Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.1 Lima ene./mar. 2023 Epub 27-Mar-2023
http://dx.doi.org/10.31403/rpgo.v69i2473
Original paper
Could magnetic resonance imaging contribute to detecting isolated fetal ventriculomegaly other than additional abnormalities?
1. MD, Department of Perinatology, University of Health Sciences Tepecik Training and Research Hospital Izmir, Turkey
2. MD, Department of Perinatology, Bakircay University Faculty of Medicine, Cigli Training and Research Hospital, Izmir, Turkey.
3. MD, Department of Perinatology, University of Health Sciences Tepecik Training and Research Hospital Izmir, Turkey.
4. MD, Department of Obstetrics and Gynecology, Tinaztepe University Faculty of Health Sciences, Izmir, Turkey.
5. MD, Department of Obstetrics and Gynecology, Bakircay University Faculty of Medicine, Cigli Training and Research Hospital, Izmir, Turkey.
6. MD, Department of Radiology, Bakircay University Faculty of Medicine, Cigli Training and Research Hospital, Izmir, Turkey.
7. MD, Department of Perinatology, University of Health Sciences Tepecik Training and Research Hospital, Izmir, Turkey.
Objective:
To assess the role of brain magnetic resonance imaging (MRI) in fetuses presenting with isolated ventriculomegaly (IVM) in the ultrasound (US) evaluation of the fetal brain.
Methods:
US and MRI findings of 197 fetuses diagnosed with IVM between November 2018 and November 2020 were retrospectively evaluated. Fetuses with abnormal karyotypes, additional anomalies, or known etiologies for ventriculomegaly were excluded. US and MRI findings were compared both in terms of mean ventricular measurements and IVM grade.
Results:
MRI measurements were significantly higher in mild IMV (10.33 ± 0.38 mm vs. 11.11 ± 0.51 mm, p< 0.001) compared to US. In mild IVM, MRI measured ventricles larger than US with a mean difference of 0.78 mm. There was no significant difference in US and MRI measurements in terms of mean values in moderate and severe IVM. There was good agreement between US and MRI in detecting right, left and mean IVM severity (Κ=0.265, Κ=0.324, and Κ=0.261, respectively). Linear regression analyses revealed a statistically significant relationship between US and MRI measurements of the right, left, and mean IVM (p<0.001, p<0.001, and p<0.001, respectively). MRI showed perfect agreement with US in detecting IVM laterality (Κ=1.0, p<0.001).
Conclusions:
In fetuses with mild IVM detected by US, fetal brain MRI evaluation should be considered for accurate diagnosis. This approach may provide effective strategies in the antenatal management and counseling of these pregnancies.
Key words: Fetal brain; Fetal ultrasound; Magnetic resonance imaging; Hydrocephalus
Introduction
Detailed ultrasonography (USG) performed at 18-20 weeks of gestation is of great importance to detect fetal anomalies1. One of the fetal structures that should be examined during these weeks is the lateral ventricles in the fetal brain. Currently, the upper limit of lateral ventricular measurement is accepted as 10 mm2. Ventriculomegaly (VM) is the enlargement of lateral ventricles and most common central nervous system anomaly during pregnancy with a reported prevalence ranging from 1:50 to 1:1600 newborns2,3. VM is not a specific finding, and it may occur as a result of different causes, or it can be isolated without any cause. The absence of any pathology accompanying VM is called isolated VM (IVM) and it can be considered an extreme variant of normal4.
Accurate intrauterine diagnosis of fetal IVM is crucial in order to provide appropriate counseling for patients, arrange optimum management of pregnancy, give opportunity to refer patients to tertiary centers and deliver the fetus in a timely manner. US is the primary diagnostic modality for the imaging of fetal anatomy dueto its efficacy, low cost, and non-invasiveness. In recent years, fetal brain magnetic resonance imaging (MRI) is frequently recommended as an additional examination when a problem is observed in fetal neurosonographic examination. Although MRI is performed to detect pathologies that cannot be detected by US, it has not yet been clearly determined in which indications MRI is beneficial or in which cases it is superior to US5,6.
In this study, we aimed to evaluate and compare US and MRI in the measurement of the lateral ventricle diameter in fetuses with IVM.
Methods
In this cross-sectional study, the information of patients who applied to the Perinatology Department of Izmir Tepecik Training and Research Hospital between November 2018 and November 2020 were analyzed from the medical data-base. Approval for this study was obtained from the local Ethics Committee.
