Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.1 Lima Jan./Mar. 2023 Epub Mar 27, 2023
http://dx.doi.org/10.31403/rpgo.v69i2487
Case report
Vasa previa with velamentous cord insertion: a case report
1. Medical Specialist in Gynecology and Obstetrics, Hospital Nacional Dos de Mayo (HNDM), Lima, Peru
2. Clínica Internacional, Lima, Peru
Vasa previa is a rare and infrequent prenatal finding of hemorrhage in the second half of pregnancy, in which umbilical vessels devoid of Wharton's jelly interpose between the fetal presentation and the internal cervical os. When undetected and rupture of the vessels occurs, it is associated with a high perinatal mortality rate. Three types are described; the case presented is type 1 vasa previa secondary to velamentous insertion of the cord. It was diagnosed prenatally by transvaginal ultrasound associated with color Doppler. A cesarean section was performed with favorable maternal and perinatal evolution.
Key words: Vasa previa; Umbilical cord; Prenatal diagnosis; Ultrasonography; prenatal; Doppler
Introduction
Vasa previa (VP) represents a rare entity of hemorrhage in the second half of pregnancy in which unprotected fetal vessels of Wharton's jelly or placental tissue flow across the amniotic membrane through the internal cervical os and ahead of the fetal presentation1. The estimated incidence is 0.46-0.6 in 1,000 pregnancies2,3.
Three variants of vasa previa have been identified: type 1, secondary to a velamentous insertion of the cord; type 2, associated with bilobed or succenturiata placenta; and type 3, where there are one or more boomerang-shaped vessels crossing the membranes along the placental margin4.
The risk factors associated with the entity are: placenta previa (OR: 19; 95% CI: 6.1-58), velamentous insertion (OR: 672; 95% CI: 112-4,034), assisted reproductive techniques such as in vitro fertilization and intracytoplasmic sperm injection (OR: 19; 95% CI: 6.6-54), morphological abnormalities of the placenta such as bilobed placenta and succenturiata (OR: 71; 95% CI: 14-349) and multiple gestation (OR: 2.66; 95% CI: 0.80-8.8)3. It should be noted that between 6%-14.3% of cases are detected VP in the absence of risk factors5.
The clinical course can be complicated by rupture of the vessels causing fetal hemorrhage or extrinsic compression of the cord causing heart rate decelerations, asphyxia, and fetal death6. When VP is not detected prenatally, fetal mortality ranges from 22.5%-100%7, but if the diagnosis is made prenatally, the neonatal mortality rate is <1%; one third of patients will require an unscheduled delivery8.
Most international guidelines performing routine prenatal ultrasound recommend an ultrasound evaluation of the umbilical vessels and cord insertion9. However, universal ultrasound screening for VP is not recommended unless prenatal risk factors are present10.
We present a case of prenatal diagnosis of vasa previa secondary to velamentous insertion.
Case report
A 38-year-old female patient, G3P1011, 29 weeks 4 days by first trimester ultrasound, with previous vaginal delivery and medical abortion, without pathological or surgical history of interest and who had 5 prenatal controls in a health center, presented with emergency uterine contractions and little bleeding from the vaginal canal. On physical examination she was hemodynamically stable, with a soft, depressible abdomen occupied by a pregnant uterus of normal tone. The vaginal canal showed scanty dark red bleeding. Fetal monitoring was performed and showed two rhythmic uterine contractions in 10 minutes.
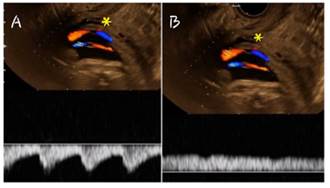
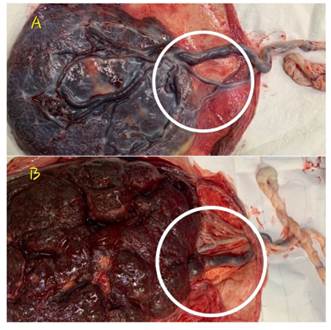
Obstetric ultrasound showed a single fetus in breech presentation without morphological alterations, with a heart rate of 142 beats per minute, fetal weight estimated at 1,494 g at the 62nd percentile for gestational age, normal amniotic fluid volume, low insertion posterior body placenta and, in front of the fetal presentation, vessels passing over the cervix were observed (Figure 1). Transvaginal ultrasound revealed cervical length of 35 mm, and color Doppler showed vessels devoid of umbilical cord running longitudinally above the internal cervical os (Figure 2). Pulsed Doppler exhibited an arterial vessel and another fetal venous vessel (Figure 3), which led to the diagnosis of vasa previa with velamentous insertion. She was hospitalized for tocolysis and pulmonary maturation. Five days later she was discharged without uterine contractions or intercurrences. Weekly outpatient follow-up was indicated. The patient attended only two check-ups.
