Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista Peruana de Ginecología y Obstetricia
versão On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.1 Lima jan./mar. 2023 Epub 27-Mar-2023
http://dx.doi.org/10.31403/rpgo.v69i2486
Caso Clínico
Preeclampsia and eclampsia complicated with retinal detachment. Report of three cases
1Physician specializing in Critical Obstetrics and Gynecology, Medical Chief of the Special Care Unit, Hospital Materno Infantil 1˚ de Mayo, Instituto Salvadoreño del Seguro Social, El Salvador.
2Third year resident physician of Gynecology and Obstetrics. Hospital Materno Infantil 1˚ de Mayo, Instituto Salvadoreño del Seguro Social, El Salvador.
3Medical specialist in Gynecology and Obstetrics. Hospital de la Caja de Seguro Social, Panama. Distinguished researcher of the National Research System, SENACYT Panama.
Preeclampsia is a multisystemic hypertensive disorder that occurs after 20 weeks of gestation in 5%-15% of pregnant women and is the cause of complications that can affect important organs and even cause death during gestation or in the postpartum period. It includes severe preeclampsia, eclampsia and HELLP (hemolysis, elevation of liver enzymes, low platelets) syndrome. We report three cases of retinal detachment that occurred in two patients with severe preeclampsia and one with eclampsia, all with hemorrhage and visual alteration in the postpartum period that required pharmacological treatment. Retinal detachment is a symptom associated with preeclampsia and eclampsia that can be investigated by ocular fundoscopy to determine whether conservative or pharmacological treatment is feasible.
Key words: Preeclampsia; Eclampsia; Retinal detachment; HELLP syndrome
INTRODUCCIÓN
Gestational-induced hypertension includes preeclampsia and eclampsia, occurs in approximately 5-15% of all pregnancies and may be associated with a wide variety of ocular abnormalities1).
Retinal detachment is an event secondary to choroidal ischemia resulting from retinal vasospasm as part of the multiorgan involvement of preeclampsia. Its clinical presentation is characteristic and relatively easy to diagnose. It is considered an unusual complication, although well documented in the literature, characterized by loss of visual acuity or temporary blindness that usually appears in the immediate postpartum period in patients with preeclampsia, eclampsia and HELLP syndrome1-3).
This communication presents the experience on the diagnosis and treatment of retinal detachment as an unusual complication in three cases attended at the Hospital Materno Infantil 1° de Mayo of the Instituto Salvadoreño del Seguro Social.
CASES REPORT
CASE 1
A 21-year-old primigravida at 34 weeks and 2 days of gestation with no relevant medical history convulsed at her residence and was taken to the hospital medical center where she presented a new convulsive event, postictal for 2 minutes, with recovery of consciousness. She was diagnosed as eclampsia due to blood pressure of 220/150 mmHg. A protocol of magnesium sulfate and intravenous hydralazine was started. Tests were taken for diagnostic certification and to rule out HELLP syndrome. The patient was stabilized and then cesarean section was performed without complications. In the special care unit, during her second day post cesarean section she reported blurred vision in her left eye. The ophthalmologist found visual acuity of the right eye 20/150, intraocular pressure 12 mmHg. In fundoscopy the cornea was clear, with wide chamber, clear crystalline lens, without Tyndall, dense cottony exudates with abundant vascular tortuosity. In the left eye, visual acuity was 20/700, intraocular pressure 12 mmHg. On fundoscopy, the cornea was clear, with wide chamber, clear crystalline lens, no Tyndall, with dense cottony exudates, marked vascular tortuosity. The conclusion was serous retinal detachment in the right eye and serous and bullous detachment in the left eye. The final diagnosis was serous and bullous retinal detachment secondary to hypertensive retinopathy. Bromfenac ophthalmic drops and strict blood pressure control were prescribed. In addition, two oral antihypertensives were administered (Figure 1).
