Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.68 no.4 Lima Oct./Dic 2022 Epub Nov 30, 2022
http://dx.doi.org/10.31403/rpgo.v68i2456
Case report
Fetal diagnosis of spinal cord filar cyst. Report of 5 cases
1. Obstetrician-Gynecologist, Hospital Nacional Daniel Alcides Carrión. Callao, Peru
5Clinica Santa Isabel, Lima, Peru
6Clínica Delgado- AUNA, Lima, Peru
The filar cyst is a rare finding in prenatal reports. Described as an image with well-defined anechogenic fluid in the center of the spinal canal below the conus medullaris, it usually has a good long-term prognosis. So far 13 cases of prenatal diagnosis have been published in the literature, we report 5 new cases and review the literature.
Key words: Cyst; filar; Filum terminale; Cyst; ventricularis terminalis; Prenatal diagnosis
Introduction
With the development of ultrasound technology, prenatal imaging of the spine in the fetus has improved, which has increased interest in searching for closed spinal dysraphisms and describing conus medullaris anatomy. Also, variants of the normal cystic aspect in the inferior medullary portion have begun to be reported, such as the filar cyst and dilatation of the terminal ventricle1.
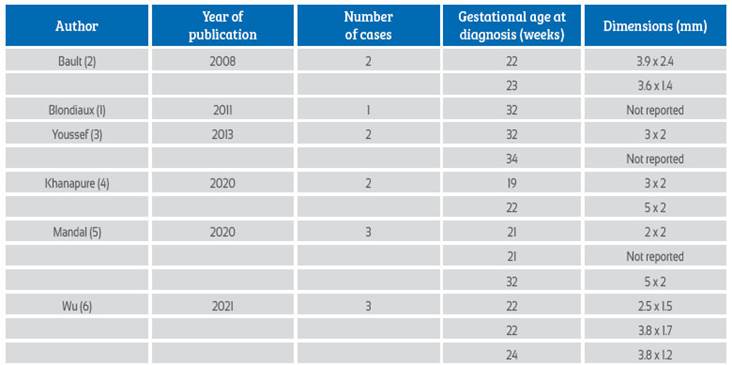
The filar cyst (FC) is a rare finding in prenatal reports. At the time of this publication, only 13 cases have been reported in the literature1-6 (Table 1). In the following, we report 5 cases of fetal-diagnostic FC.
Cases report
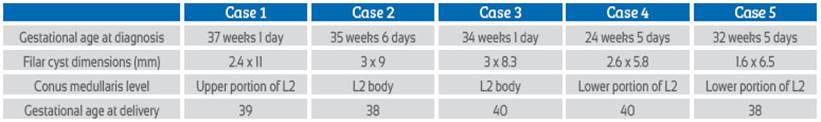
Cases were collected during 2 years in 3 institutions. The diagnoses were made in pregnant women without risk factors and during follow-up examinations.
The lumbosacral spine was evaluated along its entire length in order to determine an approximation of the osible the conus medullaris. When visualizing the conus medullaris, a cystic image of anechogenic content without connection to the ependymal canal was identified (Figures 1-5ª). Whenever osible, the finding of the filar cyst was confirmed using a high-frequency linear transducer (Figures 1-5B). A summary of the findings can be found in Table 2.
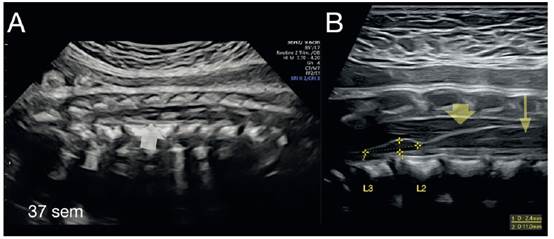
Figure 1 A) Sagittal section of the spine at the lumbosacral level allowing visualization of the conus medullaris and its position with respect to the vertebral bodies; FC is observed (gray arrow). B) Image of the conus medullaris (yellow arrow) obtained with high frequencytransducer, FC below the conus medullaris showing no connection with the ependymal duct (thin arrow).
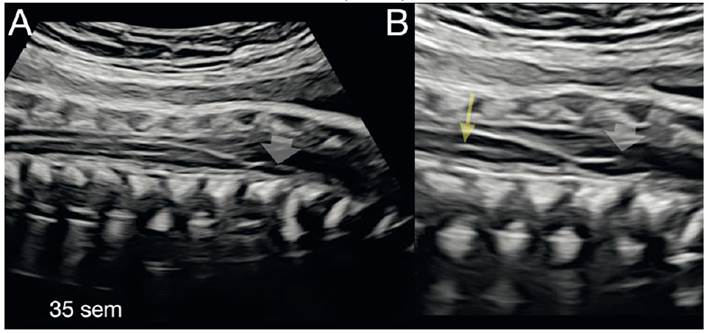
Figure 2 A) Sagittal section of the spine at the lumbosacral level showing conus medullaris and FC (gray arrow). B) Image of the conus medullaris with FC showing no connection with the ependymal duct (thin arrow).
