of the sheep and human fetus. Pediatr Res. 2018 Sep;84(3):348-51. doi: 10.1038/s41390-018-0094-9. Epub 2018 Jul 16. PMID: 30013152 [ Links ]
2. Kiserud T. Physiology of the fetal circulation. Semin Fetal Neonatal Med. 2005 Dec;10(6):493-503. doi: 10.1016/j.siny.2005.08.007. Epub 2005 Oct 19. PMID: 16236564 [ Links ]
3. Tan CMJ, Lewandowski AJ. The Transitional Heart: From Early Embryonic and Fetal Development to Neonatal Life. Fetal Diagn Ther. 2020;47(5):373-86. doi: 10.1159/000501906. Epub 2019 Sep 18. PMID: 31533099; PMCID: PMC7265763 [ Links ]
4. Morton SU, Brodsky D. Fetal Physiology and the Transition to Extrauterine Life. Clin Perinatol. 2016 Sep;43(3):395-407. doi: 10.1016/j.clp.2016.04.001. Epub 2016 Jun 11. PMID: 27524443; PMCID: PMC4987541 [ Links ]
5. Tynan D, Alphonse J, Henry A, Welsh AW. The Aortic Isthmus: A Significant yet Underexplored Watershed of the Fetal Circulation. Fetal Diagn Ther. 2016;40(2):81-93. doi: 10.1159/000446942. Epub 2016 Jul 6. PMID: 27379710 [ Links ]
6. Chabaneix J, Fouron JC, Sosa-Olavarria A, Gendron R, Dahdah N, Berger A, Brisebois S. Profiling left and right ventricular proportional output during fetal life with a novel systolic index in the aortic isthmus. Ultrasound Obstet Gynecol. 2014 Aug;44(2):176-81. doi: 10.1002/uog.13345. Epub 2014 Jun 30. PMID: 24585706 [ Links ]
7. Abuhamad A, Chaoui R. Pulsed Doppler echocardiography. In: A practical guide to fetal echocardiography: Normal and abnormal hearts. Lippincott, Williams, and Wilkins: Philadelphia, USA, 2009. [ Links ]
8. Crispi F, Hernandez-Andrade E, Pelsers MM, Plasencia W, Benavides-Serralde JA, Eixarch E, Le Noble F, Ahmed A, Glatz JF, Nicolaides KH, Gratacos E. Cardiac dysfunction and cell damage across clinical stages of severity in growth-restricted fetuses. Am J Obstet.Gynecol. 2008 Sep;199(3):254.e1-8. doi:10.1016/j.ajog.2008.06.056. PMID: 18771973 [ Links ]
9. Godfrey ME, Messing B, Cohen SM, Valsky DV, Yagel S. Functional assessment of the fetal heart: a review. Ultrasound Obstet Gynecol. 2012 Feb;39(2):131-44. doi: 10.1002/uog.9064. Epub 2012 Jan 9. PMID: 21611999 [ Links ]
10. Allan LD, Joseph MC, Boyd EG, Campbell S, Tynan M. M-mode echocardiography in the developing human fetus. Br Heart J. 1982 Jun;47(6):573-83. doi: 10.1136/hrt.47.6.573. PMID: 7082505; PMCID: PMC481184 [ Links ]
11. Carceller-Blanchard AM, Fouron JC. Determinants of the Doppler flow velocity profile through the mitral valve of the human fetus. Br Heart J. 1993 Nov;70(5):457-60. doi: 10.1136/hrt.70.5.457. PMID: 8260278; PMCID: PMC1025359 [ Links ]
12. Carvalho JS, O'Sullivan C, Shinebourne EA, Henein MY. Right and left ventricular long-axis function in the fetus using angular M-mode. Ultrasound Obstet Gynecol. 2001 Dec;18(6):619-22. doi: 10.1046/j.0960-7692.2001.00587.x. PMID: 11844201 [ Links ]
13. Cui W, Roberson DA, Chen Z, Madronero LF, Cuneo BF. Systolic and diastolic time intervals measured from Doppler tissue imaging: normal values and Z-score tables, and effects of age, heart rate, and body surface area. J Am Soc Echocardiogr. 2008 Apr;21(4):361-70. doi: 10.1016/j.echo.2007.05.034. Epub 2007 Jul 12. PMID: 17628402 [ Links ]
14. Chao G, Zheng C, Meng D, Su J, Xie X, Li W, Henein M. Tei index: the earliest detectable cardiac structural and functional abnormality detectable in Hb Bart's foetal edema. Int J Cardiol. 2009 May 29;134(3):e150-4. doi: 10.1016/j.ijcard.2008.12.182. Epub 2009 Feb 23. PMID: 19233491 [ Links ]
15. DeVore GR. Assessing fetal cardiac ventricular function. Semin Fetal Neonatal Med. 2005 Dec;10(6):515-41. doi: 10.1016/j.siny.2005.08.009. PMID: 16257825 [ Links ]