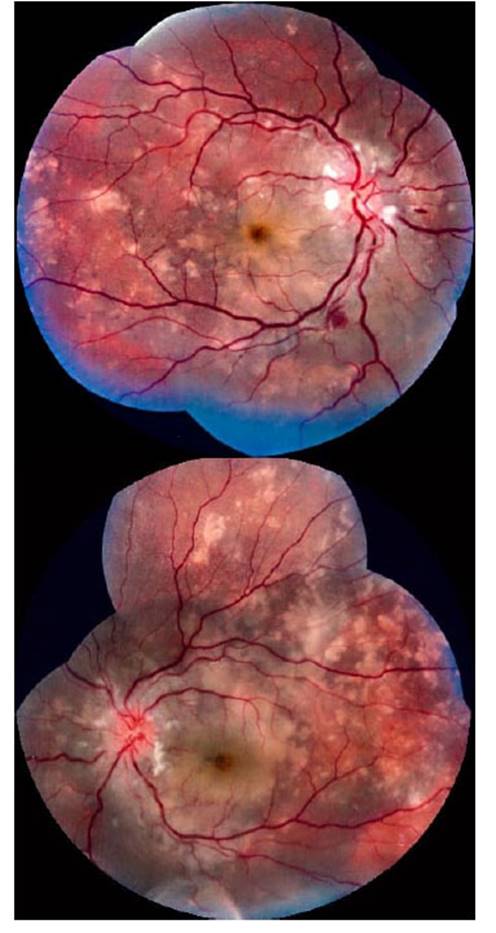
Figure 1 evaluation reported right eye visual acuity 20/150, intraocular pressure 12 mmhg. Fundoscopy: clear cornea, wide chamber, clear lens, no tyndall, dense cottony exudates with abundant vascular tortuosity. leFt eye with visual acuity 20/700, intraocular pressure 12 mmhg. Fundoscopy: clear cornea, wide chamber, clear lens, no tyndall, dense cottony exudates, marked vascular tortuosity. conclusion: serous retinal detachment in the right eye and serous and bullous detachment in the leFt eye. the Final diagnosis was serous and bullous retinal detachment secondary to hypertensive retinopathy.
CASE 2
A 30-year-old primigravida with 37 weeks of gestation and a history of A1 gestational diabetes consulted for severe headache. In the medical evaluation, severe preeclampsia was diagnosed with blood pressure of 167/115 mmHg and urine creatinine protein index of 0.6. Tests were requested for diagnostic certification and to rule out HELLP syndrome, and a protocol of magnesium sulfate and intravenous hydralazine was started. Labor was induced with prostaglandins. The delivery was vaginal and she presented hemorrhage due to episiotomy dissecting hematoma, which was drained and sutured. On her first postpartum day, the patient reported bilateral scotomas, without neurological alteration. The evaluation by the ophthalmologist determined in the right eye intraocular pressure of 15 mmHg, fundoscopy with clear cornea, wide chamber, clear crystalline lens, isochoric pupil reactive to light, flattened nasal retina, uncommitted macula. In the left eye, the cornea was clear, wide chamber, clear lens, isochoric pupil reactive to light, flattened nasal retina, uninvolved macula. The diagnosis was bilateral serous retinal detachment. Ophthalmic ketorolac drops were administered and blood pressure was strictly controlled. Two oral antihypertensives were added (Figure 2).

Figure 2 right eye evaluation reported intraocular pressure 15 mmhg. Fundoscopy: clear cornea, wide chamber, clear lens, isochoric pupil reactive to light, Flattened nasal retina, uninvolved macula. in the leFt eye: clear cornea, wide chamber, clear lens, isochoric pupil reactive to light, Flattened nasal retina, uninvolved macula. diagnosis: bilateral serous retinal detachment.
