Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.1 Lima Jan./Mar. 2023 Epub Mar 27, 2023
http://dx.doi.org/10.31403/rpgo.v69i2477
Special article
Shoulder dystocia: resolution proposals according to the different birthing positions depending on the mobility of the pelvis
1. Obstetrician Gynecologist. Assistant Professor of Gynecology and Obstetrics and Academic Coordinator of Clinical Gynecology and Obstetrics, Faculty of Medical Sciences, Universidad Nacional del Litoral. Route 168 K80. Santa Fe, Argentina. CP3000
2. Pedagogue and Psychomotor Skills Specialist. Educator in Anatomy applied to Movement. Director of L'EIX - Centre of Corporal Pedagogy. Carrer Llibertat 10, Girona, Spain. CP: 17200.
3. Obstetrician and Attorney. Full Professor of Obstetrics at Hospital de Clínicas José de San Martin (Coordinating Chair), Faculty of Medical Sciences, Universidad de Buenos Aires. Paraguay 2155.C.A.B.A., Argentina. CP: C1121A6B.
4. Doctor in Medicine. Full Professor of Clinical Gynecology and Obstetrics, Faculty of Medical Sciences, Universidad Nacional del Litoral. Route 168 K80, Santa Fe, Argentina. CP3000.
Introduction:
Shoulder dystocia is a complication of vaginal delivery caused by a difficulty in delivering the fetal shoulders. It can be triggered in an unpredictable and unplanned manner, so it should be considered as a potential risk for every vaginal birth. Most of the recommendations on shoulder dystocia resolution maneuvers are made from the lithotomy position and without considering the intrinsic movements of the pelvis during labor.
Objectives
: To analyze the maneuvers for resolving shoulder dystocia based on knowledge of the biomechanics of the pelvis and its relationship with the fetal shoulders, considering the different birthing positions. Methods: Non-systematized bibliographic review.
Results
: In the case of anterior shoulder dystocia, the McRoberts maneuver with suprapubic pressure followed by extraction of the posterior arm could be recommended for a birthing woman in lithotomy position. If the birthing woman is in an upright position, it is suggested to move to the four-support position and an original variant resulting from the analysis of the biomechanics of the pelvis called ‘four-lying in asymmetry’. These maneuvers are non-invasive techniques, require minimal training and resources, and can be performed from any childbirth position.
Conclusions
: The resolution of shoulder dystocia does not have a single algorithm; it will depend on the type of dystocia, the position of the birthing woman, the context, and the greater or lesser ability of one maneuver over another. Gaskin maneuver and four supports in asymmetry should be considered before performing internal maneuvers for the resolution of shoulder dystocia.
Key words: Shoulder dystocia; Labor; Biomechanical phenomena; Patient positioning; Interdisciplinary communication
Introduction
Shoulder dystocia is a complication of vaginal delivery. The diagnosis is established when a difficulty in delivery of the fetal shoulders is identified after gentle head traction or by a delay of more than 60 seconds between the delivery of the head and the rest of the body1. When this happens, the attendant must perform additional obstetric maneuvers for a successful birth.
It is only possible to identify a high risk of shoulder dystocia in the case of estimated fetal weight greater than 5,000 g in non-diabetic pregnant women or greater than 4,500 g in diabetic pregnant women and a history of severe shoulder dystocia with brachial plexus palsy2. Beyond that, it is an unpredictable complication and there are cases in which even with appropriate resolution maneuvers it is impossible to avoid injury3. For that reason and because of its constant incidence rate over time, it should be considered and reported as an acceptable risk during delivery4.
Shoulder dystocia is not considered per se an ‘obstetric failure’ but when maternal or fetal injury is caused. This forces the training of healthcare professionals to focus on the prevention of these harms. Maternal complications are related to postpartum hemorrhage or soft tissue injuries. Neonatal complications are related to brachial plexus injuries, bone fractures, hypoxic ischemic encephalopathy and, in exceptional cases, neonatal death5,6.
Most academic publications describe the maneuvers for resolving shoulder dystocia with the patient lying on her back, without considering other childbirth positions different from lithotomy7.
This work postulates that, based on the knowledge of both pelvic mobility and shoulder dystocia physiopathology, health professionals and the pregnant woman could find strategies for its resolution regardless of the delivery position. For this purpose, reflective theoretical research with a hermeneutic approach was conducted as a result of a non-systematized bibliographic review. First, the biomechanics of the pelvis, physiology and physiopathology of shoulder delivery are analyzed. Secondly, we present, as a practical guide, a series of maneuvers for the resolution of this dystocia according to the delivery position. A novel variant called 'all fours in asymmetry' is introduced.
Development
The pelvic canal and shoulders
The descent of the shoulders during labor may be jeopardized either when entering the pelvis or on the way through the pelvic canal. This can be due -among many causes- as a result of feto-pelvic disproportion or a precipitous delivery. Understanding dystocia resolution maneuvers implies understanding the biomechanics of the pelvis and the required time for shoulder delivery.
The pelvis: its shape and intrinsic movements
The fetus must go through a non-linear path in the pelvic canal. It has a 90-degree angle curved shape between the pelvic inlet and outlet levels. In addition, these planes present different orientations and diameters that are delimited by the bony ridges and pelvic muscle-aponeurotic structures. This forces the fetus go through a curved path but also rotate along the descent in a movement similar to a ¼ - – turn screw8,9.