Pregnant women who were found to have IVM during routine fetal ultrasonographic examination were included in the study. Fetuses with a lateral ventricle width of 10 mm or greater in US examination were first evaluated for possible etiologies. Fetal karyotype analyses, congenital infection screening and a detailed fetal anomaly scan were performed to all fetuses with VM. Multiple pregnancies and pregnant women who did not have an MRI after US follow-up were ex cluded from the study. Those with concomitant infection, karyotype anomaly or additional central nervous system (CNS) anomaly were also excluded from the study.
US examinations of the fetuses were performed by perinatologists of our department. Samsung® HS 70A4D real time ultrasonography system (2017) was used as the ultrasonography device. Lateral ventricle measurement was made at the level of the atrium of the lateral ventricles. Measurement was performed by aligning the ultrasound calipers at the glomus level of the choroid plexus and positioning the calipers to the inner wall of the ventricle (Figure 1). The largest of the three measurements was recorded. In our center, MRI examinations of cases with VM detected on US are performed as soon as possible (average 2 weeks) so that they can be included in the perinatology advisory council. Fetal brain MRI were evaluated and reported by experienced clinicians at Radiology Department of our center. MRI examinations with standard protocol were performed by 1.5 T MRI systems (Siemens® Aera) using a 6-channel body coil with a radiologist monitoring. Images were acquired with T2-weighted MRI sequences: fast imaging with steady-state free precession (true FISP) and half-Fourier acquisition single-shot turbo spinecho (HASTE). Fetal brain images were performed using both techniques in axial, coronal, and sagittal planes. The widest range measured in these sections was accepted as the ventricular width. The parameters for HASTE imaging included time to repetition (TR): 1350 ms; time to echo (TE): 84 ms; flip angle (FA): 120 degrees; slice thickness: 4 mm; matrix: 256 × 256; NSA:1. The parameters of true FISP imaging were TR: 4.4 ms, TE: 2.2 ms, slice thickness: 4 mm, matrix: 240 × 256; NSA:1. MRI was performed without sedation or contrast agent (Figure 2).

Figure 2 mild (a) and moderate (b) ventriculomegaly image on mri. moderate (c) and severe (d) ventriculomegaly image on mri (a and d: coronal section, b and c: transverse section).
Patients with IVM as a result of both US and MRI were divided into 3 separate groups: 1) Mild IVM (10 mm -≤12 mm); 2) Moderate IVM (>12mm -≤15mm; 3) Severe IVM (>15mm). The VM of right and left ventricles were recorded separately.
Statistical analysis
Continuous data are given as mean ± standard deviation while categorical data are presented as percentage (%). Cohen’s kappa coefficient and intraclass correlation coefficient were used to measure reliability for categorical and continuous variables, respectively. Scatter graphs of measurement techniques were drawn. SAS Studio (SAS Institute Inc. 2015. SAS / IML® 14.1 Us er’s Guide. Cary, NC: SAS Institute Inc.) program was used in the implementation of the analysis. A p<0.05 value was accepted as the criterion for statistical significance.
Results
Demographic characteristics of the entire study population are shown in Table 1. The average age of the 197 pregnant women included in the study was 28.2±5.64 years. The mean gravidity and parity of the patients were 2.01 and 0.812, respectively. US was performed on all fetuses between 18 and 35 weeks, and fetal MRI was performed between 20 and 37 weeks of gestation in pregnant women with IVM (Table 1). The ventricular width values for both the right and left ventricle and their mean values were analyzed.
Measurements of the right ventricle by US and MRI are shown in Table 2. According to US measurements of the right ventricle, 177 (89.9%) fe-tuses had mild, 16 (8.1%), moderate and 4 (2%) severe VM. According to MRI of the right ventricle, 124 (62.9%) fetuses had mild, 63 (32%) moderate and 10 (5.1%) severe IVM. MRI measured 123 (69.5%) of fetuses with mild right VM as mild, 52 (29.4%) as moderate and 2 (1.1%) as severe right VM. MRI measured 1 (6.2%) of the fetuses with moderate right VM as mild, 11 (68.8%) as moderate and 4 (25%) as severe VM. MRI measured all 4 fetuses with severe IVM as severe IVM. MRI measurements of the right ventricle were significantly correlated with US measurements (p<0.001).
