Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.1 Lima Jan./Mar. 2023 Epub Mar 27, 2023
http://dx.doi.org/10.31403/rpgo.v69i2476
Original paper
Predictors of successful vaginal delivery following cesarean section
1Specialist in Gynecology and Obstetrics, Assistant to the Obstetrics and Gynecology Service, Hospital Central "Dr. Urquinaona", Maracaibo, Venezuela.
2Doctor of Medical Sciences, Assistant of the Obstetrics and Gynecology Service, Hospital Central"Dr.Urquinaona",Maracaibo,Venezuela.
3Doctor of Clinical Medicine, School of Medicine, The University of Zulia, Maracaibo, Venezuela.
4Doctor of Clinical Medicine, School of Medicine, The University of Zulia, Maracaibo, Venezuela
5Doctor of Clinical Medicine, School of Medicine, The University of Zulia, Maracaibo, Venezuela.
6Obstetrics and Gynecology Physician, Sanitas Medical Center, Coral Springs, Florida, USA.
7Doctor of Medical Sciences, Assistant of the Obstetrics and Gynecology Service, Hospital Central"Dr.Urquinaona",Maracaibo,Venezuela.
Objective
: To determine predictors of successful vaginal delivery following primary transverse segmental cesarean section for non-recurring cause.
Methods
: Pregnant women with spontaneous onset of labor and history of cesarean section with transverse incision in the lower segment for non-recurrent cause. The trial of labor was considered successful if it ended in vaginal delivery.
Main study measures
: Maternal age, parity, frequency of labor prior to previous cesarean section, gestational age at delivery, station of fetal cephalic presentation at admission, and fetal weight.
Results
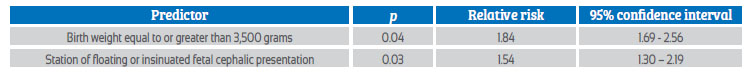
: A total of 126 pregnant women were selected, of whom 85 (67.4%) had successful trials (vaginal delivery), while 41 (32.5%) had a failed trial. No differences in general characteristics were found between groups (p = ns). Univariate analysis showed that fetal weight equal to or less than 3,500 grams, station of fixed or engaged fetal cephalic presentation, and gestational age less than 40 weeks were significant predictors of successful trial of labor outcome (p < 0.05). Logistic regression analysis showed that fetal weight equal to or greater than 3,500 grams (p = 0.04) and station of floating insinuated fetal cephalic presentation (p = 0.03) retained significance as predictors.
Conclusion
: Predictors for a successful trial of vaginal delivery following cesarean section were fetal weight less than or equal to 3,500 grams and station of fixed or engaged fetal cephalic presentation.
Key words: Vaginal birth after cesarean; Trial of labor; Fetal presentation; Fetal station; Fetal weight; Cesarean section
INTRODUCTION
Cesarean section is a common surgical procedure, but there are concerns that its frequency is steadily increasing in the last decades1-4. One of the main causes of the increase is elective surgery in patients with previous cesarean section3,5-7). Different investigations have focused their interest on the safety of vaginal birth after cesarean section (VBAC), a practice that should be encouraged to avoid the increase of pregnancy termination due to non-recurrent causes.
Several studies have shown that vaginal birth in patients with a history of cesarean section is safe8-10). Other reports have provided evidence that 60%-80% of post-cesarean trial deliveries result in successful vaginal deliveries11,12). However, caution is necessary, as complications can arise, especially in poorly equipped and understaffed obstetric care facilities (6,7).
Although most patients undergoing VBAC achieve vaginal deliveries with live newborns without the use of instruments, those who fail have a higher risk of maternal morbidity and mortality compared to those undergoing repeat cesarean section7). Several investigations have attempted to establish possible predictors of successful VBAC13,14). One of the main factors for the indication of abdominal termination of pregnancy is the history of previous cesarean section. However, those cases whose indication for termination of pregnancy is failure to progress due to cephalopelvic disproportion (recurrent cause), the success rate of VBAC is higher than when the indication is a non-recurrent cause (e.g., hemorrhage of the second half of pregnancy)15,16). In addition, patients with previous cesarean sections for second stage dystocia have a lower rate of failed tests17-19). There is also evidence of increased frequency of instrumental deliveries20).