Schematically, the birth canal can be analyzed as an upper area or pelvic inlet, a middle area or midpelvis, and a lower area or pelvic outlet. These areas are more usually called estrechos (narrow, strait, in Spanish). We suggest revising this term since it refers to something narrow, straitened, tight, or rigid. Considering language performativity by which linguistic practices create real facts, we propose to reflect on the negative impact of this word to refer to the maternal pelvis10.
In the upright or standing position, the pelvic inlet or upper area is rounded, forward and upward-oriented, and the longest diameters are obliquus. It has an osteoarticular structure with three mobile articulations: the pubic symphysis and the two sacroiliac joints11,12.
The midpelvis has a similar but less bended orientation; on either side, sciatic spines are backward, inward, and upward-oriented. This middle area houses the deep perineal muscles or levator ani. The anteroposterior diameter is longer because the most concave part of the sacrum is behind this area13-16.
The pelvic outlet or lower space has a rhomboidal shape that is susceptible to being divided into an anterior (urogenital) triangle that faces forward and downward and a posterior (anorectal) triangle that is backward and downward oriented. This space houses the superficial and mid-perineal muscles. Functionally, the anteroposterior diameter predominates due to both the shift of the sacrum that swings forward as the fetal head pushes (among other forces) and the retropulsion of the coccyx that is moved backward during the expulsion period17,18.
When the birthing woman is in lithotomy position, the upper area is oriented upward and backward, the anterior triangle of the lower area is oriented upward and forward, and the posterior triangle remains downward and forward. When the birthing woman is in all fours position, these areas are reoriented in the opposite direction of the lithotomy position (Figure 1).
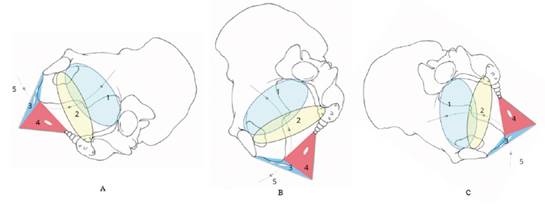
Figure 1 Pelvic spaces in vertical position (A), standing (B) and all fours (C): 1 (light blue): edge or upper area, 2 (yellow): middle area, 3 (blue): anterior triangle ofthe lower area, 4 (red): posterior triangle ofthe lower area, 5: pelvic curve. ©Núria Vives Parés
Contraction force vector makes the fetus travel through the birth canal while adjusting to the various pelvic spaces and shapes with passive movements. However, it is not a passive movement along a static canal. This canal can undergo modifications in its diameter, transform, adjust, and become available for the fetal mobile with the aid of the movements made by the birthing woman11.
The range of movement is broadened by the softening and flexibilization of sacroiliac joints and the pubic symphysis during gestation17,19,20. This is caused by hormones such as estrogens and relaxin, possibly as an adaptive evolutionary response to the growth of the fetal cranium over time16,21,22.
Bone shifts caused by sacroiliac joints and the pubis are known as intrinsic movements and result from the changes in the position of legs and vertebral spine11,23.
The sacroiliac articulation enables micromovements in the sagittal, frontal, and transverse planes23. According to Calais-Germain and Vives Parés (2009), movements in the sagittal plane are called nutation and counternutation. Sacral nutation occurs when the bone is shifted forward: the promontory moves closer to the pubic symphysis and the coccyx moves away from it. At the same time, the iliac bones can do an opposed movement called iliac nutation: the anterior superior iliac spines (ASIS) move backward and upward, and the ischiatic tuberosities move forward. This usually occurs in the expulsion period to broaden the middle and lower areas of the pelvis11,18,24.
Sacral contranutation occurs when the sacrum swings backward: the promontory moves away from the pubic symphysis, thus broadening the pelvic inlet in the sagittal plane25. Iliac bones can produce the opposite movement called iliac counteranutation: the ASIS move forward and downward, and the ischiatic tuberosities move backward. This usually occurs in the accommodation phase of the presentation when entering the upper space11,18,24 (Figure 2).
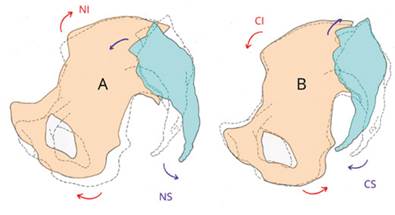
Figure 2 Pelvic movements in the sagittal plane. In red: iliac movements. In blue, sacrum movements: A: nutation movements, SN: sacral nutation (the promontory moves closer to the pubic symphysis), IN: iliac nutation (ASISmove backward) B: counternutation movements, SC: sacral counternutation (the promontory moves away from the pubic symphysis), IC: iliac counternutation (ASISmove forward). ©Nuria Vives
Combined movements in the frontal and transverse plane are called iliac supination and pronation. During iliac supination, the ASIS are shifted outward (and slightly forward) and ischia move inward (and slightly backward). This movement is produced by the external flexion and rotation of muscles in the coxofemoral joint and broadens the lateral diameter of the upper pelvic area. During pronation, the ASIS are shifted inward and backward; sciatic spines move outward (and slightly forward) and the ischia move further outward and forward. This movement is caused by the flexion and rotation of the muscles in the coxofemoral joint and broadens the lateral diameter of the middle and lower pelvic spaces11 (Figures 3 and 4).