16. Duan Y, Harada K, Wu W, Ishii H, Takada G. Correlation between right ventricular Tei index by tissue Doppler imaging and pulsed Doppler imaging in fetuses. Pediatr Cardiol. 2008 Jul;29(4):739-43. doi: 10.1007/s00246-008-9215-2. Epub 2008 Apr 29. PMID: 18443844 [ Links ]
17. Fernandez Pineda L, Tamariz-Martel Moreno A, Maître Azcárate MJ, Lopez Zea M, Rico Gómez F, Cazzaniga Bullón M, Quero Jiménez M. Contribution of Doppler atrioventricular flow waves to ventricular filling in the human fetus. Pediatr Cardiol. 2000 Sep-Oct;21(5):422-8. doi: 10.1007/s002460010101. PMID: 10982699 [ Links ]
18. Friedman D, Buyon J, Kim M, Glickstein JS. Fetal cardiac function assessed by Doppler myocardial performance index (Tei Index). Ultrasound Obstet Gynecol. 2003 Jan;21(1):33-6. doi: 10.1002/uog.11. PMID: 12528158 [ Links ]
19. Gagnon C, Bigras JL, Fouron JC, Dallaire F. Reference Values and Z Scores for Pulsed-Wave Doppler and M-Mode Measurements in Fetal Echocardiography. J Am Soc Echocardiogr. 2016 May;29(5):448-460.e9. doi: 10.1016/j.echo.2016.01.002. Epub 2016 Mar 9. Erratum in: J Am Soc Echocardiogr. 2019 Jan;32(1):169-170. PMID: 26971082 [ Links ]
20. Tsutsumi T, Ishii M, Eto G, Hota M, Kato H. Serial evaluation for myocardial performance in fetuses and neonates using a new Doppler index. Pediatr Int. 1999 Dec;41(6):722-7. doi: 10.1046/j.1442-200x.1999.01155.x. PMID: 10618901 [ Links ]
21. DeVore GR., Cuneo BF. Satou G., Sklansky M. How to determine the percentage of study subjects < 5th or > 95th centile using the control group when only the mean and standard deviation are provided. Ultrasound Obstet Gynecol. 2019; 54 (1): 139-141. doi: 10.1002/uog.20110 (Appendix S1 Calculator for determining percentage of study group with values 5th or; 95th centile using mean and SD of study and control groups. uog20110-sup-0001- AppendixS1.xlsx [ Links ]
22. Van Mieghem T, DeKoninck P, Steenhaut P, Deprest J. Methods for prenatal assessment of fetal cardiac function. Prenat Diagn. 2009 Dec;29(13):1193-203. doi: 10.1002/pd.2379. PMID: 19816885 [ Links ]
23. Van Mieghem T, Gucciardo L, Lewi P, Lewi L, Van Schoubroeck D, Devlieger R, De Catte L, Verhaeghe J, Deprest J. Validation of the fetal myocardial performance index in the second and third trimesters of gestation. Ultrasound Obstet Gynecol. 2009 Jan;33(1):58-63. doi: 10.1002/uog.6238. PMID: 18973212 [ Links ]
24. Van Splunder IP, Wladimiroff JW. Cardiac functional changes in the human fetus in the late first and early second trimesters. Ultrasound Obstet Gynecol. 1996 Jun;7(6):411-5. doi: 10.1046/j.1469-0705.1996.07060411.x. PMID: 8807756 [ Links ]
25. Gardiner HM, Pasquini L, Wolfenden J, Barlow A, Li W, Kulinskaya E, Henein M. Myocardial tissue Doppler and long axis function in the fetal heart. Int J Cardiol. 2006 Oct 26;113(1):39-47. doi: 10.1016/j.ijcard.2005.10.029. Epub 2005 Dec 19. PMID: 16360223 [ Links ]
26. Hernandez-Andrade E, López-Tenorio J, Figueroa-Diesel H, Sanin-Blair J, Carreras E, Cabero L, Gratacos E. A modified myocardial performance (Tei) index based on the use of valve clicks improves reproducibility of fetal left cardiac function assessment. Ultrasound Obstet Gynecol. 2005 Sep;26(3):227-32. doi: 10.1002/uog.1959. PMID: 16116562 [ Links ]
27. DeVore GR, Falkensammer P, Sklansky MS, Platt LD. Spatio- temporal image correlation (STIC): new technology for evaluation of the fetal heart. Ultrasound Obstet Gynecol. 2003 Oct;22(4):380-7. doi: 10.1002/uog.217. PMID: 14528474 [ Links ]