CASE 3
A 28-year-old secundigesta with term pregnancy delivered vaginally at a second level regional hospital, which was complicated by severe postpartum hemorrhage due to atony. Bleeding was estimated at 2,000 mL, which was resolved with uterotonic administration and without the use of ergot alkaloids (methylergonovine). In addition, severe postpartum preeclampsia was diagnosed due to blood pressure of 167/123 mmHg, and a protocol of magnesium sulfate and intravenous hydralazine was started. Tests were requested for diagnostic certification and to rule out HELLP syndrome. Hours later she reported decreased visual acuity and presence of scotomas, so an ocular ultrasound was performed, which showed echoes of membrane with insertion to the optic disc (posterior chamber). Bilateral retinal detachment was diagnosed and she was referred to a tertiary gynecology and obstetrics hospital, where an ophthalmologic evaluation by ocular fundoscopy was performed, which described normal anterior segment in both eyes, intraocular pressure of 10 mmHg in both eyes, bilateral changes in pigmentation and elevation at macular level, retinal folds at macula level, healthy optic nerve, deep border, flattened retina in both eyes, clear vitreous in both eyes. The diagnosis was exudative retinal detachment in both eyes secondary to preeclampsia, which was treated with conservative management, administration of oral antihypertensives and ambulatory control (Figure 3).

Figure 3 bilateral retinal detachment was diagnosed by ultrasound. ophthalmologic evaluation by ocular Fundoscopy described: normal anterior segment in both eyes, intraocular pressure 10 mmhg in both eyes, changes in pigmentation and elevation at macular level in both eyes, retinal Folds at macular level, healthy optic nerve, deep rim, Flattened retina in both eyes, clear vitreous in both eyes. diagnosis: exudative retinal detachment in both eyes secondary to preeclampsia.
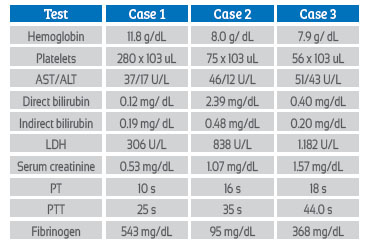
Although in two of the cases there were alterations in the laboratory tests suggesting the presence of HELLP syndrome, these alterations could have been associated with the formation of the episiotomy dissecting hematoma in case 2 and the severe postpartum hemorrhage in case 3, since no elevation of liver enzymes was observed (Table 1).
DISCUSSION
Pregnancy is associated with ocular changes in most patients very rarely permanent. These changes may be associated with the development of new conditions or exacerbated by preexisting comorbidities.
Ignorance of the symptoms associated with retinal detachment may lead to persistent or permanent blindness. Confusion between an alteration of neurological origin usually delays the confirmation of the ocular alteration. Usually the convulsive event (eclampsia) has been conditioned with cerebral involvement. The evaluation by brain tomography is frequently reported as normal, which makes it necessary to investigate the focal alteration in the eye. The clinician must know how to differentiate that the symptomatology orients to look for the origin of the lesion in the eye or in the brain, and if it is temporary or definitive1,4).
Pathologic conditions affecting the eye in pregnancy include preeclampsia, eclampsia, and central serous retinopathies. The most significant pre-existing condition that can aggravate ocular function is diabetes mellitus1).
The most common ocular symptoms in preeclampsia are blurred vision, photopsias, scotomas, and diplopia. The most frequently reported retinal abnormality in the ophthalmology literature in the context of preeclampsia is focal arteriolar spasm, associated with peripapillary or focal retinal edema. When the vessels return to normal after delivery, visual disturbance is unusual and, if present, other causes should be investigated1-5).
Severe retinal detachment secondary to choroidal ischemia is an unusual but well-documented cause of visual loss in preeclampsia, with residual pigment epithelial changes1,6).
Ten percent of patients with pregnancy-associated hypertension are complicated by HELLP syndrome characterized by hemolysis, elevated liver enzymes, and low platelets. Ocular findings associated with this syndrome include bilateral serous retinal detachment and vitreous hemorrhage1).
The incidence of visual and retinal abnormalities has decreased at present due to better management of pregnancy-induced hypertension. A high percentage of these abnormalities improve with antihypertensive pharmacologic management or delivery1).
