Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.2 Lima Apr./Jun. 2023 Epub July 06, 2023
http://dx.doi.org/10.31403/rpgo.v69i2510
Original paper
Pregestational obesity and birth alterations
1 Medical specialist in Gynecology and Obstetrics. Assistant to the Obstetrics and Gynecology Service, Hospital Central "Dr. Urquinaona", Maracaibo, Venezuela.
2 Doctor in Medical Sciences. Assistant of the Obstetrics and Gynecology Service, Hospital Central "Dr. Urquinaona", Maracaibo, Venezuela.
3 Doctor in Clinical Medicine, School of Medicine , University of Zulia, Maracaibo, Venezuela.
3 Doctor in Clinical Medicine, School of Medicine , University of Zulia, Maracaibo, Venezuela.
3 Doctor in Clinical Medicine, School of Medicine , University of Zulia, Maracaibo, Venezuela.
6 Obstetrics and Gynecology Physician. Sanitas Medical Center, Coral Springs , Florida, EE. UU.
7 Doctor in Medical Sciences. Assistant of the Obstetrics and Gynecology Service, Hospital Central "Dr. Urquinaona", Maracaibo, Venezuela.
Objective
: To establish the association between pregestational obesity and the risk of birth alterations. Design: Retrospective cohort study. Institution: Hospital Central "Dr. Urquinaona", Maracaibo, Venezuela.
Methods
: Obstetric outcome of patients according to pregestational mass index -obese (group A), overweight (group B), and normal weight (group C)- attended between January and December 2021. Main study measures: Duration of pregnancy and duration, type and alterations of delivery.
Results
: A total of 2,250 deliveries were attended during the study period, of which 226 pregnant women were selected for analysis. The majority of the pregnant women (60.5%) were assigned to group A, 47 (20.8%) to group B, and 41 (17.5%) to group C. Pregnant women in group A had a higher probability of cesarean section (odds ratio (OR) 1.76; 95% confidence interval (95%CI), 1.03 - 2.98), prolonged labor (OR 2.09; 95%CI, 1.23 - 3.53) and prolonged pregnancy (OR 2.30; 95%CI, 1.32 - 4.01) compared to pregnant women in group C. The pregnant women in group B did not show statistically significant differences in the frequency of obstetric variables compared to the pregnant women in group C (p = ns).
Conclusion
: There was a significant association between pregestational obesity and the risk of birth alterations.
Keywords: Body mass index; Maternal obesity; Obstetric labor complications
INTRODUCCIÓN
Obesity is one of the most common conditions in the general population. Human energy balance is regulated by genetic factors and the precise genetic mechanisms are still unknown. However, it is often considered a condition secondary to patients' eating habits, preventable with self-control and discipline1).
Being underweight or obese can cause potential problems during pregnancy. Different studies have analyzed the potential effects of overweight and obesity on pregnancy and its outcome1). Overweight and obese subjects are at increased risk of developing diabetes, hypertension, dyslipidemia, cardiovascular and cerebrovascular disease, gout, sleep apnea, osteoarthritis, menstrual irregularities, and some cancers2). Pregestational obesity is associated with obstetric complications such as gestational diabetes, macrosomia, shoulder dystocia, and operative risks including anesthetic complications and surgical wound dehiscence and infection3). It may also be associated with increased risk of cesarean section4-6). Both pregestational and gestational weight gain is associated with increased frequency of fetal macrosomia, labor and fetal heart rate abnormalities, prolonged pregnancy, meconium staining of amniotic fluid and cesarean section5).
The aim of this study was to establish the association between pregestational obesity and delivery abnormalities.
METHODS
The data for this study were obtained from the medical records of pregnant women attended at the Hospital Central "Dr. Urquinaona", Maracaibo, Venezuela, between January and December 2021. Women with singleton pregnancies at term and without medical or obstetric complications such as diabetes, hypertension, preeclampsia, placenta previa and/or previous cesarean section were included.
Pregestational weight and height of the pregnant women were obtained and verified from medical history data. The formula used to calculate the body mass index (BMI) was weight in kilograms divided by height in meters squared7,8). The patients were classified according to pregestational BMI as obese (BMI greater than 30 kg/m2; group A) and overweight (BMI between 25-30 kg/m2; group B) and were compared with normal weight pregnant women (BMI between 20-25 kg/m2; group C). The variables evaluated were type of delivery, duration of labor, frequency of prolonged pregnancies and fetal macrosomia. Detailed information on delivery complications and neonatal outcome was obtained by reviewing medical records.
Data were analyzed using SPSS® statistical software, version 22.0. Data analysis also included logistic regression, t-test for independent samples, and chi-square test. Regression analysis was performed to control for potential confounding variables. The odds ratio (OR) with 95% confidence interval (95%CI) was used to establish the risk in the study variables on obstetric and perinatal outcomes. A value of p < 0.05 was considered statistically significant.
