Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Peruana de Ginecología y Obstetricia
versão On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.1 Lima jan./mar. 2023 Epub 27-Mar-2023
http://dx.doi.org/10.31403/rpgo.v69i2485
Case reports
Prenatal diagnosis and follow-up of fetal cardiac tumors: case series and review of the literature
1. Instituto Nacional Materno Perinatal, Lima, Perú
2. Hospital de Apoyo II Santa Rosa, Piura, Perú
Background:
Cardiac tumors are frequent in the fetal and infant stages, with rhabdomyoma being the most prevalent in fetal life. Its diagnosis has increased due to ultrasound screening. Objective: To report the first Peruvian series of cases with prenatal diagnosis of fetal cardiac tumors in a maternal perinatal institute.
Methods:
Descriptive study of case series. The database of all fetuses with prenatal diagnosis of cardiac tumors from January 2009 to January 2021 at the Instituto Nacional Materno Perinatal (INMP), Lima, Peru, was reviewed. These patients were followed up by telephone and in two cases echocardiographic control was performed.
Results:
We found 6 cases of patients diagnosed with cardiac tumors in the last 12 years in the INMP, with reduction in size in the follow-up of all cases and association with tuberous sclerosis in half of them.
Conclusions:
Cardiac rhabdomyomas represent the most frequent tumors in fetal life. Most of them have in common the partial remission of the tumor. However, the clinical evolution depends on the location of the tumor, size, and its association or not with tuberous sclerosis. For this reason, close follow-up is recommended, especially of the central nervous system.
Key words: Rhabdomyoma; Tuberous sclerosis; Prenatal diagnosis
Introduction
Fetal cardiac tumors are infrequent, more so primary cardiac tumors1,2. According to autopsy findings in children, an incidence of 0.027%-0.08% is described1 and in fetuses it is 0.14%3. This incidence has increased tenfold in recent years due to improved prenatal ultrasound diagnosis1.
Histologically, the most common cardiac tumors are rhabdomyomas, fibromas, teratomas, myxomas, and hemangiomas, which vary in incidence across studies1-3 and according to life stage of fetuses, neonates and children.
Benign cardiac tumors are the most common in fetuses and children, with rhabdomyoma being the most frequent, representing 60% of primary cardiac tumors4. Although it is classified as benign, it can cause adverse outcomes depending on its location, size and presence of arrhythmias5. Malignant cardiac tumors represent only 10% of primary tumors4.
Cardiac rhabdomyomas were first described in 1862 by Von Recklinghausen. Histologically they are composed of the pathognomonic 'spider cells'6. They are most frequently located in the ventricles and ultrasonographically present as oval, nodular, hyperechogenic, well-defined and frequently multiple lesions7. In prenatal life and depending on their location, they can be asymptomatic, cause arrhythmias, obstruct the outflow tract, give rise to pericardial effusion, hydrops and death. At birth they are usually asymptomatic. However, there may also be cyanosis, decreased peripheral pulse and auscultation of heart murmurs. Rarely require surgical management4,8.
The prognosis of prenatally detected cardiac rhabdomyomas is favorable, since, having completed their fetal somatic growth, hamartomas lose their mitotic potential and undergo apoptosis9. The literature describes that cardiac rhabdomyomas tend to regress with time10. However, there is an association between cardiac rhabdomyomas and tuberous sclerosis. Thus, between 60-90% of cardiac rhabdomyomas have a diagnosis of tuberous sclerosis, which worsens the prognosis5,8,11. Tuberous sclerosis is a genetic syndrome whose initial manifestation is usually cardiac rhabdomyomas. In addition, they are characterized by the presence of generalized hamartomas in other tissues12.
In the present study, we describe the clinical and ultrasound characteristics and the evolution of 6 patients with prenatal diagnosis of cardiac rhabdomyoma over 12 years.
Methods
The present is a descriptive case series study, in which the database of the National Maternal Perinatal Institute (INMP), Lima, Peru, of fetuses with prenatal diagnosis of cardiac tumors, from January 2009 to January 2021, was reviewed. Data were extracted from maternal and neonatal medical records. Subsequently, the patients were followed up by telephone and echocardiographic control was performed in two of the patients at the institution. In the remaining four cases, data from other hospitals provided by the parents were considered.
Results
Ten cases were found, of which 4 were excluded because they did not have adequate postnatal follow-up. The characteristics of the mothers and the prenatal diagnosis of 6 cases of fetuses with cardiac tumors are summarized in Table 1.