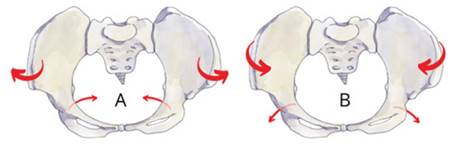
Figure 3 Movements in the frontal/transverse plane. A: Iliac supination (topview ofthe pelvis). B: Iliac supination (bottom view ofthe pelvis). The ASISare moved outward and ischia move inward. ©Nuria Vives Parés

Figure 4 All fours in asymmetry position: The flexed leg (the opposite to the fetal back) causes the iliac nutation. The knee is turned inward (blue arrow) and the heel is turned outward (red arrow) to add the iliac pronation. The asymmetry produced by this movement when broadening the middle and lower areas of the pelvis is shown with a green arrow. ©Núria Vives
Shoulders path through the birth canal
It is necessary to know the shoulders path through the birth canal to understand their dystocia. The adjustment of shoulders to the pelvic inlet coincides with the intrapelvic rotation of the fetal head. The latter makes a rotation from higher or lower amplitude -according to the childbirth position- to take a symmetrical position to the pelvis. That movement is made in a sagittal direction, usually in occipito-pubic position26.
Shoulders must follow the head movement, thus making their first rotation: from the sagittal or anteroposterior position to the transverse or obliquus position. If the back is on the left, the anterior or right shoulder is related to the right pectineal line and the posterior or left shoulder is related to the left innominate line9. The latter must enter the pelvis first since it is the most distant from the outlet and the most subjected to traction. In this way, they will descend until passing the ischiatic tuberosities. There, they will have to make a second rotation to return to the anteroposterior direction, resulting -in most cases- in an asymmetrical arrangement: one of the shoulders is overelevated and the other one is descended27.
The second shoulder rotation is produced by a mechanism that differs from the first one (internal cephalic). This would be a consequence of the internal rotation of the fetal chest (rib cage), which must pass the most curved part of the birth canal. For that, it finds more flexibility in the lateral bending and rotation movement rather than in the dorsal flexion movement. This rotation drives shoulders to the sagittal plane and enables the external cephalic restitution27. Once this is achieved, the anterior shoulder is seen to act as a pivot on the pubis to let the posterior shoulder finish its path through the sacral curve and come out first26.
Shoulder dystocia
The delivery of shoulders through the birth canal usually presents no difficulties. Even in macrosomic fetuses, the passing of shoulders through the lesser pelvis can occur in a gradual and sequential way without being stuck28. According to the previous description, from higher to lower severity, the clinical features could include:
1. Bilateral dystocia in which both shoulders are stuck above the upper pelvic space.
2. Unilateral dystocia where the posterior shoulder has entered the pelvis, but the anterior shoulder is trapped above the superior areas, over the pectineal line or the pubic symphysis (the most frequent situation)(5).
3. Difficulty in the second shoulder rotation.
If the fetal head emerges in the sagittal plane, the shoulders are rarely stuck in the same plane. They will be probably stuck in the obliquus plane. In case the fetal back is on left, the posterior shoulder will be on the left sacroiliac joint, between the sacral aileron and the innominate line; and the anterior shoulder will impact at the right pectineus line level near the pubic symphysis.
The birth attendant can notice the following signs: the face and chin cannot be identified after the head is out, the head remains firmly adhered to the vulva or it even retracts (turtle sign), the external cephalic version is not observed and shoulders do not come out29.
Once these signs are identified, the birthing woman and her relative or person of trust should be explained in a clear and plain way that there is a condition of shoulder dystocia. The patient must be asked to stop pushing since it would cause the shoulder to impact more strongly. The outcome would be the same if trying to solve the situation by using traction30,31. This also applies to the temptation to use the fingers to remove or sweep the baby’s chin that do not detach from the perineum. Direct manipulations on the head and neck are directly correlated with peripartum injuries32.
Resolution protocol
For any of the birthing positions, a series of common steps are recommended. Saying ‘shoulder dystocia’ aloud is suggested. Afterwards, we propose considering HELPER mnemotechnic (Help, Evaluate for episiotomy, Legs, Pressure, Enter maneuvers, Roll the birthing woman to her hands and knees). In spite of some debates over the order of the letters in the acronym, we hold that the wide acquaintance of the term ‘help’ that even Spanish speakers have contribute to a positive cognitive effect.
As regards the first letter of the acronym, H (help), birth attendants must call for help. They will request the presence of the following: a physician specialized in obstetrics, bachelor of obstetrics, anesthesiologist, pediatrician, nurse, and someone to record the events that occur from the shoulder dystocia diagnosis to its resolution. The record must include: time elapsed from diagnosis to shoulder delivery; chronological order and duration for each performed maneuver; the list of professionals that took part in the childbirth; health status of the baby at birth; and the report provided to parents and relatives29.
The second letter of the acronym is E (evaluation). The birth attendant must evaluate three aspects. The first one is related to the diagnosis of the type of dystocia.