The objective of the present investigation was to determine the predictors of successful vaginal delivery following primary transverse segmental cesarean section for nonrecurrent cause.
METHODS
A case-control study was performed with participants who were prospectively selected for VBAC trials among pregnant women who attended the high-risk prenatal consultation of the Central Hospital "Dr. Urquinaona", Maracaibo, Venezuela, between January 2019 and December 2021. The research protocol was approved by the hospital's Ethics Committee and written consent was obtained from all participants included in the study after a detailed explanation of the research objectives.
Patients were selected with a history of cesarean section by transverse incision in the lower segment for a nonrecurrent cause previously performed in the hospital, confirmed by clinical history showing indication for cesarean section, type of surgery and postoperative evolution. All the selected participants had pregnancies with singleton fetus in cephalic presentation and fetal weight estimated by ultrasound after 36 weeks less than 4,000 grams. The pelvis was assessed clinically and considered adequate by medical personnel who were independent of the study. Pregnant women with contraindications to vaginal delivery, non-reactive fetus in the non-stress test, or who refused to participate in the study were excluded. Pregnant women with successful trials were considered as cases (group A) and patients with failed trials were considered as controls (group B).
Once the diagnosis of spontaneous labor was made, a clinical evaluation was performed to establish the fetal presentation, fetal well-being parameters and availability of the patient. A peripheral venous line was cannulated and blood group and crossmatching tests were requested for the possibility of blood transfusions. The use of oxytocin to correct and increase uterine activity was left to the discretion of the attending physician. The evolution of labor was monitored using the World Health Organization partograph. Intraand postpartum complications were managed according to the service protocol for the management of each incident.
The trial was considered successful if it ended in euthocic vaginal delivery. The predictors selected for statistical analysis were maternal age, parity, frequency of labor prior to previous cesarean section, gestational age at delivery, station of fetal cephalic presentation at admission (floating insinuated or fixed engaged) and fetal weight.
Data were collected, coded and analyzed using SPSS® version 22 statistical software. Univariate analysis was used to evaluate the discriminatory capacity of each variable with successful outcome of the trial of labor (euthocic vaginal delivery). Variables with significant association at alpha 0.20 were included in a logistic regression analysis model to determine the final predictive value with a significance value of p < 0.05. The results are presented as relative risk with 95% confidence interval.
RESULTS
During the study period, 126 pregnant women were selected for the investigation. Of all participants, 85 patients (67.4%) had successful trial of labor following cesarean section (group A), while 41 women (32.5%) underwent cesarean section due to failed trial of labor (group B). The comparison between the selected maternal and fetal variables between the groups is shown in Table 1. No significant differences were found in relation to maternal age, number of pregnancies and labor before previous cesarean section (p = ns).
Table 1 association between maternal-neonatal variables and vaginal birth after cesarean section test success.

Univariate analysis showed that fetal weight less than or equal to 3,500 grams, station of fetal cephalic presentation fixed engaged and gestational age less than 40 weeks presented statistically significant values as predictors of successful VBAC (p < 0.005). Logistic regression analysis to determine relative risks and 95% confidence intervals showed that only birth weight less than or equal to 3,500 grams (p = 0.04) and station of fixed or engaged fetal cephalic presentation (p = 0.03) were significant predictors of successful vaginal birth after a cesarean section.
DISCUSSION
VBAC is desirable; moreover, the results of this study and other previous research have shown successful and safe outcomes3,6,9-12). The purpose of our study was to identify factors that increase the success rate and reduce maternal and perinatal morbidity and mortality, which could complicate the resulting trial of labor in patients with previous cesarean section.
Of the maternal and fetal variables studied that could influence successful VBAC, only fetal weight greater than or equal to 3,500 grams and the floating or insinuated fetal cephalic presentation station continued to be predictors. These findings are expected, as both parameters are related to the relationship between the fetus and pelvic capacity. Fetal weights greater than 3,500 grams are associated with higher cesarean section rates3). Therefore, it is not surprising that fetal weights below this value were associated with successful VBAC. Obviously, the smaller the fetal size, the greater the ease with which it passes through a normal-sized pelvis. Those fetuses with weights greater than 3,500 grams are more likely to produce cephalopelvic disproportion or volume dystocia, which are two of the main indications for cesarean section3,5).