28. DeVore GR, Klas B, Satou G, Sklansky M. 24-segment sphericity index: a new technique to evaluate fetal cardiac diastolic shape. Ultrasound Obstet Gynecol. 2018 May;51(5):650-8. doi: 10.1002/uog.17505. PMID: 28437575 [ Links ]
29. Hecher K, Campbell S, Doyle P, Harrington K, Nicolaides K. Assessment of fetal compromise by Doppler ultrasound investigation of the fetal circulation. Arterial, intracardiac, and venous blood flow velocity studies. Circulation. 1995 Jan 1;91(1):129-38. doi: 10.1161/01.cir.91.1.129. PMID: 7805194 [ Links ]
30. Reed KL, Sahn DJ, Scagnelli S, Anderson CF, Shenker L. Doppler echocardiographic studies of diastolic function in the human fetal heart: changes during gestation. J Am Coll Cardiol. 1986 Aug;8(2):391-5. doi: 10.1016/s0735-1097(86)80056-0. PMID: 2942595 [ Links ]
31. Khandoker AH, Al-Angari HM, Marzbanrad F, Kimura Y. Investigating fetal myocardial function in heart anomalies by Doppler myocardial performance indices. Annu Int Conf IEEE Eng Med Biol Soc. 2017 Jul;2017:2197-200. doi: 10.1109/EMBC.2017.8037290. PMID: 29060332 [ Links ]
32. Hecher K, Campbell S, Snijders R, Nicolaides K. Reference ranges for fetal venous and atrioventricular blood flow parameters. Ultrasound Obstet Gynecol. 1994 Sep 1;4(5):381-90. doi: 10.1046/j.1469-0705.1994.04050381.x. PMID: 12797146 [ Links ]
33. Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, Tajik AJ, Seward JB. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function--a study in normals and dilated cardiomyopathy. J Cardiol. 1995 Dec;26(6):357-66. PMID: 8558414 [ Links ]
34. Pellett AA, Tolar WG, Merwin DG, Kerut EK. The Tei index: methodology and disease state values. Echocardiography. 2004 Oct;21(7):669-72. doi: 10.1111/j.0742-2822.2004.04052.x. PMID: 15488100 [ Links ]
35. Soveral I, Crispi F, Guirado L, García-Otero L, Torres X, Bennasar M, Sepúlveda-Martínez Á, Nogué L, Gratacós E, Martínez JM, Bijnens B, Friedberg M, Gómez O. Fetal cardiac filling and ejection time fractions by pulsed-wave Doppler: reference ranges and potential clinical application. Ultrasound Obstet Gynecol. 2021 Jul;58(1):83-91. doi: 10.1002/uog.22152. Epub 2021 Jun 12. PMID: 32672395 [ Links ]
36. Stirnemann JJ, Mougeot M, Proulx F, Nasr B, Essaoui M, Fouron JC, Ville Y. Profiling fetal cardiac function in twin-twin transfusion syndrome. Ultrasound Obstet Gynecol. 2010 Jan;35(1):19-27. doi: 10.1002/uog.7488. PMID: 20020467 [ Links ]
37. Harada K, Rice MJ, Shiota T, Ishii M, McDonald RW, Reller MD, Sahn DJ. Gestational age- and growth-related alterations in fetal right and left ventricular diastolic filling patterns. Am J Cardiol. 1997 Jan 15;79(2):173-7. doi: 10.1016/s0002-9149(96)00706-0. PMID: 9193018 [ Links ]
38. Youssef L, Miranda J, Paules C, Garcia-Otero L, Vellvé K, Kalapotharakos G, Sepulveda-Martinez A, Crovetto F, Gomez O, Gratacós E, Crispi F. Fetal cardiac remodeling and dysfunction is associated with both preeclampsia and fetal growth restriction. Am J Obstet Gynecol. 2020 Jan;222(1):79. e1-79.e9. doi:10.1016/j.ajog.2019.07.025. Epub 2019 Jul 20. PMID: 31336074 [ Links ]
39. Kocica MJ, Corno AF, Carreras-Costa F, Ballester-Rodes M, Moghbel MC, Cueva CN, Lackovic V, Kanjuh VI, Torrent- Guasp F. The helical ventricular myocardial band: global, three-dimensional, functional architecture of the ventricular myocardium. Eur J Cardiothorac Surg. 2006 Apr;29 Suppl 1:S21-40. doi: 10.1016/j.ejcts.2006.03.011. Epub 2006 Mar 24. PMID: 16563790 [ Links ]
Received: September 19, 2022; Accepted: October 17, 2022











 texto en
texto en 