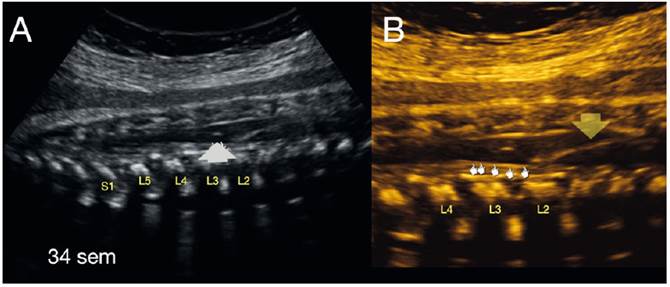
Figure 3 A) Sagittal section of the spine at lumbosacral level showing conus medullaris and its position with respect to the vertebral bodies (L2); FC is observed (gray arrow). B) Image of the conus medullaris (yellow arrow) obtained with high frequency transducer, FC below the conus medullaris.
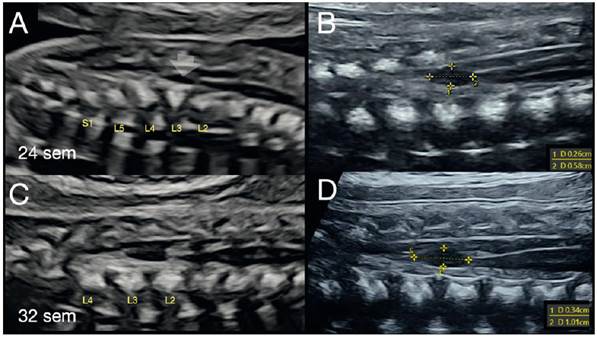
Figure 4 A) Sagittal section of the spine at lumbosacral level showing conus medullaris and FC (gray arrow). B) Image of the conus medullaris obtained with high frequency transducer; FC below the conus medullaris showing no connection with the ependymal duct. C: 32nd week control of the conus medullaris in L2 body position. D) Increase in size of the FC is observed with respect to the previous control.
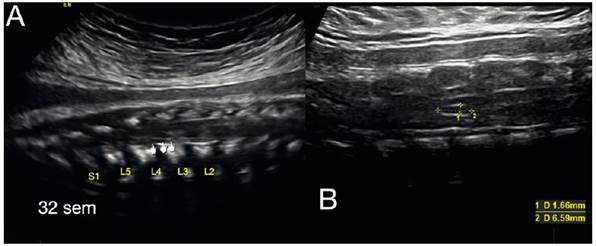
Figure 5 A) Sagittal section of the spine at lumbosacral level showing conus medullaris and FC. B) Image of the conus medullaris obtained with high frequency transducer, FC below the conus medullaris.
Discussion
Cystic lesions of the inferior segment of the medulla (conus medullaris and filum terminale) can be divided into filar cyst and terminal ventricle cyst1,4
The filar cyst is an image with well-defined anechogenic fluid in the center of the medullary canal below the conus medullaris, without internal trabeculae and without demonstrable connection to the ependymal duct or central canal (Figures 1-5B). The etiology has not been fully elucidated, although it is postulated an inadequate regression of the structures that form or are in relation to the filum terminale (ependymal cells or lags of the central canal)1-7.
The cyst of the ventricle terminale (also called fifth ventricle or Krause's cyst) constitutes an anechogenic image within the conus medullaris in which there is continuity with the ependymal canal. Unlike the FC, the cyst of the terminal ventricle can be associated with neurological problems related to sphincter control1,4,8.
FC is considered within the variants of normality in neonatal spine studies; its real incidence is still unknown. The perinatal prognosis is reported as good and only exceptional cases may be associated with other malformations such as tethered cord or lipoma of the filum terminale9,10.
Iraní9, in the largest retrospective series published with 664 infants in which spinal ultrasound was performed, found 78 cases of FC (incidence of 11.2%). In 13 of them, MRI was performed on suspicion of low conus medullaris, without being able to corroborate the persistence of FC in the MRI. Only two of the 78 cases were classified as anchored medulla in association with other malformations. An important finding of this study was that the incidence of FC decreased as the age of the infant increased. No cases were found after 6 months of age.