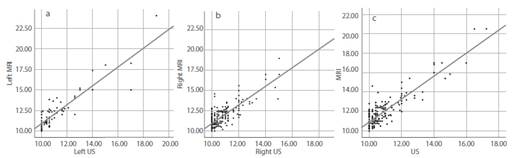
Table 2 Ventricle measurements, MRI / US compliance evaluation

Abbreviations: MRI: magnetic resonance imaging; US: ultrasound
Left ventricle measurements by US and MRI are presented in Table 2. The total number of fetuses with left VM was 83. US measurements of left VM classified 70 (8.4%) fetuses as mild, 9 (10.8%) as moderate and 4 (4.8%) as severe IVM. MRI measurements of the left ventricle classified 51 (61.5%) fetuses as mild, 24 (28.9%) as moderate and 8 (9.6%) as severe IVM. MRI measured 50 (71.4%) fetuses with mild left IVM as mild, 20 (28.6%) of them as moderate and none as severe IVM. MRI measured 1 (11.1%) of fetuses with moderate left IVM as mild, 4 (44.4%) as moderate and 4 (44.4%) as severe IVM. MRI measured all 4 fetuses with severe IVM as severe IVM. MRI measurements of the left ventricle correlated significantly with US measurements (p<0.001).
When we evaluated the consistency between US and MRI by comparing the mean values of both ventricles in the three categories, a statistically significant association was observed between the two techniques (Table 2) (p<0.001). A fair agreement was observed between US and MRI for detecting the severity of right, left and mean IVM (Κ=0.265, Κ=0.324 and Κ=0.261, respectively). Compared to US, MRI measurements were significantly higher for right mild IVM (10.34 ± 0.43 vs 11.05 ± 0.54, p<0.001), right severe IVM (16.12 ± 2.25 vs 19.50 ± 2.51, p=0.013) and left mild IVM (10.35 ± 0.36 vs 11.10 ± 0.55, p<0.001). However, when we evaluated the mean values of both ventricles, it was observed that MRI measurements were significantly higher only for mild IVM (10.33 ± 0.38 vs 11.11 ± 0.51, p<0.001) compared to US. In mild IVM, MRI measured larger ventricles than US at a mean difference of 0.78 mm. There was no significant difference between US and MRI measurements in terms of mean values of moderate and severe IVM.
Furthermore, linear regression analyses revealed statistically significant relationship be tween US and MRI measuremets of right, left and mean IVM (p<0.001, p<0.001 and p<0.001, respectively) (Figure 3). This positive correlation between US and MRI was found to be moderate for right IVM (r=0.674) and strong for left (r=0.780) and mean IVM (r=0.717) (Table 3 and Figure 3). Finally, laterality of IVM was compared in all fetuses. MRI showed perfect agreement with US in detecting laterality of IVM (Κ=1.0, p<0.001). Unilateral IVM was detected by US in 113 of 197 fetuses. All of these were evaluated as unilateral IVM by MRI. Similarly, all 84 fetuses who had bilateral IVM by US were also found to have bilateral IVM by MRI.
Table 3 MRI / US compliance evaluation.
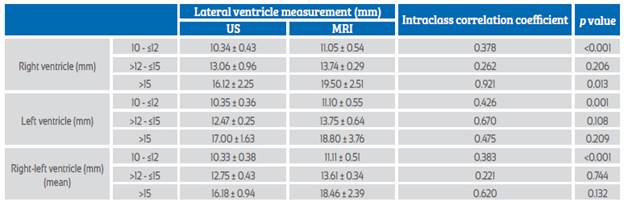
Abbreviations: MRI: magnetic resonance imaging; US: ultrasonography
Discussion
Technological advancements in recent years have also been reflected in medical applications, especially in imaging methods. Innovations in both US and MRI devices bring improvements in clinical practice. US examination has become a part of routine obstetric care because it is safe, non-invasive, readily available, and widely acceptable. However, it is not possible to define those characteristics for MRI. Both the high cost and the need for specialized personnel to perform the procedure hinder the use of MRI. For these reasons, it is important to identify patients who are candidates for MRI in clinical practice. Our findings revealed the answer to the ques tion 'when should MRI be considered in patients with IVM on US examination?’.
We found that 30.5% of fetuses with right mild IVM and 29.6% of fetuses with left mild IVM on US were evaluated as moderate or severe IVM by MRI. Among our fetuses with moderate IVM on US, 31.2% of fetuses with right moderate IVM and 55.6% of fetuses with left moderate IVM were diagnosed as mild or severe IVM on MRI. Considering that the prognosis of moderate or severe IVM is worse than mild IVM, it can be proposed that MRI can be beneficial in cases with mild or moderate IVM on US. However, none of the fetuses with severe IVM on US were diagnosed as mild or moderate IVM by MRI. Therefore, MRI did not provide additional benefit in terms of ventricular measurement in fetuses with severe IVM compared to US.