The BVAC rate in this investigation was 67.4%, which places it within the suggested range 60%-80% and is slightly higher than that found in previous investigations6,8-12). The differences observed in previous reports may reflect the effects of several factors. First, the predictors used (observation, patient selection and surveillance) in this study were strictly controlled. Information obtained from medical records on the characteristics of primary cesarean section was also controlled to avoid a confounding effect on the research results. On the other hand, those institutions that perform this type of post-delivery trial on all patients with previous cesarean section are likely to have lower success rates.
The station of the fetal cephalic presentation represents the relationship between the fetus and the pelvis. The advancement of the floating or insinuated fetal cephalic presentation reflects the adequacy of the pelvic inlet and the median strait21, so it was not surprising that most patients with the extent of the fixed or engaged fetal presentation progressed to vaginal delivery.
It is noteworthy that the phrase, 'once a cesarean, always a cesarean' dates back to an article entitled 'conservatism in obstetrics' published in 191622. Although cesarean section was rarely performed at that time, the purpose was to call attention to physicians to avoid performing unnecessary cesarean sections. In that article, cesarean section was classified as 'a radical obstetric surgery' and suggested to those physicians performing it that they should determine the best possible obstetric practice to avoid having to resort to it. This famous sentence appeared in the final paragraph and was clearly intended to emphasize the risks of primary cesarean section, communicating the message that a repeat procedure might be necessary. Interestingly, the article noted that there were several exceptions to the rule, as one of the patients had three uncomplicated vaginal deliveries following cesarean section. This is remarkable, given that vertical uterine incisions were the standard at the time. The transverse arched (or Kerr's) uterine incision would be introduced a few years later23).
There are reports that VBAC can be successful in more than 60% of trials24). However, these success rates may result from the inclusion of well-selected patient groups, and the exact number of pregnant women undergoing trial of labor is unknown. Successful VBAC is associated with lower morbidity (fewer blood transfusions, postpartum infections, and hysterectomies) compared with repeat surgery25).
Although the results of this study indicate the high success rate of the BVAC trial, it is necessary to perform monitoring close to delivery and to have emergency ward availability to avoid complications such as uterine rupture, which causes both maternal and perinatal complications6. Other common complications include excessive bleeding requiring surgical exploration, hysterectomy and risk of bladder injury, in addition to the possibility of acute fetal distress26). Although uterine rupture is the most feared complication of post cesarean delivery, most studies report rates of symptomatic uterine rupture close to 1%. However, there are other reports indicating frequencies well below 1% 27).
The group of patients who present vaginal deliveries prior to cesarean section with transverse incision in the uterine segment and without contraindications for vaginal delivery are candidates for a trial of labor, which is not applicable to patients with two or more surgeries, since the risk of uterine rupture is multiplied28). It is also necessary to consider that the success rate may be higher in patients whose causes of cesarean section are iterative (e.g., fetal distress or breech presentation). Patients with a history of uterine incisions other than transverse or arcuate are also not candidates for VBAC.
CONCLUSION
The results of the present investigation demonstrate that the predictors for a successful trial of postcesarean vaginal delivery are fetal weight less than or equal to 3,500 grams and station of fixed or engaged fetal cephalic presentation. However, further research is needed to study the utility of the identified factors along with other clinical or imaging factors, in other trials. The most important aspect of this research is that the identified predictors can be measured at the time of delivery.