Another important neonatal series was published by Seo10, who considered 396 infants with sacral cutaneous stigmata for the study. In those under one month of age (196 cases) ultrasound was performed, finding 49 cases of FC; in the subsequent control with magnetic resonance imaging, only 23 persisted. In the other group in which MRI was performed (201) between 5 and 12 months of life, 7 cases of FC were found, of which only 13 cases persisted beyond one year of life. At follow-up up to 3 years, the cysts that persisted were asymptomatic; only 2 cases presented growth of the filar cyst and were associated with lipoma of the filum terminale.
Publications of fetal diagnosis so far have been occasional, with only 13 cases published (Table 1). In 2008, Bault2 reported the first two published cases. But, it was Blondiaux1, in 2011, who published the first image in a spinal ultrasound review. The cases reported so far have been in the second and third trimesters and in all, the perinatal outcomes were good. Wu6 reported 3 cases of diagnosis in the second trimester (22-24 weeks) with spontaneous resolution at 27-29 weeks, which may indicate that it was a transient finding and more frequent in the second trimester. Furthermore, this correlates with the tendency to spontaneous resolution in the neonatal stage9,10. In the cases presented in the series, most were diagnosed in the third trimester and the only second trimester case did not regress. Based on the review of published images and our own, we can configure that the charcharacteristic image of a FC would be: fusiform cyst, elongated, well defined, anechogenic, below the conus medullaris (with a variable distance), central in the medullary canal and without communication with the ependymal canal of the conus medullaris (Figures 1-5A and B).
In the present case series, the use of a high-frequency linear transducer allowed a great improvement in the visualization of both the FC and the evaluation of the conus medullaris anatomy (Figures 1-5B). Therefore, we suggest its use in the presence of suspected fetal spine pathology, given its easy accessibility(1). Or in its absence, fetal MRI may be used, although there are no cases described in the literature.
In conclusion, the filar cyst is a variant of normality rarely reported as a prenatal diagnosis. It has a good perinatal prognosis. Therefore, the recommendation would be a birth control with spinal ultrasound for corroboration and evaluation of the conus medullaris.
REFERENCES
1. Blondiaux E, Katorza E, Rosenblatt J, Nahama-Allouche C, Lenoir M, le Pointe HD, Garel C. Prenatal US evaluation of the spinal cord using high-frequency linear transducers. Pediatr Radiol. 2011;41(3):374-83. doi: 10.1007/s00247-010-1922-1 [ Links ]
2. Bault JP. P27.12: Isolated filar cyst of the lumbar spine: Report of two fetal cases. Ultrasound Obstet Gynecol. 2008;32:398-466. doi: 10.1002/uog.5942 [ Links ]
3. Youssef A, Bellussi F, Rizzo N, Pilu G, Ghi T. Cyst of the filum terminale: two cases detected on prenatal ultrasound. Ultrasound Obstet Gynecol. 2013;42(3):363-4. doi: 10.1002/uog.12524 [ Links ]
4. Khanapure B, Tinmaswala A. Antenatal diagnosis of filar cysts: an ultrasound study of 2 cases. J Fetal Med. 2020;7:317-9. doi: 10.1007/s40556-020-00276-1 [ Links ]
5. Mandal D, Roy P, Dey S. Cyst of the filum terminale: potpourri of 3 prenatally diagnosed Cases. J Fetal Med. 2020;7: 321-3. doi: 10.1007/s40556-020-00269-0 [ Links ]
6. Wu J. Spontaneous disappearance of filar cysts diagnosed by transabdominal ultrasonography: a report of three cases. J Ultrasound Med. 2022;41(4):1009-12. doi: 10.1002/jum.15769 [ Links ]
7. Saker E, Henry BM, Tomaszewski KA, Loukas M, Iwanaga J, et al. The filum terminale internum and externum: A comprehensive review. J Clin Neurosci. 2017;40:6-13. doi: 10.1016/j.jocn.2016.12.020 [ Links ]
8. Lotfinia I, Mahdkhah A. The cystic dilation of ventriculus terminalis with neurological symptoms: Three case reports and a literature review. J Spinal Cord Med. 2018;41(6):741-7. doi: 10.1080/10790268.2018.1474680 [ Links ]
9. Irani N, Goud AR, Lowe LH. Isolated filar cyst on lumbar spine sonography in infants: a case-control study. Pediatr Radiol.2006;36(12):1283-8. doi: 10.1007/s00247-006-0317-9 [ Links ]
10. Seo K, Oguma H, Furukawa R, Gomi A. Filar cysts in rare cases may progress in size, particularly when associated with filar lipoma. Childs Nerv Syst. 2019;35(7):1207-11. doi: 10.1007/s00381-019-04148-6 [ Links ]
Received: June 20, 2022; Accepted: September 27, 2022











 text in
text in