Di Mascio et al. found that the rate of detecting central nervous system abnormalities in mild and moderate IVM with MRI was higher than with US7. In their study, fetal MRI detected as sociated anomalies in 16.8% of fetuses affected by IVM on standard US assessment. The rate of associated anomalies detected only on MRI still persisted (5%) even when neurosonography was performed. In our study, we investigated the superiority of MRI over US in differentiating the severity of IVM. The superior diagnostic performance of MRI in our fetuses with mild IVM was similar to the study of Di Mascio et al. Although mild IVM is detected in some fetuses on US, the presence of severe VM in MRI in these fetuses suggests that MRI is required in terms of detecting severe VM. Pisapia et al. reported the difference between US and MRI measurements of fetal lateral ventricular size, especially in fetuses with mild and moderate VM. They emphasized that MRI mean ventricular measurements were larger than US measurements and therefore, MRI measurement may be necessary in cases of mild and moderate ventriculomegaly. Kandula et al. reported that the median difference between ventricular size on US and MRI is 1 mm6. These findings are similar to our results8. This differ ence between MRI and US measurements may be related to the different segments and mark ings used by the two techniques to measure the ventricles. Progression of dilatation over time to MRI evaluation is also not uncommon. Lam et al. reported that in the mild ventriculomegaly category the progression can be up to 1.1 mm per week, while it can reach 1.4 mm and 3.3 mm per week respectively in the moderate and severe groups9.
In contrast to our study, Parazzini et al. found different results in a study involving 179 fetuses with mild IVM. In their study, MRI confirmed sonographic diagnosis of mild IVM in 72.6% of fetuses. Among fetuses whose MRI results differed from those of US, 19.5% were diagnosed with additional anomalies, 2.7% with moderate IVM and 5% with normal ventricles10. Based on these results, they concluded that MRI provided additional clinical information in terms of prognosis and counseling in only 1.1% of fetuses with mild IVM. Similarly, Tercanli et al. proposed that little additional morphological information can be gained from MRI after a properly performed US examination11. Malinger et al. stated that neurosonography and MRI produced similar diagnoses in most of the fetuses with CNS anomalies. They did not support the common belief of fetal brain MRI is more accurate than dedicated neurosonography and recommended MRI as an adjunct method in the case of an unclear sonographic finding12.
We observed that MRI did not change the degree of ventriculomegaly in fetuses with severe IVM. However, the degree of ventriculomegaly was found to be increased by MRI in some fetuses with mild or moderate IVM. Our study demonstrated that MRI did not contribute additional benefit for severe IVM after US assessment. A detailed neurosonography seems to be sufficient in severe VM but not in mild or moderate VM. Recently, the Eurocanadian neurosonography group published the largest study investigating the role of fetal brain MRI in detecting an associated anomaly not diagnosed on ultrasound in fetuses with mild or moderate VM7. They showed that fetal brain MRI detected an additional structural anomaly in 5.4% of fetus es with mild or moderate IVM on US. Neuronal migration and acquired anomalies such as hemorrhage were the most common anomalies that can be difficult to diagnose on US. Similar to our findings, they suggested to perform fetal brain MRI for mild or moderate IVM to rule out associated anomalies that can be potentially missed on ultrasound. Our results emphasize that MRI may provide certain benefits in mild and moderate IVM. That is, perinatal management of fe-tuses with a diagnosis of mild or moderate IVM on US could be changed following MRI assessment. Late diagnosis of severe VM may lead to increased parental stress and lack of legal options for termination of pregnancy. We also assessed the role of fetal brain MRI in detecting laterality of IVM on US. There was a significant correlation between US and MRI in terms of laterality of VM (p<0.001). Therefore, we revealed that fetal brain MRI did not additional contribute to the sonographic diagnosis of whether IVM is unilateral or bilateral.
The retrospective nature of the study poses an obstacle to generalization of the data. In addition, it would be more appropriate to have more cases to generalize the neurosonography-MRI compliance in severe IVM cases. Furthermore, although most pregnant women underwent MRI two weeks or less after US, the duration between US and MRI could affect our results. One of the strengths of our study is the exclusion of chromosomal, structural, infectious, or hemorrhagic etiologies to specify the study population as isolated. Second, the minimum gestational age for MRI was 20 weeks. It is already known that most fetal organs can be visualized in detail from the 20th week of gestation and MRI could provide additional information to that obtained by US.