Table 1 Patient characteristics and prenatal diagnosis of fetal cardiac tumors.
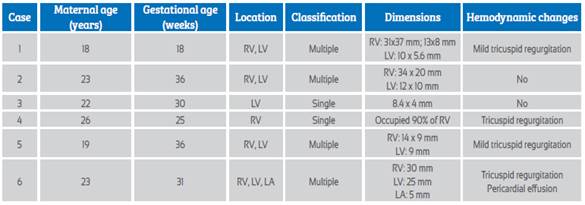
RV: right ventricle. LV: left ventricle. LA: left atrium.
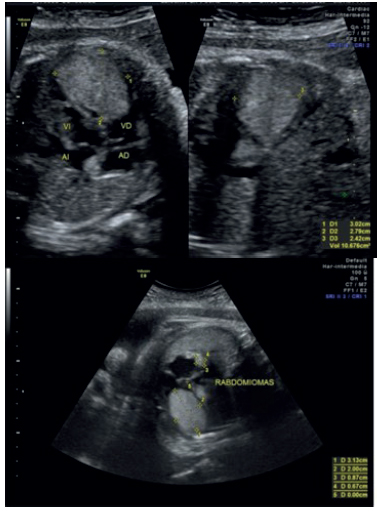
The mean age of the pregnant women at diagnosis was 21.8 years (18-26 years) and the mean gestational age was 29 weeks (18-36 weeks). Four (66.7%) were multiple and two (33.3%) were single. All cases presented tumors in the ventricles, with a similar proportion between the right and left ventricle, and in only one case a cardiac tumor was found in the left atrium. In three cases the size of the tumors was greater than 20 mm (Figure 1). In one case the size was not specified, but it was reported to occupy more than 90% of the right ventricle (Figure 2). The largest was 31 x 37 mm. In four (66.7%) cases there was mild tricuspid regurgitation. All cardiac tumors were classified as rhabdomyomas due to their echographic characteristics.
Among the perinatal outcomes (Table 2), the mean gestational age at birth was 37.7 weeks (37-38 weeks). Five (83.3%) of the newborns were female. The route of delivery was cesarean section in most cases. Only 16.7% of the newborns had low birth weight. All newborns had Apgar greater than 7 at 5 minutes.
In the follow-up, one of the infants required cardiac surgery due to hemodynamic alterations. We have institutional ultrasound evidence of decrease in tumor volume in two patients. In the rest, indirect information was obtained by telephone follow-up of the parents on the absence of cardiac tumors in the extra-institutional controls.
In 50% of the cases the patients had a diagnosis of tuberous sclerosis; of these, 66.7% had multiple cardiac tumors.
Discussion
Cardiac rhabdomyomas are the most frequent fetal tumors, although they are still considered a rare diagnosis. However, their incidence has increased with the more extensive use of ultrasonography and prenatal diagnosis1. In our institution 10 cases of cardiac tumors were identified in 12 years of study, but data are available for only 6 of them. All cases had a diagnosis of cardiac rhabdomyoma and 50% were associated with tuberous sclerosis. We have institutional ultrasound evidence of decreased tumor volume in two patients. In the rest of cases, indirect information was obtained through telephone follow-up with the parents regarding the absence of cardiac tumors in extra-institutional controls.
On ultrasonographic evaluation, rhabdomyomas are observed as ovoid, echogenic, unshaded masses that can be located in any of the four cardiac cavities, mainly in the ventricles12,13. In all our cases, rhabdomyomas were found in the ventricles, with equal predominance between both, as indicated in the literature12. In patients with tuberous sclerosis, Jóźwiak et al. found that most were located in the right ventricle (35%), followed by the left ventricle in 22%, interventricular septum in 33%, left and right atrium in 5%14.
The literature reports that 90% of rhabdomyomas are multiple12. Four of our patients (66.7%) had multiple rhabdomyomas. According to what has been reported, 70-90% of rhabdomyomas are associated with tuberous sclerosis. Our case series only found an association in half of the patients, which could mean a lower prevalence of this pathology in our country.