REFERENCES
1. Tognon F, Borghero A, Putoto G, Maziku D, Torelli GF, Azzimonti G, et al. Analysis of caesarean section and neonatal outcome using the Robson classification in a rural district hospital in Tanzania: an observational retrospective study. BMJ Open. 2019;9(12):e033348. doi: 10.1136/bmjop-en-2019-033348 [ Links ]
2. Abdo AA, Hinderaker SG, Tekle AG, Lindtjørn B. Caesarean section rates analysed using Robson's 10-Group Classification System: a cross-sectional study at a tertiary hospital in Ethiopia. BMJ Open. 2020;10(10):e039098. doi: 10.1136/bmjopen-2020-039098 [ Links ]
3. Medeiros MQ, Lima PHM, Augusto CLC, Viana BJA, Pinheiro BAK, Peixoto AB, et al. Comparison of obstetrical interventions in women with vaginal and cesarean section delivered: cross-sectional study in a reference tertiary center in the Northeast of Brazil. Ceska Gynekol. 2019;84(3):201-7. [ Links ]
4. Rose A, Raja EA, Bhattacharya S, Black M. Intervention thresholds and cesarean section rates: A time-trends analysis. Acta Obstet Gynecol Scand. 2018;97(10):1257-66. doi: 10.1111/aogs.13409 [ Links ]
5. Ogunyemi D, McGlynn S, Ronk A, Knudsen P, Andrews-Johnson T, Raczkiewicz A, et al. Using a multifaceted quality improvement initiative to reverse the rising trend of cesarean births. J Matern Fetal Neonatal Med. 2018;31(5):567-79. doi: 10.1080/14767058.2017.1292244 [ Links ]
6. Rudzinski P, Lopuszynska I, Pieniak K, Stelmach D, Kacperczyk-Bartnik J, Romejko-Wolniewicz E. Feeding practices, maternal and neonatal outcomes in vaginal birth after cesarean and elective repeat cesarean delivery. Int J Environ Res Public Health. 2022;19(13):7696. doi: 10.3390/ijerph19137696 [ Links ]
7. Dalvi SA. Difficult deliveries in cesarean section. J Obstet Gynaecol India. 2018;68(5):344-8. doi: 10.1007/s13224-017-1052-x [ Links ]
8. Gupta N, De A, Batra S. VBAC: Changes over Last 10 Years. J Obstet Gynaecol India. 2019;69(2):110-4. doi: 10.1007/s13224-018-1101-0 [ Links ]
9. Maroyi R, Naomi B, Moureau MK, Marceline BS, Ingersoll C, Nerville R, et al. Factors associated with successful vaginal birth after a primary cesarean section in women with an optimal inter-delivery interval. Int J Womens Health. 2021;13:903-9. doi: 10.2147/IJWH.S334269 [ Links ]
10. Rosman AN, van Dillen J, Zwart J, Overtoom E, Schaap T, Bloemenkamp K, van den Akker T. Lessons learned from the perinatal audit of uterine rupture in the Netherlands: A mixed-method study. Health Sci Rep. 2022;5(5):e664. doi: 10.1002/hsr2.664 [ Links ]
11. Németh G, Molnár A. Vaginal birth after cesarean section in light of international opinions. Orv Hetil. 2017;158(30):116874. doi: 10.1556/650.2017.30810 [ Links ]
12. Basile Ibrahim B, Kennedy HP, Holland ML. Demographic, socioeconomic, health systems, and geographic factors associated with vaginal birth after cesarean: An analysis of 2017 U.S. birth certificate data. Matern Child Health J. 2021;25(7):1069-80. doi: 10.1007/s10995-020-03066-3 [ Links ]
13. Dereje L, Tilahun T, Markos J. Determinants of successful trial of labor after a previous cesarean delivery in East Wollega, Western Ethiopia: A case-control study. SAGE Open Med. 2022;10:20503121221097597. doi: 10.1177/20503121221097597 [ Links ]
14. Bjellmo S, Andersen GL, Hjelle S, Klungsøyr K, Krebs L, Lydersen S, Romundstad PR, Vik T. Does caesarean delivery in the first pregnancy increase the risk for adverse outcome in the second? A registry-based cohort study on first and second singleton births in Norway. BMJ Open. 2020;10(8):e037717. doi: 10.1136/bmjopen-2020-037717 [ Links ]
15. Warren JB, Hamilton A. Clinical Inquiry: What's the best way to predict the success of a trial of labor after a previous C-section? J Fam Pract. 2015;64(12):E3-7. [ Links ]