Conclusions
In conclusion, our study demonstrated improvements in diagnostic capability when fetal brain MRI is performed in mild or moderate IVM detected on US. However, the benefit of MRI in fetuses with severe IVM has not proven by our findings. Accurate identification of grade of fe tal VM is crucial in prenatal diagnosis. In fetuses with mild or moderate IVM, fetal brain MRI not only contributes to staging VM but can be an important component in the choice of treatment, delivery planning and counseling. Larger and prospective studies are needed to define the actual role of MR in patients with neurosonographic detected IVM.
Acknowledgements:
None.
REFERENCES
1. Salomon LJ, Alfirevic Z, Da Silva Costa F, Deter RL, Figueras F, Ghi T, et al. ISUOG Practice Guidelines: ultrasound assessment of fetal biometry and growth. Ultrasound Obstet Gynecol. 2019;53(6):715-23. doi:10.1002/uog.20272 [ Links ]
2. Society for Maternal-Fetal Medicine (SMFM); Fox NS, Monteagudo A, Kuller JA, Craigo S, Norton ME. Mild fetal ventriculomegaly: diagnosis, evaluation, and management. Am J Obstet Gynecol. 2018;219(1):B2-B9. doi:10.1016/j.ajog.2018.04.039 [ Links ]
3. Mirsky DM, Stence NV, Powers AM, Dingman AL, Neuberger I. Imaging of fetal ventriculomegaly. Pediatr Radiol. 2020;50(13):1948-58. doi:10.1007/s00247-020-04880-1 [ Links ]
4. Lavongtheung A, Jedraszak G, Naepels P, Tourneux P, Gonfry- Jouet C, Le Moing A-G, Gondry J, Chevreau J. Should isolated fetal ventriculomegaly measured below 12 mm be viewed as a variant of the norm? Results of a 5-year experience in a prenatal referral center. J Matern-Fetal Neonatal Med. 2018;31(17):2325-31. doi:10.1080/14767058.2017.13 42801 [ Links ]
5. Blondiaux E, Garel C. Fetal cerebral imaging - ultrasound vs. MRI: an update. Acta Radiol. 2013;54(9):1046-54. doi:10.1258/ar.2012.120428 [ Links ]
6. Kandula T, Fahey M, Chalmers R, Edwards A, Shekleton P, Teoh M, Clark J, Georgen SK. Isolated ventriculomegaly on prenatal ultrasound: what does fetal MRI add? J Med Imaging Radiat Oncol. 2015;59(2):154-62. doi:10.1111/1754-9485.12287 [ Links ]
7. Di Mascio D, Sileo FG, Khalil A, Rizzo G, Persico N, Giancotti A, et al. Role of magnetic resonance imaging in fetuses with mild or moderate ventriculomegaly in the era of fetal neurosonography: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2019;54(2):164-71. doi:10.1002/uog.20197 [ Links ]
8. Pisapia JM, Sinha S, Zarnow DM, Johnson MP, Heuer GG. Fetal ventriculomegaly: Diagnosis, treatment, and future directions. Childs Nerv Syst. 2017;33(7):1113-23. doi:10.1007/s00381-017-3441-y [ Links ]
9. Lam SJ, Kumar S. Evolution of fetal ventricular dilatation in relation to severity at first presentation. J Clin Ultrasound. 2014;42(4):193-8. doi:10.1002/jcu.22124 [ Links ]
10. Parazzini C, Righini A, Doneda C, Arrigoni F, Rustico M, Lanna M, Triulzi F. Is fetal magnetic resonance imaging indicated when ultrasound isolated mild ventriculomegaly is present in pregnancies with no risk factors? Prenat Diagn. 2012;32(8):752-7. doi:10.1002/pd.3896 [ Links ]
11. Tercanli S, Prüfer F. Fetal Neurosonogaphy: Ultrasound and Magnetic Resonance Imaging in Competition. Ultraschall Med. 2016;37(6):555-7. doi:10.1055/s-0042-117142 [ Links ]
12. Malinger G, Ben-Sira L, Lev D, Ben-Aroya Z, Kidron D, Lerman- Sagie T. Fetal brain imaging: a comparison between magnetic resonance imaging and dedicated neurosonography. Ultrasound Obstet Gynecol. 2004;23(4):333-40. doi:10.1002/uog.1016 [ Links ]
Data confidentiality: Data will be shared with third parties in line with the requests of the Editor or referees.
Ethical approval: Research involving human subjects complied with all relevant national regulations, institutional policies and is in accordance with the tenets of the Helsinki Declaration (as revised in 2013). It has been approved by the authors and the local Institutional Review Board (2021/ 01-20).
Received: December 20, 2022; Accepted: January 20, 2023











 texto en
texto en