Bilateral dystocia can derive from the lack of rotation and descent of the fetal head which is tried to be solved by using instrumental maneuvers or fundal pressure (Kristeller maneuver). Maneuvers such as Jacquemier-Barnum or Reverse Wood’s screw (as we will explain below) on the posterior shoulder or arm are recommended; and even a cesarean section could be required as a rescue measure although it implies a reintroduction of the fetal head, which is associated to a high mortality risk2,28,33.
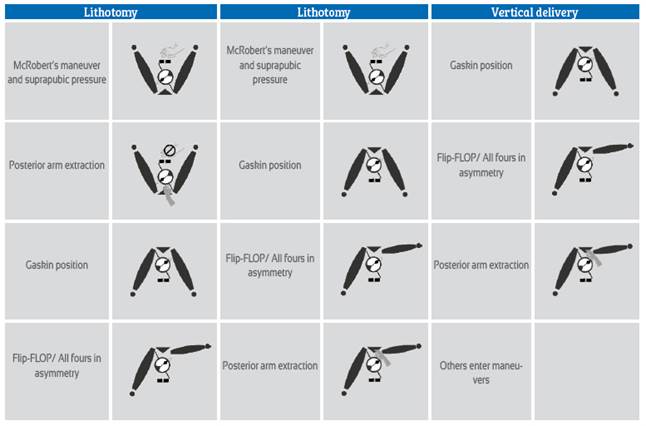
If the anterior shoulder is the affected one, the posterior shoulder will be in the pelvic cavity. In this case, we suggest performing maneuvers in the corresponding order depending on whether it is a vertical or lithotomy position.
If the difficulty arises in the second rotation of shoulders, we suggest making the patient roll to all fours, find asymmetric positions and perform maneuvers to extract the posterior arm (see resolution in vertical position)34,35.
The second aspect refers to the evaluation of the fetal back. It is useful to know that it will be on the opposite side to where the fetus is facing. The birth attendant must be there to apply suprapubic pressure and determine the direction of each maneuver. The third aspect suggests considering an episiotomy, since internal maneuvers could be needed and thus more space would be required.
Patient in lithotomy position
For lithotomy position, we suggest continuing with the third letter of HELP: L (legs). Two birth attendants -one at each side of the birthing woman- take each leg to her abdomen to produce a hyperflexion. It is the well-known McRoberts maneuver36. This maneuver causes a 1 or 2-cm shift of the pubic symphysis that enables the birth attendants to slide hands on the fetal shoulder37.
Hip flexion higher than 90 grades together with the external force made on knees and thighs causes the nutation of iliac bones. That nutation, on the one hand, takes the upper ridge of the pubic symphysis upward and backward, and on the other hand, flattens the lumbar curve37. This broadens the anteroposterior diameter of the middle and lower areas of the pelvis and allows the posterior fetal shoulder to descend and be placed in the sacral curve11,14,38.
The fourth letter of the acronym is P (suprapubic Pressure). The birth attendant that is standing at the side of the fetal back performs the external suprapubic pressure or Rubin I maneuver. The birth attendant must place hands as for cardiopulmonary reanimation (CPR) and apply pressure on the posterior part of the anterior shoulder sideward and downward. Pressure can be constant or making a swinging movement similar to that for cardiac massages. That movement is intended to settle the fetal shoulder, reduce the biacromial diameter and slide the anterior shoulder by a rotation movement under the pubic symphysis39.
Reports of success of these maneuvers are between 25-40%40,41. It must be taken into account that insisting on them could cause an increased traction and expose the baby to a higher risk of brachial plexus injury and clavicle fracture40,42.
The fifth letter of the acronym is E (internal maneuvers). Four maneuvers are described here: Rubin II, Woods maneuver, reverse Woods maneuver, and posterior arm extraction. It is worth recalling that the direction of maneuvers depends on the side of the fetal back.
1. Rubin II: The right hand should be introduced into the vagina (in 5 o’clock position if the fetal back is on the left or the fetal head is facing to the right side) and pressure should be applied counterclockwise on the posterior side of the anterior shoulder, while the birth attendant exerts suprapubic pressure. This maneuver is intended to reduce the biacromial diameter43.
2. Woods screw: If starting from the previous maneuver, the position of the right hand should remain the same and then the left hand’s fingers should be introduced into the vagina (in 7 o’clock position if the fetal back is on the left or on the same side to which the fetal head is facing) to apply pressure counterclockwise on the anterior side of the posterior shoulder. Both hands must apply pressure counterclockwise simultaneously. A birth attendant can also apply external suprapubic pressure31.
Reverse Woods screw: If starting from the previous maneuver, the left hand should be withdrawn from inside the vagina. The right hand should remain in the vagina and fingers should slide downward from the posterior side of the anterior shoulder to exert pressure clockwise. External suprapubic pressure is not recommended32.
3. Posterior arm extraction or Jacquemier-Barnum's maneuver: A hand should be introduced towards the space created by the sacral curve to find the posterior arm of the fetus. Then, pressure should be exerted on the antecubital fossa to flex the elbow, take the forearm, and move it across the chest and face to extract the posterior arm39.
