Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.1 Lima Jan./Mar. 2023 Epub Mar 27, 2023
http://dx.doi.org/10.31403/rpgo.v69i2484
Case report
Effect of interruption in sedentary behavior on glycemic control in gestational diabetes
1Kinesiologist, Professor of Physical Education, Master in Clinical Exercise Physiology, Teacher School of Kinesiology, Faculty of Dentistry and Health, Universidad Diego Portales, Santiago, Chile. Professor, School of Kinesiology, Faculty of Health Sciences, Universidad de las Américas, Santiago, Chile. UDP, UDLA research team.
2Medical Gynecologist, Chief of Gynecology and Obstetrics, Department of Gynecology and Obstetrics, Maternal Fetal Medicine Unit, Hospital San José, Santiago, Chile. Maternal Fetal Medicine Unit, Clínica Indisa, Santiago de Chile.
3Kinesiologist, Master in Biological Sciences, mention in Physiology. Professor, School of Kinesiology, Faculty of Dentistry and Rehabilitation Sciences, Universidad San Sebastián, Santiago, Providencia, Chile. USS, UDP Research team, Santiago, Chile.
Physical activity produces beneficial effects in pregnant women. In spite of this, most of them present high levels of sedentary behavior. The objective of the study was to demonstrate the effect of a break in sedentary behavior on metabolic control in a 36-year-old patient with gestational diabetes. The intervention consisted of reorganizing her daily routine and performing a sedentary behavior break protocol. The patient achieved optimal metabolic control after the beginning of the intervention and until the end of pregnancy. The sedentary behavior break protocol added to the reorganization of the patient's routine proved to be effective in achieving glycemic control and avoiding complications associated with gestational diabetes.
Key words: Pregnancy; Diabetes; gestational; Sedentary behavior; Exercise
INTRODUCTION
Gestational diabetes (GD) is one of the most frequent complications during pregnancy1). Worldwide prevalence is estimated to be close to 18%2). More recent studies show figures between 8-26%, always associated with the age variable as a determinant parameter of higher prevalence3,4).
GD is defined as any degree of glucose intolerance that manifests itself or is detected during pregnancy. For its diagnosis, fasting glycemia values between 100-125 mg/dL on 2 different days are considered. If the values are higher than 125 mg/dL, it is considered that the patient probably had pregestational alterations5). The second parameter to be considered for the diagnosis of GD is glycemia 2 hours after glucose load (75 g); values greater than or equal to 140 mg/dL are considered altered and allow the diagnosis of GD5,6).
The treatment of GD consists of nutritional counseling, promotion of regular physical activity (PA), rigorous monitoring of the fetus and, only when the expected glycemic control is not achieved, drug treatment is resorted to7,8).
Regarding PA recommendations for 2020, the WHO9) describes that pregnant women should perform at least 150 minutes (min) of aerobic physical activity of moderate intensity. In addition, she should limit the time spent in sedentary behaviors (SB) by interrupting them even with light intensity physical activities.
SB is understood as the time spent performing activities with the minimum energy cost (1-1.5 MET (unit of measurement of the metabolic rate; 1 MET corresponds to 3.5 mL O2/kg x min) during the waking period10).
In 2017, Fazzi11) showed that pregnant women spend more than 50% of their waking time in SB. On the other hand, the American Diabetes Association establishes that pregnant women with GD or at high risk of presenting it should perform breaks in their sedentary behavior (BSB) every 30 min, practicing light exercise for at least 3 min12). It is interesting to highlight some research such as that of Fritschi13) who found that each minute in SB of a person with diabetes causes an increase of 0.12 min in hyperglycemia during the day.
In view of the above, several international entities have reached consensus on the importance of interrupting SB to improve glycemic homeostasis14,15).
We would like to report the results of a retrospective case study in which BSB was performed, in order to see how simple strategies can be used to achieve better metabolic control in patients with GD.
CASE REPORT
A 36-year-old woman, 24 weeks gestation and with no history of disease presented for medical evaluation in the 24th week of pregnancy weighing 60 kg, height 1.67 m, body mass index (BMI) 21.5 kg/m2. She was seen at a private health center in Santiago de Chile and underwent fasting glycemia and glucose afterload tests (75 g). The results were as follows: fasting glycemia 100 mg/ dL and afterload (2 h) 222 mg/dL, HbA1 7.3% and in accordance with glycemia parameters. The patient was diagnosed with gestational diabetes(5) and was referred for nutritional counseling.
From day 1 of her GD diagnosis, the patient was asked to rigorously record her self-assessed glycemia with hemoglycemic tests (Accu-Chek Guide model), with fasting and postprandial (60 and 120 min) samples taken at the three main meal times (breakfast, lunch, dinner). She was also asked to carefully record her daily food intake, which was monitored by a nutritionist, and she was instructed on her new diet. The patient maintained her pre-GD physical activity levels.