Cardiac rhabdomyomas tend to regress over the years in 90% of cases and do not require surgical management unless they cause severe hemodynamic decompensation. Despite this potential complication, there are currently m-THOR protein inhibitor drugs, such as everolimus, which may help to decrease the size of the tumor15. Dhulipudi et al. performed a prospective observational study in neonates with cardiac rhabdomyomas presenting with clinical symptoms or blood flow obstruction. Five neonates (100%) showed tumor regression during follow-up with everolimus. Therefore, there is potential benefit with the use of this drug in selected symptomatic cases. Multicenter studies are still needed to determine its safety and efficacy in a larger population 16.
Cardiac rhabdomyomas are usually asymptomatic. However, depending on their size and location, they may cause obstruction to blood flow, hemodynamic alteration, presence of arrhythmias, pericardial effusion, hydrops and fetal death8. Chao et al. found that a size greater than 20 mm was associated with an increased risk of perinatal death17. Likewise, Okmen F et al. found that cardiac tumor size was associated with perinatal mortality18. In our series, there was no evidence of neonatal death despite the size of the tumor greater than 20 mm. However, 66.7% had mild tricuspid regurgitation on prenatal ultrasound, with only one of them presenting hemodynamic decompensation.
It is important to highlight that there is an association between fetal cardiac rhabdomyomas and tuberous sclerosis in up to 80% of cases. This pathology affects various organs, with the worst prognosis being the involvement of the nervous system, so one of the most frequent symptoms is epilepsy (83%). Early diagnosis and management are important to improve cognitive outcomes19. The fatal complications described are renal angiolipoma, sudden unexpected death associated with epilepsy, pulmonary lymphomyolipoma, subependymal giant cell astrocytoma and pancreatic cancer20. In our series, 50% of the children had a diagnosis of tuberous sclerosis. Due to this association, a comprehensive evaluation is required when cardiac rhabdomyomas are diagnosed, and magnetic resonance imaging should be performed to look for hamartomas in other locations such as brain, kidney and others, in order to provide counseling to family members and timely multidisciplinary management.
Among the limitations of this presentation, we should point out that 4 patients were lost to follow-up due to migration to another city, genetic study of tuberous sclerosis was not performed on the patients under study due to lack of resources, and some patient data were communicated by telephone interview.
In conclusion, rhabdomyomas represent the most frequent benign cardiac tumors in fetal life; most cases have partial remission of the tumor. However, the clinical course depends on the location, size and its association with tuberous sclerosis. Therefore, a comprehensive and multidisciplinary study is recommended in the fetal stage and close follow-up in childhood.
REFERENCES
1. Allen H. Shaddy R. Penny D, Feltes T, Cetta F. Moss and Adams: Heart Disease in Infants, Children, and Adolescents. 9a edition. USA: Wolters Kluwer.2016. [citado 23 de mayo de 2021]; Disponible en: https://www.academia.edu/38449613/Moss_and_Adams_Heart_Disease_in_Infants_Children. [ Links ]
2. Yuan S-M. Fetal Primary Cardiac Tumors During Perinatal Period. Pediatr Neonatol. 2017;58(3):205-10. doi: 10.1016/j.pedneo.2016.07.004 [ Links ]
3. Holley D, Martin G, Brenner J, Fyfe D, Huhta J, Kleinman C, et al. Diagnosis and management of fetal cardiac tumors: a multicenter experience and review of published reports. J Am Coll Cardiol. 1995;26(2):516-20. doi: 10.1016/0735-1097(95)80031-b [ Links ]
4. Uzun O, Wilson D, Vujanic G, Parsons J, De Giovanni J. Cardiac tumours in children. Orphanet J Rare Dis. 2007;2(1):11. doi: 10.1186/1750-1172-2-11 [ Links ]