RESULTS
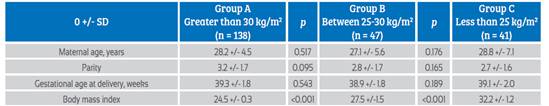
A total of 206 pregnant women with an average age of 27.8 +/7.1 years, parity of 3.2 +/1.8 deliveries and gestational age at delivery of 39.1 +/1.8 weeks were selected for the study. Of this group of patients, 138 pregnant women (61.1%) were assigned to group A, 47 women (20.8%) to group B and 41 (18.1%) to group C. The characteristics of each group are shown in Table 1. No significant differences were found in maternal age, parity, and gestational age at delivery between the groups. Body mass index was significantly higher in groups B and C compared to group A (p < 0.001).
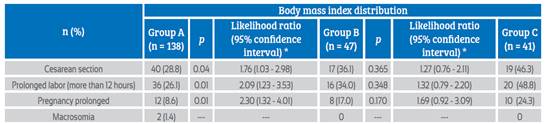
Table 2 shows the obstetric outcome in each of the study groups. Pregnant women in group A had a higher probability of cesarean section (PR 1.76; 95%CI, 1.0-2.98), prolonged labor (PR 2.09; 95%CI, 1.23-3.53) and prolonged pregnancy (PR 2.30; 95%CI, 1.32-4.01) compared to pregnant women in group C (p < 0.05). Pregnant women in group B did not show statistically significant differences in the probability of obstetric and perinatal outcomes compared to pregnant women in group A (p = ns). When adjusting for confounding variables (age and parity), no significant changes were found in the odds ratio in each of the analyses. Only two cases of fetal macrosomia were found, which corresponded to group A.
DISCUSSION
Factors such as pregestational obesity, weight gain during pregnancy, maternal age, increased parity, and history of cesarean section are associated with increase of dystocic deliveries6). This study analyzed the potential association between pregestational body mass index and obstetric and perinatal outcomes, demonstrating that the risk of cesarean section and prolonged labor (> 12 hours) were higher in obese patients. Although initially the differences between obese and non-obese pregestational pregnant women were significant, after controlling for confounding variables, these differences remained significant. The possible explanation for this finding is that both obstetric complications may be associated with increased soft tissue volume in both the perineum and maternal pelvis7,8). On the other hand, an investigation that analyzed different maternal anthropometry data confirmed the value of pregestational maternal weight, height and body mass index as a predictor of maternal and perinatal outcome9).
Perinatal complications, such as prematurity, low birth weight and death, are generally associated with pregestational low weight, low weight gain, adolescent pregnancy, nulliparity and smoking10,11). The consequences of pre-pregnancy BMI variations can vary widely among different population groups. As one of the markers of nutritional status, low BMI may reflect chronic nutritional deficiencies and/or acute lack of food intake. On the other hand, high values may reflect the degree of adiposity resulting from the imbalance between food intake and energy expenditure from physical activity3).
In the present investigation, the frequency of prolonged pregnancy was significantly higher in obese pregnant women before gestation (25%) compared with non-obese pregnant women (10%). Previous studies have shown a strong association between obesity and prolonged pregnancy, cesarean section and macrosomia5). However, among our data, only 2 newborns with a diagnosis of macrosomia were found, both in non-obese pregnant women.
Most previous studies have shown increased risk of chronic hypertension, preeclampsia and gestational diabetes in pregnant women with excess weight and/or excessive weight gain before and during pregnancy. There is evidence that newborns of obese women are larger for their gestational age and cesarean section rates are higher. Higher birth weight is associated with increased risk of shoulder dystocia, trauma and perinatal asphyxia. There is also an increased risk of postpartum hemorrhage, puerperal infection and deep vein thrombosis. In addition, surgical morbidity and mortality increases and there are more post-anesthetic complications5).
There are numerous obstetric morbidities and complications associated with pregestational obesity12-14), for example, the risk of cesarean section (5 times higher), occurrence and development of hypertension (9 times higher), preeclampsia (12 times higher) and gestational diabetes (24 times higher) in patients with different degrees of obesity compared to patients with normal weight15). These data are supported by different analyses showing marked increases in the risks of these and other conditions such as thromboembolism, chorioamnionitis, wound infection and need for intensive care16).
Pregestational obesity is not a contraindication to pregnancy, but prenatal care and education by expert dietitian-nutritionists is essential to achieve a complication-free pregnancy. Obese women should receive preconception counseling on lifestyle and behavioral modifications to achieve ideal body weight before pregnancy.