The nutritional indications focused on maintaining 5 meal times with snacks, and reinforcing that the carbohydrates consumed were high in fiber and did not exceed 75 g per meal (whole wheat bread, brown rice, corn). The importance of consuming carbohydrates in small quantities, but necessary to avoid ketosis, was emphasized. The patient's body mass index was evaluated throughout the pregnancy, showing a normal weight gain, since she started the pregnancy with 59 kg and ended with 67 kg, i.e., she had a total weight gain of 8 kg.
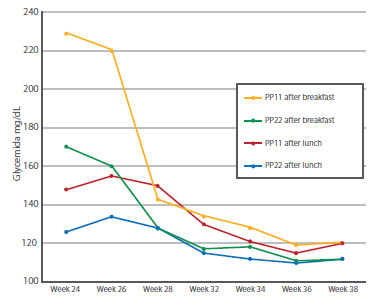
Regarding medical treatment, all the results obtained were evaluated by her attending physician during monthly check-ups until the 7th month and biweekly check-ups until the time of delivery (Figure 1). The patient did not receive any pharmacological treatment at any time during pregnancy and after being diagnosed with GD; neither was it necessary to prescribe any medication. The patient attended her medical check-up in week 26 and her glycemic control was not optimal after breakfast and lunch, in spite of complying with the nutritional recommendations (Figure 1).
Because of the above, the physician insisted that she make a change in her daily routine regarding her physical activity levels, in particular, her SB. He insisted that she should take breaks from SB and reorganize her daily routine (Figure 2).
As for the intervention with SB breaks in the patient and reorganization of her daily routine every morning, it was structured as follows: she had to drive for 60 min to get to work, so she was instructed NOT to have breakfast at home, but 10 min before arriving at work. She was emphatically prescribed to perform SB breaks every 30 min, throughout the day, according to since the intervention performed on the patient, maintaining in the last weeks of gestation values lower or equal to 120 mg/dL (Figure 1). As for the record of complications or unwanted effects due to the intervention, the patient did not report any. At week 38 (+1 day), the baby was delivered without complications, with the birth of a healthy female baby, who did not present hypoglycemia at birth; she was normal weight (3.060 kg) and had a height of 49 cm.
DISCUSSION
Exercise in pregnant women has important effects on insulin sensitivity, glut4 expression and improvement in glucose uptake16). In this regard we can refer to the meta-analysis published by Tobias16), where the results reaffirm the fact that it improves metabolic control in pregnant women who maintain physical activity programs. However, there is very little evidence of control through BSB in this population. Regarding the BSB and its benefits, this variable has a high level of evidence14-17) that is consistent with the glycemic control found in this case. Studies show a reduction in complications and weight management in type 2 DM patients, but not in the specific case of gestational diabetes. In GD, to date there is only the article published by Wagnild18) in which the time that pregnant women maintained sedentary behavior and its incidence was evaluated, finding a significant association between women with higher SB and the incidence of GD (p < 0.05). In addition, pregnant women who performed BSB had better fasting and postprandial glycemic control (p < 0.05).
Dempsey protocol14). This protocol consisted of BSB every 30 min, where the person should stand and perform 1 min of walking in place, 1 min of squats and 1 min of plantiflexion (total 3 min of exercise). It is important to mention that it was explained to the patient that the squats are at medium height and at tolerance, in order not to generate discomfort. The suggested routine was started at week 26 + 3 (Figure 2).
The patient's metabolic control showed a favorable evolution reflected in the HbA1c samples collected after the intervention since week 26, which showed a clear decrease of 5.1% in week 38 of gestation. This demonstrated optimal metabolic control and was in accordance with international recommendations to keep it under 5.5%(5.6). Regarding the postprandial capillary glycemia samples, for all feeding times, it is possible to visualize the decreases presented
In conclusion, reorganization of the physical activity routine and sedentary behavior in patients with respect to their eating schedules and intervention with breaks in sedentary behavior are simple, inexpensive and feasible strategies to prescribe to pregnant women. These sedentary behavior breaks can be implemented with self-monitoring after receiving simple and easily understood instructions for the general population, strategies that can produce significant and beneficial physiological effects in pregnant women with gestational diabetes.