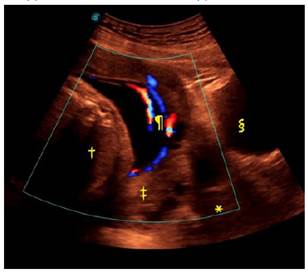
Figure 1 Abdominal ultrasound: Vessels (¶) from the placenta (‡) passing over the cervix (*) are seen in front of the fetal presentation (†). The maternal bladder is visualized (§).
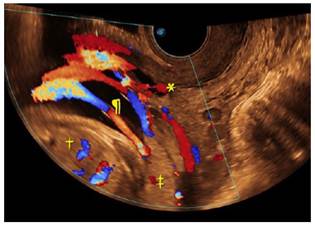
Figure 2 Transvaginal ultrasound: In front of the fetal presentation (†), color Doppler shows fetal vessels (¶) running longitudinally above the internal cervical os (*). Placenta (‡).
At 35 weeks and 5 days of gestation, the patient presented in emergency for regular uterine contractions and scant vaginal bleeding. A cesarean section was performed without complications, in which a live male newborn was obtained, 2,512 grams, 37 weeks by Capurro, adequate for gestational age and Apgar 7 at 1 minute and 9 at 5 minutes. Macroscopic examination of the placenta (Figure 4) confirmed the ultrasound findings of vasa previa secondary to velamentous insertion. In-hospital maternal and neonatal evolution was favorable, and the mother and newborn were discharged after 48 hours.
Discussion
The umbilical cord normally inserts into the center of the placenta. However, two main types of abnormal insertion have been identified, both of which have clinical significance during labor11. One is marginal insertion when the cord inserts at the periphery of the placental mass, which is supported by very little placental tissue; and the second is velamentous insertion (VI), when the cord attaches only to the amniotic membranes rather than to the placental mass, leaving the umbilical vessels unprotected by Wharton's jelly12. These vessels are prone to compression and rupture, especially in labor. In the VI, when the vessels pass through the internal cervical os and in front of the fetal presentation or are within 2 cm of the internal cervical os they constitute the type 1 variant of vasa previa (VP1)5,13.
The VP1 entity represents a rare entity, estimating that 1-50 cases of VI is complicated with VP and is associated with high perinatal mortality rates, particularly when it is not suspected during the prenatal stage1,11. VI has an incidence of 0.4-11% in singleton pregnancies and increases in twin pregnancies (1.6-40%). In addition, it has adverse pregnancy outcomes, such as small-for-gestational-age newborns, preterm delivery, perinatal death, intrauterine fetal death, and intrapartum complications, including emergency cesarean delivery12,14.
Most routine prenatal ultrasound protocols include an ultrasound evaluation of the umbilical vessels and cord insertion into the fetal abdomen15. However, routine ultrasound often fails to detect VI and universal ultrasound screening is not recommended but may be performed in cases where prenatal risk factors are present5. Prenatal VI identification is a desirable clinical goal, as these pregnancies have an increased risk of adverse perinatal outcomes and, despite the obvious importance of prenatal VI detection in obstetric practice, only a few studies have focused on the systematic identification of the site of placental cord insertion during prenatal ultrasonography16.
Prenatal diagnosis of VP is most often made by ultrasound between 18-26 weeks of gestation. On the gray scale, parallel or circular echogenic lines are observed near the internal cervical os; and if associated with color Doppler, pulsed Doppler fetal vessels show an arterial or venous waveform. The accuracy of ultrasound when performed transvaginally combined with color Doppler is 93%, with specificity between 99%-100%1,17. Prenatal diagnosis is associated with 97%-99% perinatal survival, while the absence of diagnosis increases the risk of hypoxic morbidity 50-fold and the risk of perinatal death 25-fold18.
Because the vessels are attached to the chorion, rupture of the membranes may result in rupture of the vessels with fetal hemorrhage. Or extrinsic compression of the cord may occur leading to fetal heart rate decelerations which, if prolonged, may lead to fetal asphyxia and subsequent death10.
For this reason, the goal of management will be to prolong pregnancy in a safe manner, avoiding possible complications related to rupture of membranes or delivery, as well as minimizing the impact of prematurity19. Although it is difficult to establish the optimal gestational age for delivery, in cases of uncomplicated VP, elective cesarean section is recommended at around 36 weeks gestation, when a low rate of perinatal mortality and morbidity is observed20.