During pregnancy, it is necessary to follow a proper diet and lead an active life. Therefore, decreasing obesity before and during pregnancy should lead to decreased rate of birth disturbances and reduced surgical morbidity12).
The association of pregestational obesity with birth complications is supported by other studies. Evidence indicates that primary and secondary obesity prevention measures prior to pregnancy can improve perinatal outcome17-19). The increased risk of complications in obese pregnant women provides evidence for the need to reverse current nutrition trends. The prevalence of obesity continues to increase in all countries, especially in developing countries. This is despite attempts to prevent it. Most efforts have focused on individual women or small groups, which has proven to be ineffective, as women of childbearing age are increasingly surrounded by stimuli that lead to higher caloric intake20).
There is evidence that the risks of cesarean section are greater and more complex in obese pregnant women. Apart from having a higher probability of indication for abdominal termination of pregnancy, they also have a higher risk of postoperative complications associated with obesity (e.g., preeclampsia)21-23). Although cesarean section is a good indicator of the possible effects of obesity on birth alterations, the information it can provide should be carefully analyzed, as it can be affected by multiple factors. In this research we tried to limit the knowledge provided by this indicator to only those patients who had an indication associated with pregestational obesity, in order to avoid confusion. The results of this research suggest the role of obesity in increasing the cesarean section rate, a finding that may help practitioners optimize the care of pregnant women with pregestational obesity24,25).
The disturbing increases in risks and probabilities suggest that the situation may become even more worrisome as the prevalence of obesity continues to increase13). The prevalence of pregestational and gestational diabetes is increasing. In addition, many women are delaying pregnancy and the rate of multiple pregnancies is increasing as a result of the widespread use of in vitro fertilization procedures. Each of these factors interacts with maternal obesity, leading to high-risk pregnancies. Prevention of excessive weight gain in adolescents and young women would be the most effective intervention possible. However, strategies to achieve this are necessary, as the economic benefits of reducing the complications of obesity during and outside of pregnancy would be substantial.
REFERENCES
1. Kalliala I, Markozannes G, Gunter MJ, Paraskevaidis E, Gabra H, Mitra A, et al. Obesity and gynaecological and obstetric conditions: umbrella review of the literature. BMJ. 2017;359:j4511. doi: 10.1136/bmj.j4511 [ Links ]
2. Lin LH, Lin J, Yan JY. Interactive affection of pre-pregnancy overweight or obesity, excessive gestational weight gain and glucose tolerance test characteristics on adverse pregnancy outcomes among women with gestational diabetes mellitus. Front Endocrinol (Lausanne). 2022;13:942271. doi: 10.3389/fendo.2022.942271 [ Links ]
3. Girardi G, Bremer AA. The intersection of maternal metabolic syndrome, adverse pregnancy outcomes, and future metabolic health for the mother and offspring. Metab Syndr Relat Disord. 2022;20(5):251-4. doi: 10.1089/met.2021.0124 [ Links ]
4. Olerich K, Soper D, Delaney S, Sterrett M. Pregnancy care for patients with super morbid obesity. Front Pediatr. 2022;10:839377. doi: 10.3389/fped.2022.839377 [ Links ]
5. Ounjaijean S, Wongthanee A, Kulprachakarn K, Rerkasem A, Pruenglampoo S, Mangklabruks A, et al. Higher maternal BMI early in pregnancy is associated with overweight and obesity in young adult offspring in Thailand. BMC Public Health. 2021;21(1):724. doi: 10.1186/s12889-021-10678-z [ Links ]
6. Timmermans YEG, van de Kant KDG, Oosterman EO, Spaanderman MEA, Villamor-Martinez E, Kleijnen J, et al. The impact of interpregnancy weight change on perinatal outcomes in women and their children: A systematic review and meta-analysis. Obes Rev. 2020;21(3):e12974. doi: 10.1111/obr.12974 [ Links ]
7. Kominiarek MA, Cordero C, Stuebe AM, Simon M, Evenson KR, Perreira KM, et al. Pre-pregnancy health behaviors and gestational weight gain among hispanic/latino women: hispanic community health study/study of latinos. Matern Child Health J. 2021;25(12):2002-13. doi: 10.1007/s10995021-03252-x [ Links ]