16. Wu Y, Kataria Y, Wang Z, Ming WK, Ellervik C. Factors associated with successful vaginal birth after a cesarean section: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19(1):360. doi: 10.1186/s12884-019-2517-y [ Links ]
17. Barbounaki S, Gourounti K, Sarantaki A. Vaginal birth after cesarean section (VBAC) model using fuzzy analytic hierarch process. Acta Inform Med. 2021;29(4):275-80. doi: 10.5455/aim.2021.29.275-280 [ Links ]
18. Nahum-Yerushalmy A, Walfisch A, Lipschuetz M, Rosenbloom JI, Kabiri D, Hochler H. Uterine rupture risk in a trial of labor after cesarean section with and without previous vaginal births. Arch Gynecol Obstet. 2022;305(6):1633-9. doi: 10.1007/s00404-021-06368-1 [ Links ]
19. Gobillot S, Ghenassia A, Coston AL, Gillois P, Equy V, Michy T, Hoffmann P. Obstetric outcomes associated with induction of labour after caesarean section. J Gynecol Obstet Hum Reprod. 2018;47(10):539-43. doi: 10.1016/j.jogoh.2018.09.006 [ Links ]
20. Zhan W, Zhu J, Hua X, Ye J, Chen Q, Zhang J. Epidemiology of uterine rupture among pregnant women in China and development of a risk prediction model: analysis of data from a multicentre, cross-sectional study. BMJ Open. 2021;11(11):e054540. doi: 10.1136/bmjopen-2021-054540 [ Links ]
21. Ayenew AA, Zewdu BF. Partograph utilization as a decision-making tool and associated factors among obstetric care providers in Ethiopia: a systematic review and meta-analysis. Syst Rev. 2020;9(1):251. doi: 10.1186/s13643-020-01505-4 [ Links ]
22. Wilson RD, Caughey AB, Wood SL, Macones GA, Wrench IJ, Huang J, et al. Guidelines for antenatal and preoperative care in cesarean delivery: enhanced recovery after surgery society recommendations (Part 1). Am J Obstet Gynecol. 2018;219(6):523.e1-523.e15. doi: 10.1016/j.ajog.2018.09.015 [ Links ]
23. Vigorito R, Montemagno R, Saccone G, De Stefano R. Obstetric outcome associated with trial of labor in women with three prior cesarean delivery and at least one prior vaginal birth in an area with a particularly high rate of cesarean delivery. J Matern Fetal Neonatal Med. 2016;29(22):3741-3. doi: 10.3109/14767058.2016.1142968 [ Links ]
24. Fobelets M, Beeckman K, Faron G, Daly D, Begley C, Putman K. Vaginal birth after caesarean versus elective repeat caesarean delivery after one previous caesarean section: a cost-effectiveness analysis in four European countries. BMC Pregnancy Childbirth. 2018;18(1):92. doi: 10.1186/s12884018-1720-6 [ Links ]
25. Salman L, Hiersch L, Shmueli A, Krispin E, Wiznitzer A, Gabbay-Benziv R. Complicated primary cesarean delivery increases the risk for uterine rupture at subsequent trial of labor after cesarean. Arch Gynecol Obstet. 2018;298(2):2737. doi: 10.1007/s00404-018-4801-x [ Links ]
26. Kumari N, Jain N, Dhar RSG. Effect of a locally tailored clinical pathway tool on VBAC outcomes in a private hospital in India. J Obstet Gynaecol India. 2021;71(3):246-53. doi: 10.1007/s13224-021-01446-5 [ Links ]
27. Tesema O, Tilahun T, Kejela G. Determinants of uterine rupture at public hospitals of western Ethiopia: A case-control study. SAGE Open Med. 2022;10:20503121221092643. doi: 10.1177/20503121221092643 [ Links ]
28. Siddiqui SA. Obstetric factors for unsuccessful trial of labor in second-order birth following previous cesarean. Ann Saudi Med. 2013;33(4):356-62. doi: 10.5144/02564947.2013.356 [ Links ]
Statement of ethical issues
Ethical responsibilities: Protection of persons. The authors declare that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Confidentiality of data: The authors declare that they have followed the protocols of the Central Hospital "Dr. Urquinaona" and the University of Zulia on the publication of patient data.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Funding: The authors certify that they have not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the study.
Received: August 18, 2022; Accepted: November 26, 2022











 text in
text in