The original mnemotechnic developed by the American Academy of Family Physicians (AAFP) adds a second R to the acronym HELPER (HELPERR)32. That R stands for ‘Remove the posterior arm’ or posterior arm extraction. For practical purposes, it was considered among the internal maneuvers to resolve shoulder dystocia. However, evidence suggests that it should be the first of the internal maneuvers that can be selected6,33. Several studies make this recommendation since it is associated to a lower rate of complications. This maneuver reduces the traction on the stuck shoulder and, thus, it has a protective effect on the brachial plexus elongation6,40,44,45.
The sixth letter of the acronym is R for ‘roll’. It is suggested to move the patient to Gaskin or all fours position. She will be asked to roll, helping her to find four support points on her hands and knees. The shoulder is usually unstuck due to the movement caused by the shift from supine position to all fours position46. This can be done on the floor or on the stretcher if it is wide and safe enough (the recommended maneuvers for vertical delivery will be explained in detail).
Each maneuver must be accomplished in 30 to 60 seconds at the most. If it is not effective in that period of time, the health professional must continue with the following maneuver39. According to the clinical situation, the health professional can alter the sequence of maneuvers. The report by Hoffman et al. (2011) on 2,018 cases of shoulder dystocia described an average head-to-body delivery interval of 10,7 minutes (3-20-minute range) for those newborns that presented hypoxic-ischemic encephalopathy (n=6), and also an average of more than 5 required maneuvers. Other studies suggest that this risk increases after 5 minutes from diagnosis5 , 6 , 47.
Patient in vertical position
For the patient in vertical position, it is recommended to start with the Gaskin maneuver or all fours position.
The pelvis is supported just by the hips, in particular by the femoral head (coxofemoral joint). Its three bones, the sacrum and the two iliac crests, are free to move48. This freedom somehow enables a dialogue between the fetal mobile and the pelvic canal that becomes available and adaptable to the baby’s needs on the way through the birth canal14,49. The extra benefit is the gravity force that makes the fetus go downward and towards the ischiopubic rami. This allows the posterior shoulder to slide along the sacral curve and creates more space to perform maneuvers. It could be especially useful in cases of bilateral dystocia before trying to reach the posterior shoulder or arm8,11,34,42,50.
Just switching to all fours position will probably resolve most cases of dystocia50. In case this does not occur, a novel maneuver called ‘all fours in asymmetry’ is here suggested before resorting to internal maneuvers.
‘All fours in asymmetry’ maneuver derives from the analysis of the Flip-FLOP technique created by the midwife Gail Tully51,52. Starting from all fours position, the birthing woman is asked to move the leg corresponding to the side of the fetal back: she is told to flex her hip, raise her knee, and place her foot on the floor. However, when considering the pelvis biomechanics and physiopathology of dystocia, the flexed leg should be the opposite leg to the fetal back.
If the fetal back is on the left, the anterior shoulder might tend to be blocked by the right pubis or pectineal line of the right iliac bone. When flexing the leg on this side, the iliac bone is taken to nutation: the ischium, the ischiopubic ramus, and the pubis are dragged upward and forward on the sagittal plane, broadening just one side of the middle and lower space of the pelvis and thus causing the pubis to slide underneath the stuck shoulder (as in a reverse McRoberts maneuver). If the birthing woman is further requested to produce an internal hip rotation, turning the foot and knee of the flexed leg inward and taking the heel outward, a pronation is added to the right iliac bone, broadening even further the middle and lower areas sideways.
The pelvic cavity is asymmetrical: it is noticed in the asymmetry of the two innominate lines, the sciatic spines, and the possible shearing of the pubic symphysis18. As a consequence, the oblique diameters are broader (Figure 4).
In case the delivery does not occur, the most accessible shoulder to receive the internal maneuvers is the one that rests on the sacral curve. Finding the posterior arm on the same side of the flexed leg is recommended.
Gaskin maneuver combined with all fours in asymmetry opposed to the fetal back are noninvasive external maneuvers. They require some kind of training and can be carried out without birth attendants. They can be performed from any position and in contexts with minimal resources. Even though in some texts these positions are not recommended for patients with peridural anesthesia, they can be successful after some previous training as long as that anesthesia does not cause a motor block53,54. On the other hand, these maneuvers include both the participation of the birthing woman and her companion’s collaboration. It is then reasonable to suggest these maneuvers first, regardless of the maternal birthing position, before resorting to internal maneuvers50,55 (Table 1).
Table 1 Sequence of maneuvers for resolution of anterior shoulder dystocia according to the position of the pregnant woman.
Being aware of risks, training for health professionals and patients, detailed medical records, and effective communication between health care teams and families improve obstetric results and significantly reduce litigation risks. All birth institutions must persevere in the importance of simulation training for health professional teams to optimize performance in this kind of situations as a guarantee of patients’ safety56-59.
Conclusions
Shoulder dystocia is a complication that is difficult to prevent. Its resolution requires a whole grasp of pelvis biomechanics and shoulder rotation movement during their way through the canal. This knowledge contraindicates the intuitive maneuver of making a traction movement and allows finding solutions to let shoulders out by using the pelvic spaces generated by movement.
Birth attendants count on three simple maneuvers that require just changing the body position of the birthing woman: the McRoberts maneuver, Gaskin maneuver, and all fours position in asymmetry. The latter is provided as a novel contribution. All fours positions save technical and professional resources, are accessible, and include the birthing woman as part of the answer. Their constraints, on the other hand, lay in the scarcity of academic reports on their effectiveness. In case internal maneuvers are needed, special attention should be paid to the posterior arm or shoulder to avoid the continuous traction of the brachial plexus.