In the past, most cases of retinal detachment were attributed to severe preeclampsia or eclampsia. Case reports of retinal detachment published in the past decade include information on the presence of HELLP syndrome as the most conditioning factor for retinal detachment3).
Thrombotic microangiopathy is associated as a cause of retinal hypoxia and retinal detachment in HELLP syndrome. However, cerebral hyperperfusion, and consequently ocular hyperperfusion, may be the cause of retinal detachment in the absence of vascular injury1-6).
Retinal detachment should be differentiated from posterior vitreous detachment (PVD). Both pathological entities share vision symptoms such as scotomas, blurred vision, and 'flashes'. Posterior vitreous detachment is characterized by the formation of fluid sacs that contract and decrease in volume. When the eye changes position, the gelatin moves within the vitreous cavity and this movement begins to separate it from the retina. Because the retina is a very thin and fragile structure, the separation of the vitreous exerts enough force to produce a tear or hole in it. This phenomenon is frequently observed in the elderly and should draw attention to a young patient presenting with these clinical features in the postpartum period, usually associated with excessive pushing during vaginal delivery or in the context of preeclampsia4).
Reversible posterior encephalopathy syndrome (PRES) can cause visual disturbances such as hemianopsia, blurred vision, amaurosis fugax and complete cortical blindness that can occur in up to 2/3 of patients with PRES. The confirmatory diagnosis of this entity is made by brain magnetic resonance imaging, observing areas of cortical vasogenic edema. Retinoscopy in these cases shows no alterations5,6). The visual alteration may persist in the absence of reversible posterior encephalopathy syndrome in the MRI. Unilateral visual disturbance could be an indicator of retinal and not cerebral cortical involvement, leading to an examination such as ocular fundoscopy. Computed tomography has not been shown to be a tool for evaluation of brain injury as the genesis of isolated visual impairment in pre-eclampsia-eclampsia7,8).
REFERENCES
1. Sheth BP, Mieler WF. Ocular complications of pregnancy. Curr Opin Ophthalmol. 2001;12(6):455-63. DOI: 10.1097/00055735-200112000-00011 [ Links ]
2. Dinn RB, Harris A, Marcus PS. Ocular changes in pregnancy. Obstet Gynecol Surv. 2003;58(2):137-44. doi: 10.1097/01. OGX.0000047741.79433.52 [ Links ]
3. Vigil-De Gracia P, Ortega-Paz L. Desprendimiento de retina en asociación con preeclampsia, eclampsia y síndrome HELLP. Int J Gynaecol Obstet. 2011;114:223-5. [ Links ]
4. Barnard D. Differential diagnosis of PVD and retinal detachment. Department of Optometry, SCHOOL OF Health Sciences Hadassah College, Jerusalem. Israel. December 2008;5:4-7. http://www.barnardlevit.co.uk/assets/Lectures/Differential-diagnosis-of-PVD-and-retinal-detachment-2008.pdf [ Links ]
5. Fischer M. Posterior reversible encephalopathy syndrome, J Neurol. 2017;264:1609-10. https://doi.org/10.1007/s00415-016-8377-8 [ Links ]
6. Sathish S. Bilateral choroidal ischaemia and serous retinal detachment in pre-eclampsia. Clin Exp Oftalmol. 2000;28(5):387-90. DOI: 10.1046/j.1442-9071.2000.00342.x [ Links ]
7. Androudi S. Study of serous retinal detachment in a preeclamptic patient. Semin Ophthalmol. 2007;22:189-91. DOI: 10.1080/08820530701501469 [ Links ]
8. Dahiya K. MRI Brain Lesions in Eclampsia: A Series of 50 Cases Admitted to HDU of a Tertiary Care Hospital. J Family Reprod Health. 2018;12(1):51-6. [ Links ]
Received: November 14, 2022; Accepted: December 19, 2022











 texto em
texto em