REFERENCES
1. Melcer Y, Maymon R, Jauniaux E. Vasa previa: prenatal diagnosis and management. Curr Opin Obstet Gynecol. 2018;30(6):385-91. doi:10.1097/GCO.0000000000000478 [ Links ]
2. Pavalagantharajah S, Villani LA, D'Souza R. Vasa previa and associated risk factors: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2020;2(3):100117. doi:10.1016/j.ajogmf.2020.100117 [ Links ]
3. Ruiter L, Kok N, Limpens J, Derks JB, de Graaf IM, Mol B, Pajkrt E. Incidence of and risk indicators for vasa praevia: a systematic review. BJOG Int J Obstet Gynaecol. 2016;123(8):1278-87. doi:10.1111/1471-0528.13829 [ Links ]
4. Ranzini AC, Oyelese Y. How to screen for vasa previa. Ultrasound Obstet Gynecol. 2021;57(5):720-5. doi:10.1002/uog.23520 [ Links ]
5. Oyelese Y. Vasa previa: time to make a difference. Am J Obstet Gynecol. 2019;221(6):539-41. doi:10.1016/j.ajog.2019.08.034 [ Links ]
6. Sullivan EA, Javid N, Duncombe G, Li Z, Safi N, Cincotta R, et al. Vasa Previa Diagnosis, Clinical Practice, and Outcomes in Australia. Obstet Gynecol. 2017;130(3):591-8. doi:10.1097/AOG.0000000000002198 [ Links ]
7. Bonilla-Sepúlveda ÓA. Vasa previa, presentación de un caso en un centro de referencia en Envigado, Colombia, y revisión de la literatura. Rev Colomb Obstet Ginecol. 2014;65(1):85-91. doi:10.18597/rcog.82 [ Links ]
8. Westcott JM, Simpson S, Chasen S, Vieira L, Stone J, Doulaveris G, et al. Prenatally diagnosed vasa previa: association with adverse obstetrical and neonatal outcomes. Am J Obstet Gynecol MFM. 2020;2(4):100206. doi:10.1016/j.ajogmf.2020.100206 [ Links ]
9. Bohîltea RE, Dima V, Ducu I, Iordache AM, Mihai BM, Munteanu O, t al. Clinically Relevant Prenatal Ultrasound Diagnosis of Umbilical Cord Pathology. Diagnostics. 2022;12(2):236. doi:10.3390/diagnostics12020236 [ Links ]
10. Tsakiridis I, Mamopoulos A, Athanasiadis A, Dagklis T. Diagnosis and Management of Vasa Previa: A Comparison of 4 National Guidelines. Obstet Gynecol Surv. 2019;74(7):436-42. doi:10.1097/OGX.0000000000000692 [ Links ]
11. Aguirregoikoa JA, Burgos J, Moreno J, Albisua M, Urquijo E, Larrieta R. Inserción velamentosa de cordón umbilical. Rotura intraparto. Clínica E Investig En Ginecol Obstet. 2006;33(1):38-40. doi:10.1016/S0210-573X(06)74080-1 [ Links ]
12. Buchanan-Hughes A, Bobrowska A, Visintin C, Attilakos G, Marshall J. Velamentous cord insertion: results from a rapid review of incidence, risk factors, adverse outcomes and screening. Syst Rev. 2020;9(1):147. doi:10.1186/s13643-020-01355-0 [ Links ]
13. Rebarber A, Dolin C, Fox NS, Klauser CK, Saltzman DH, Roman AS. Natural History of Vasa Previa Across Gestation Using a Screening Protocol. J Ultrasound Med. 2014;33(1):141-7. doi:10.7863/ultra.33.1.141 [ Links ]
14. Ismail KI, Hannigan A, O'Donoghue K, Cotter A. Abnormal placental cord insertion and adverse pregnancy outcomes: a systematic review and meta-analysis. Syst Rev. 2017;6(1):242. doi:10.1186/s13643-017-0641-1 [ Links ]
15. Kelley BP, Klochko CL, Atkinson S, Hillman D, Craig BM, Sandberg SA, Gaba AR, Halabi SS. Sonographic Diagnosis of Velamentous and Marginal Placental Cord Insertion. Ultrasound Q. 2020;36(3):247-54. doi:10.1097/RUQ.0000000000000437 [ Links ]
16. Sepulveda W, Rojas I, Robert JA, Schnapp C, Alcalde JL. Prenatal detection of velamentous insertion of the umbilical cord: a prospective color Doppler ultrasound study. Ultrasound Obstet Gynecol. 2003;21(6):564-9. doi:10.1002/uog.132 [ Links ]
17. Ruiter L, Kok N, Limpens J, Derks JB, de Graaf IM, Mol BWJ, Pajkrt E. Systematic review of accuracy of ultrasound in the diagnosis of vasa previa. Ultrasound Obstet Gynecol. 2015;45(5):516-22. doi:10.1002/uog.14752 [ Links ]
18. Zhang W, Geris S, Al-Emara N, Ramadan G, Sotiriadis A, Akolekar R. Perinatal outcome of pregnancies with prenatal diagnosis of vasa previa: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2021;57(5):710-9. doi:10.1002/uog.22166 [ Links ]
19. Sinkey RG, Odibo AO, Dashe JS. #37: Diagnosis and management of vasa previa. Am J Obstet Gynecol. 2015;213(5):615-9. doi:10.1016/j.ajog.2015.08.031 [ Links ]
20. Mitchell SJ, Ngo G, Maurel KA, Hasegawa J, Arakaki T, Melcer Y, et al. Timing of birth and adverse pregnancy outcomes in cases of prenatally diagnosed vasa previa: a systematic review and meta-analysis. Am J Obstet Gynecol. 2022;227(2):173-81.e24. doi:10.1016/j.ajog.2022.03.006 [ Links ]
Received: October 20, 2022; Accepted: December 13, 2022











 text in
text in