Grasping the objective of each maneuver enables generating variations considering professionals’ expertise and birthing women’s preferences. That knowledge could also contribute to the fight against prejudices that still exist about vertical delivery and to keep up with the change in the paradigm of birth attendance.
Acknowledgements
The authors would like to acknowledge midwife Susanne Houd and perinatal educator Piera Maghella for their contributions to the analysis of the ‘all fours in asymmetry’ variant in shoulder dystocia resolution.
REFERENCES
1. Gherman RB. Shoulder dystocia: an evidence-based evaluation of the obstetric nightmare. Clin Obstet Gynecol. 2002;45(2):345-62. DOI: 10.1097/00003081-200206000-00006 [ Links ]
2. Raimond E, Bonneau S, Gabriel R. Distocia de hombros y parálisis obstétrica del plexo braquial. EMC-Ginecología-Obstetricia. 2022;58(2):1-14. DOI:10.1016/S1283-081X(22)46471-X [ Links ]
3. Johnson GJ, Denning S, Clark SL, Davidson C. Pathophysiologic Origins of Brachial Plexus Injury. Obstet Gynecol. 2020;136(4):725-30. DOI: 10.1097/AOG.0000000000004013 [ Links ]
4. Ouzounian JG. Shoulder Dystocia: Incidence and Risk Factors. Clin Obstet Gynecol. 2016;59(4):791-4. DOI:10.1097/GRF.0000000000000227 [ Links ]
5. American College of Obstetricians and Gynecologists' Committee on Practice Bulletins-Obstetrics, Robert BG, Joseph GO. Practice Bulletin No 178: Shoulder Dystocia. Obstet Gynecol. 2017;129(5):e123-e133. DOI:10.1097/AOG.0000000000002043 [ Links ]
6. Hoffman MK, Bailit JL, Branch DW, Burkman RT, van Veldhusien P, Li Lu et al. A comparison of obstetric maneuvers for the acute management of shoulder dystocia. Obstet Gynecol. 2011;117(6):1272-8. DOI:10.1097/AOG.0b013e31821a12c9 [ Links ]
7. Calderón J, Bravo J, Albinagorta R, Rafael P, Laura A, Flores C. Parto vertical: Retornando a una costumbre ancestral. Rev Peru Ginecol Obstet. 2008;54(1):49-57. https://doi.org/10.31403/rpgo.v54i1083 [ Links ]
8. Desseauve D, Fradet L, Lacouture P, Pierre F. Position for labor and birth: State of knowledge and biomechanical perspectives. Eur J Obstet Gynecol Reprod Biol. 2017;208:46-54. DOI:10.1016/j.ejogrb.2016.11.006 [ Links ]
9. Stansfield E, Fischer B, Grunstra NDS, Pouca MV, Mitteroecker P. The evolution of pelvic canal shape and rotational birth in humans. BMC Biol. 2021;19(1):224. DOI:10.1186/s12915-021-01150-w [ Links ]
10. Abadía MC. Transformaciones performativas: agencia y vulnerabilidad en Judith Butler. OXÍMORA Rev Intern Ética y Política. 2014;(5):1-16. [ Links ]
11. Calais-Germain B, Vives Parés N. Parir en movimiento: La movilidad de la pelvis en el parto. Barcelona: La liebre de Marzo; 2013. (El gesto anatómico). [ Links ]
12. Botell ML, Bermudez MR. El parto en diferentes posiciones a través de la ciencia, la historia y la cultura. Rev Cubana Obstet Ginecol. 2012;38(1):134-45. [ Links ]
13. Calais-Germain B. El periné femenino y el parto: Elementos de anatomía y bases de ejericios prácticos. 1ª ed. Barcelona: Los Libros de la Liebre de Marzo; 1998. (Cuerpo y consciencia). [ Links ]
14. Reitter A, Daviss B-A, Bisits A, Schollenberger A, Vogl T, Herrmann E et al. Does pregnancy and/or shifting positions create more room in a woman's pelvis? Am J Obstet Gynecol. 2014;211(6):662.e1-9. DOI:10.1016/j.ajog.2014.06.029 [ Links ]
15. Hemmerich A, Diesbourg T, Dumas GA. Development and validation of a computational model for understanding the effects of an upright birthing position on the female pelvis. J Biomech. 2018;77:99-106. DOI:10.1016/j.jbiomech.2018.06.013 [ Links ]
16. Hemmerich A, Geens E, Diesbourg T, Dumas GA. Determining loads acting on the pelvis in upright and recumbent birthing positions: A case study. Clin Biomech (Bristol, Avon). 2018;57:10-8. DOI:10.1016/j.clinbiomech.2018.05.011 [ Links ]
17. Kiapour A, Joukar A, Elgafy H, Erbulut DU, Agarwal AK, Goel VK. Biomechanics of the Sacroiliac Joint: Anatomy, Function, Biomechanics, Sexual Dimorphism, and Causes of Pain. Int J Spine Surg. 2020;14(Suppl 1):3-13. DOI:10.14444/6077 [ Links ]