5. Kwiatkowska J, Waldoch A, Meyer-Szary J, Potaz P, Grzybiak M. Cardiac tumors in children: A 20-year review of clinical presentation, diagnostics and treatment. Adv Clin Exp Med. 2017;26(2):319-26. doi: 10.17219/acem/62121 [ Links ]
6. Fenoglio J, Mcallister H, Ferrans V. Cardiac rhabdomyoma: A clinicopathologic and electron microscopic study. Am J Cardiol. 1976;38(2):241-51. doi: 10.1016/0002-9149(76)90157-0 [ Links ]
7. Colosi E, Russo C, Macaluso G, Musone R, Catalano C. Sonographic diagnosis of fetal cardiac rhabdomyomas and cerebral tubers: a case report of prenatal Tuberous Sclerosis. J Prenat Med. 2013;7(4):51-5. [ Links ]
8. Chía-Vázquez N, Fuentes-Ramos G, Patiño-Bahena E, Guillén-González A, Buendía-Hernández A, Chía-Vázquez N, et al. Importancia del rabdomioma cardiaco en población pediátrica. Experiencia de 39 años. Serie de casos. Arch cardiol México. Marzo 2021;91(1):84-92. doi: 10.24875/acm.19000381 [ Links ]
9. Satge D, De Geeter B. Cardiac rhabdomyoma and apoptosis: are regression controlled by the body? Arch Mal Coeur Vaiss. 1992;85(5):603-8. [ Links ]
10. Alsabri M, Gonzalez A, Sircy A, Policherla SS, Mascoll-Robertson K. Congenital cardiac masses: a case report. J Med Case Rep. 2022 Apr 22;16(1):166. doi: 10.1186/s13256-022-03371-1 [ Links ]
11. Jaramillo J, Cruz V. Rabdomioma fetal: diagnóstico prenatal y tratamiento. Rev Colomb Cardiol. Sept./Oct. 2016;23(5):454- 454. doi:10.1016/j.rccar.2016.04.001 [ Links ]
12. Hinton R, Prakash A, Romp R, Krueger D, Knilans T. Cardiovascular Manifestations of Tuberous Sclerosis Complex and Summary of the Revised Diagnostic Criteria and Surveillance and Management Recommendations From the International Tuberous Sclerosis Consensus Group. J Am Heart Assoc. 2014;3(6):e001493. doi: 10.1161/jaha.114.001493 [ Links ]
13. Shapiro L. Cardiac tumours: diagnosis and management. Heart. 2001;85(2):218-22. doi: 10.1136/heart.85.2.218 [ Links ]
14. Józwiak S, Kotulska K, Kasprzyk-Obara J, Domanska-Pakiela D, Tomyn-Drabik M, Roberts P, et al. Clinical and Genotype Studies of Cardiac Tumors in 154 Patients with Tuberous Sclerosis Complex. Pediatrics. 2006;118(4):e1146-51. doi: 10.1542/peds.2006-0504 [ Links ]
15. Bravo-Oro A, Gómez-Elías C, Villegas-Valdez D, Reyes-Vaca J, Morales-Ibarra J, Rubio-Hernández M, et al. Everolimus response in a newborn with cardiac rhabdomyoma associated to tuberous sclerosis complex: Case report. Acta Pediatr Mex. 2020;41(5):208-14. doi: 10.18233/APM41No5pp208-2141962 [ Links ]
16. Dhulipudi B, Bhakru S, Rajan S, Doraiswamy V, Koneti N. Symptomatic improvement using everolimus in infants with cardiac rhabdomyoma. Ann Ped Cardiol. 2019;12(1):45. doi: 10.4103/apc.apc_79_18 [ Links ]
17. Chao A, Chao A, Wang T, Chang Y, Chang Y, Hsieh C, et al. Outcome of antenatally diagnosed cardiac rhabdomyoma: case series and a meta-analysis. Ultrasound Obstet Gynecol. 2008;31(3):289-95. doi: 10.1002/uog.5264 [ Links ]
18. Okmen F, Ekici H, Hortu I, Imamoglu M, Ucar B, Ergenoglu AM, Sagol S. Outcomes of antenatally diagnosed fetal cardiac tumors: a 10-year experience at a single tertiary referral center. J Matern Fetal Neonatal Med. 2022 Sep;35(18):3489- 94. doi: 10.1080/14767058.2020.1822316 [ Links ]
19. Desvars P, Genes L, Irala S, Mendieta E, Astigarraga N, Mir R. Complejo esclerosis tuberosa: reporte de un Caso Clínico neonatal. Pediatría. 2020.47(3),170-4. doi: 10.31698/ped.47032020009 [ Links ]
20. Amin S, Lux A, Calder N, Laugharne M, Osborne J, O'Callaghan F. Causes of mortality in individuals with tuberous sclerosis complex. Dev Med Child Neurol. 2017 Jun;59(6):612-7.doi:10.1111/dmcn.13352 [ Links ]
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article.
Ethical responsibilities: Protection of persons. The authors declare that the procedures followed conformed to the ethical standards of the committee on responsible human experimentation and in accordance with the World Medical Association and the Declaration of Helsinki.
Received: April 10, 2022; Accepted: February 05, 2023











 texto em
texto em