REFERENCES
1. National Institute for Health and Clinical Excellence. Diabetes in pregnancy. Management of diabetes and its complications from pre-conception. Accessed 28 October 2022. Available at: https://www.nice.org.uk/guidance/ng3 [ Links ]
2. Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Hadden C. HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358(19):1991-2002. doi: 10.1056/NEJMoa0707943 [ Links ]
3. Melchior H, Kurch-Bek D, Mund M. The Prevalence of Gestational Diabetes. Dtsch Arztebl Int. 2017;114(24):412-8. doi: 10.3238/arztebl.2017.0412 [ Links ]
4. Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271-81. doi: 10.1016/j.diabres.2018.02.023 [ Links ]
5. American Diabetes Association. Standards of Medical Care in diabetes-2020. Diabetes Care. January 2022;43(Suppl 1). Accessed 19 September 2022. Available at: https://care.diabetesjournals.org/content/diacare/suppl/2019/12/20/43.Supplement_1.DC1/Standards_of_Care_2020.pdf. doi: 10.2337/dc20-S002 [ Links ]
6. Guía Diabetes y embarazo, Chile, Ministerio de Salud (MINSAL). Accessed 17 March 2021. Available at: https://www.minsal.cl/wp-content/uploads/2015/11/GUIA-DIABETES-Y-EMBARAZO [ Links ]
7. Ovesen P, Rasmussen S, Kesmodel U. Effect of Prepregnancy Maternal Overweight and Obesity on Pregnancy Outcome. Obstet Gynecol. 2011;118:305-12. doi: 10.1097/AOG.0b013e3182245d49 [ Links ]
8. Yu Y, Xie R, Shen C, Shu L. Effect of exercise during pregnancy to prevent gestational diabetes mellitus: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2017;31(12):1632-7. doi: 10.1080/14767058.2017.1319929 [ Links ]
9. WHO GUIDELINES ON PHYSICAL ACTIVITY AND SED-ENTARY BEHAVIOUR 2020. Accessed 22 September 2022. Available at: https://www.who.int/publications/i/item/9789240015128 [ Links ]
10. Cristi-Montero C. Considerations regarding sedentary and physical inactivity. Aten Primaria. 2016;48(5):341. doi: 10.1016/j.aprim.2015.09.002 [ Links ]
11. Fazzi C, Saunders DH, Linton K, Norman JE, Reynolds. Sedentary behaviours during pregnancy: a systematic review. Int J Behav Nutr Phys Act 2017;14(1):32. doi:10.1186/s12966017-0485-z [ Links ]
12. Colberg S, Sigal R, Yardley J, Riddell M, Dunstan D, Dempsey P. Physical Activity/Exercise and Diabetes: A Position Statement of. the American Diabetes Association. Diabetes Care. 2016;39:2065-79. doi: 10.2337/dc16-1728 [ Links ]
13. Fritschi C, Park H, Richardson A, Park C, Collins E, Mermelstein R. Association Between Daily Time Spent in Sedentary Behavior and Duration of Hyperglycemia in Type 2 Diabetes. Biol Res Nurs. 2016;18(2):160-6. doi: 10.1177/1099800415600065 [ Links ]
14. Dempsey PC, Dunstan DW, Larsen RN, Lambert GW, Kingwell BA, Owen N. Prolonged uninterrupted sitting increases fatigue in type 2 diabetes. Diabetes Res Clin Pract. 2018;135:128-33. doi: 10.1016/j.diabres.2017.11.001 [ Links ]
15. Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123-32. doi: 10.7326/M14-1651 [ Links ]
16. Tobias DK, Zhang C, van Dam RM, Bowers K, Hu FB. Physical activity before and during pregnancy and risk of gestational diabetes mellitus: a meta-analysis. Diabetes Care. 2011;34:223-9. doi: 10.2337/dc10-1368 [ Links ]
17. Diaz KM, Duran AT, Colabianchi N, Judd SE, Howard VJ, Hooker SP. Potential Effects on Mortality of Replacing Sedentary Time With Short Sedentary Bouts or Physical Activity: A National Cohort Study. Am J Epidemiol. 2019;188(3):537-44. doi: 10.1093/aje/kwy271 [ Links ]
18. Wagnild JM, Hinshaw K, Pollard T. Associations of sedentary time and self-reported television time during pregnancy with incident gestational diabetes and plasma glucose levels in women at risk of gestational diabetes in the UK. BMC Public Health. 2019;19(575):1-8. doi: 10.1186/s12889-0196928-5 [ Links ]
Ethical considerations: This case report complies with all ethical considerations according to the Declaration of Helsinki, in addition to legal considerations and safeguarding of confidential information. The patient authorized the publication of the data obtained with the protection of her identity, signing informed consent. The study was approved by the bioethics committee of the Diego Portales University, Santiago, Chile. The material contained in the manuscript has not been previously published or submitted to another biomedical journal.
Received: October 06, 2022; Accepted: November 26, 2022











 text in
text in