18. Kapandji I. Fisiologia articular: Dibujos comentados de mecánica humana. Sexta edición. España: Editorial Médica Panamericana S.A; 2008. [ Links ]
19. Becker I, Stringer MD, Jeffery R, Woodley SJ. Sonographic anatomy of the pubic symphysis in healthy nulliparous women. Clin Anat. 2014;27(7):1058-67. DOI:10.1002/ca.22423 [ Links ]
20. Becker I, Woodley SJ, Stringer MD. The adult human pubic symphysis: a systematic review. J Anat. 2010;217(5):475-87. DOI:10.1111/j.1469-7580.2010.01300.x [ Links ]
21. Freire Vila E, La Iglesia López A de, Del Corral Lorenzo C, Canedo Carballeira ME. Dolor pélvico en la embarazada. Disfunción de la sínfisis púbica. Revisión de la literatura. Rev Soc Española del Dolor. 2010;17(7):321-5. DOI:10.1016/j.resed.2010.08.001 [ Links ]
22. Pavlicev M, Romero R, Mitteroecker P. Evolution of the human pelvis and obstructed labor: new explanations of an old obstetrical dilemma. Am J Obstet Gynecol. 2020;222(1):3-16. DOI:10.1016/j.ajog.2019.06.043 [ Links ]
23. Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012;221(6):537-67. DOI:10.1111/j.1469-7580.2012.01564.x [ Links ]
24. Zlomislic V, Garfin SR. Anatomy and Biomechanics of the Sacroiliac Joint. Techniques in Orthop. 2019;34(2):70-5. [ Links ]
25. Calais-Germain B. Anatomía para el movimiento: Tomo I. 1ra. ed. Ciudad Autónoma de Buenos Aires: Continente; 2013. [ Links ]
26. Schwarcz R, Fescina RH, Duverges CA. Obstetricia. 6a ed. Buenos Aires: El Ateneo; 2005. [ Links ]
27. Borell U, Fernström I. Radiographic studies of the rotation of the fostal shoulders during labour. Acta Obstet Gynecol Scand. 1958;37(1):54-61. DOI:10.3109/00016345809157428 [ Links ]
28. Federación Argentina de Sociedades de Ginecología y Obstetricia. Consenso de Obstetricia. Distocia de Hombros; 2005. http://www.fasgo.org.ar/archivos/consensos/condistocia.pdf [ Links ]
29. Royal College of Obstetricians and Gynaecologists. Shoulder Dystocia: Green-top Guideline No. 42 2nd Edition 2012. https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg42 [ Links ]
30. Johnstone FD, Myerscough PR. Shoulder dystocia. Br J Obstet Gynaecol. 1998;105(8):811-5. DOI:10.1111/j.1471-0528.1998.tb10223.x [ Links ]
31. Woods CE. A principle of physics as applicable to shoulder delivery. Am J Obstet Gynecol. 1943;45(5):796-804. DOI:10.1016/S0002-9378(43)90948-2 [ Links ]
32. Baxley EG, Gobbo RW. Shoulder dystocia. Am Fam Physician. 2004;69(7):1707-14. https://www.aafp.org/pubs/afp/issues/2004/0401/p1707.html [ Links ]
33. Sentilhes L, Sénat M-V, Boulogne A-I, Deneux-Tharaux C, Fuchs F, Legendre G et al. Shoulder dystocia: guidelines for clinical practice from the French College of Gynecologists and Obstetricians (CNGOF). Eur J Obstet Gynecol Reprod Biol. 2016;203:156-61. DOI:10.1016/j.ejogrb.2016.05.047 [ Links ]
34. Kovavisarach E. The »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ all-fours »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ maneuver for the management of shoulder dystocia. Int J Gynaecol Obstet. 2006;95(2):153-4. DOI:10.1016/j.ijgo.2006.06.002 [ Links ]
35. Meenan AL, Gaskin IM, Hunt P, Ball CA. A new (old) maneuver for the management of shoulder dystocia. J Fam Pract. 1991;32(06):625-9. [ Links ]
36. Gherman RB, Goodwin T, Souter I, Neumann K, Ouzounian JG, Paul RH. The McRoberts' maneuver for the alleviation of shoulder dystocia: How successful is it? Am J Obstet Gynecol. 1997;176(3):656-61. DOI:10.1016/S0002-9378(97)70565-9 [ Links ]
37. Gherman R. Analysis of McRoberts' maneuver by x-ray pelvimetry. Obstet Gynecol. 2000;95(1):43-7. [ Links ]
38. Gonik B, Zhang N, Grimm MJ. Prediction of brachial plexus stretching during shoulder dystocia using a computer simulation model. Am J Obstet Gynecol. 2003;189(4):1168-72. DOI:10.1067/S0002-9378(03)00578-7 [ Links ]
39. Huntley M, Smith JD. Management of shoulder dystocia using the HELPERR mnemonic. Brit J Midwifery. 2017;25(4):240-4. DOI:10.12968/bjom.2017.25.4.240 [ Links ]
40. Leung TY, Stuart O, Suen SSH, Sahota DS, Lau TK, Lao TT. Comparison of perinatal outcomes of shoulder dystocia alleviated by different type and sequence of manoeuvres: a retrospective review. BJOG. 2011;118(8):985-90. DOI:10.1111/j.1471-0528.2011.02968.x [ Links ]
41. Gurewitsch ED. Optimizing shoulder dystocia management to prevent birth injury. Clin Obstet Gynecol. 2007;50(3):592-606. DOI:10.1097/GRF.0b013e31811eaba2 [ Links ]
42. Gottlieb AG, Galan HL. Shoulder dystocia: an update. Obstet Gynecol Clin North Am. 2007;34(3):501-31, xii. DOI:10.1016/j.ogc.2007.07.002 [ Links ]
43. Rubin A. Management of shoulder dystocia. JAMA. 1964;189(11):835-7. DOI:10.1001/jama.1964.03070110037007 [ Links ]
44. Poggi SH, Spong CY, Allen RH. Prioritizing posterior arm delivery during severe shoulder dystocia. Obstet Gynecol. 2003;101(5, Part2):1068-72. DOI:10.1016/S0029-7844(02)02332-3 [ Links ]
45. Grimm MJ, Costello RE, Gonik B. Effect of clinician-applied maneuvers on brachial plexus stretch during a shoulder dystocia event: investigation using a computer simulation model. Am J Obstet Gynecol. 2010;203(4):339.e1-5. DOI:10.1016/j.ajog.2010.05.002 [ Links ]
46. Al Saqqa M, Khaiyon N. The »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ All-Fours »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ Maneuver for the Management of Shoulder Dystocia. Qatar Med J. 2011;2011(1):20. DOI:10.5339/qmj.2011.1.20 [ Links ]
47. TY Leung, O Stuart, DS Sahota, SSH Suen, TK Lau, TT Lao. Head-to-body delivery interval and risk of fetal acidosis and hypoxic ischaemic encephalopathy in shoulder dystocia: a retrospective review. BJOG. 2011;118(4):474-9. DOI:10.1111/j.1471-0528.2010.02834.x [ Links ]
48. Calais-Germain B, Lamotte A. Anatomía para el movimiento: Tomo II. 1a ed. Ciudad Autónoma de Buenos Aires: Continente; 2013. [ Links ]
49. Hemmerich A, Bandrowska T, Dumas GA. The effects of squatting while pregnant on pelvic dimensions: A computational simulation to understand childbirth. J Biomech. 2019;87:64-74. DOI:10.1016/j.jbiomech.2019.02.017 [ Links ]
50. Bruner JP, Drummond SB, Meenan AL, Gaskin IM. All-Fours Maneuver for Reducing Shoulder Dystocia During Labor. Obstet Gynecol Surv. 1999;54(1):17-8. DOI:10.1097/00006254-199901000-00009 [ Links ]
51. Houd S. Emergenze nel parto. Riconoscerle e gestirle in team Italia: Numeri Primi Editore; 2013. [ Links ]
52. Tully G. FlipFLOP: four steps to remember. Midwifery today with international midwife. 2012;(103):9-11. https://www.ncbi.nlm.nih.gov/pubmed/23061137 [ Links ]
53. Bothou A, Apostolidi D-M, Tsikouras P, Iatrakis G, Sarella A, Iatrakis D, et al. Overview of techniques to manage shoulder dystocia during vaginal birth. Eur J Midwifery. 2021;5:48. DOI:10.18332/ejm/142097 [ Links ]
54. Lam KK, Leung MKM, Irwin MG. Labour analgesia: update and literature review. Hong Kong Med J. 2020;26(5):413-20. DOI:10.12809/hkmj208632 [ Links ]
55. Kallianidis AF, Smit M, van Roosmalen J. Shoulder dystocia in primary midwifery care in the Netherlands. Acta Obstet Gynecol Scand. 2016;95(2):203-9. DOI:10.1111/aogs.12800 [ Links ]
56. McArdle J, Sorensen A, Fowler CI, Sommerness S, Burson K, Kahwati L. Strategies to Improve Management of Shoulder Dystocia Under the AHRQ Safety Program for Perinatal Care. J Obstet Gynecol Neonatal Nurs. 2018;47(2):191-201. DOI:10.1016/j.jogn.2017.11.014 [ Links ]
57. Dahlberg J, Nelson M, Dahlgren MA, Blomberg M. Ten years of simulation-based shoulder dystocia training- impact on obstetric outcome, clinical management, staff confidence, and the pedagogical practice - a time series study. BMC Pregn Childbirth. 2018;18(1):361. DOI:10.1186/s12884-018-2001-0 [ Links ]
58. Gurewitsch Allen ED. Simulation of Shoulder Dystocia for Skill Acquisition and Competency Assessment: A Systematic Review and Gap Analysis. Simul Healthc. 2018;13(4):268-83. DOI:10.1097/SIH.0000000000000292 [ Links ]
59. Gurewitsch Allen ED, Brown Will SE, Allen RH, Satin AJ. Improving Shoulder Dystocia Management and Outcomes With a Targeted Quality Assurance Program. Obstet Gynecol Surv. 2018;73(2):75-7. DOI:10.1097/OGX.0000000000000532 [ Links ]
The material contained in the manuscript has not been previously published or submitted to another biomedical journal
Received: October 20, 2022; Accepted: January 30, 2023











 text in
text in 