8. Zaçe D, LA Gatta E, Orfino A, Viteritti AM, DI Pietro ML. Knowledge, attitudes, and health status of childbearing age young women regarding preconception health an Italian survey. J Prev Med Hyg. 2022;63(2):E270-E281. doi: 10.15167/2421-4248/jpmh2022.63.2.2571 [ Links ]
9. Bauserman MS, Bann CM, Hambidge KM, Garces AL, Figueroa L, Westcott JL, et al. Gestational weight gain in 4 lowand middle-income countries and associations with birth outcomes: a secondary analysis of the Women First Trial. Am J Clin Nutr. 2021;114(2):804-12. doi: 10.1093/ajcn/nqab086 [ Links ]
10. Li K, Yang C, Fan J, Li X, Gu C, Liu H. Prepregnancy body mass index, gestational weight gain, and maternal prepartum inflammation in normal pregnancies: findings from a Chinese cohort. BMC Pregnancy Childbirth. 2022;22(1):531. doi: 10.1186/s12884-022-04849-y [ Links ]
11. Frey HA, Ashmead R, Farmer A, Kim YH, Shellhaas C, Oza-Frank R, et al. Association of prepregnancy body mass index with risk of severe maternal morbidity and mortality among Medicaid beneficiaries. JAMA Netw Open. 2022;5(6):e2218986. doi: 10.1001/jamanetworkopen.2022.18986 [ Links ]
12. Lutsiv O, McKinney B, Foster G, Taylor VH, Pullenayegum E, McDonald SD. Pregnancy complications associated with the co-prevalence of excess maternal weight and depression. Int J Obes (Lond). 2015;39(12):1710-6. doi: 10.1038/ijo.2015.119 [ Links ]
13. Rubens M, Ramamoorthy V, Saxena A, McGranaghan P, Veledar E, Hernandez A. Obstetric outcomes during delivery hospitalizations among obese pregnant women in the United States. Sci Rep. 2022;12(1):6862. doi: 10.1038/s41598022-10786-9 [ Links ]
14. Rahman M, Rahman SM, Pervin J, Aktar S, El Arifeen S, Rahman A. Body mass index in early-pregnancy and selected maternal health outcomes: Findings from two cohorts in Bangladesh. J Glob Health. 2020;10(2):020419. doi: 10.7189/jogh.10.020419 [ Links ]
15. Edelson PK, Bastek JA, Levine LD. Evaluating the obstetrical implications of antenatal testing for women with morbid obesity: Maternal and fetal outcomes of increased surveillance. Am J Perinatol. 2016;33(9):839-43. doi: 10.1055/s0036-1572541 [ Links ]
16. Bogdanet D, Mustafa M, Khattak A, Shea PMO, Dunne FP. Atlantic DIP: is weight gain less than that recommended by IOM safe in obese women with gestational diabetes mellitus? Int J Obes (Lond). 2021;45(5):1044-1051. doi: 10.1038/s41366-021-00769-7 [ Links ]
17. Sunder A, Varghese B, Darwish B, Shaikho NM, AlSada A, Albuainain H, et al. Maternal obesity: An obstetric risk. Cureus. 2022;14(9):e29345. doi: 10.7759/cureus.29345 [ Links ]
18. Frey HA, Ashmead R, Farmer A, Kim YH, Shellhaas C, Oza-Frank R, et al. Association of prepregnancy body mass index with risk of severe maternal morbidity and mortality among Medicaid beneficiaries. JAMA Netw Open. 2022;5(6):e2218986. doi: 10.1001/jamanetworkopen.2022.18986 [ Links ]
19. Eshetu B, Balis B, Daba W, Mekonnen B, Getachew T, Roga EY, et al. Magnitude of cesarean-section and associated factors among diabetic mothers in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia: A cross-sectional study. Front Public Health. 2022;10:888935. doi: 10.3389/fpubh.2022.888935 [ Links ]
20. Lu X, Jin Y, Li D, Zhang J, Han J, Li Y. Multidisciplinary progress in obesity research. Genes (Basel). 2022;13(10):1772. doi: 10.3390/genes13101772 [ Links ]
21. Chandrasekaran S, Neal-Perry G. Long-term consequences of obesity on female fertility and the health of the offspring. Curr Opin Obstet Gynecol. 2017;29(3):180-187. doi: 10.1097/GCO.0000000000000364 [ Links ]
22. Nagpal TS, Souza SCS, Moffat M, Hayes L, Nuyts T, Liu RH, et al. Does prepregnancy weight change have an effect on subsequent pregnancy health outcomes? A systematic review and meta-analysis. Obes Rev. 2022;23(1):e13324. doi: 10.1111/obr.13324 [ Links ]
23. Denizli M, Capitano ML, Kua KL. Maternal obesity and the impact of associated early-life inflammation on longterm health of offspring. Front Cell Infect Microbiol. 2022;12:940937. doi: 10.3389/fcimb.2022.940937 [ Links ]
24. Creanga AA. Maternal obesity and severe maternal morbidity-It is time to ask new research questions. Paediatr Perinat Epidemiol. 2019;33(1):17-18. doi: 10.1111/ppe.12533 [ Links ]
25. Senbanjo OC, Akinlusi FM, Ottun TA. Early pregnancy body mass index, gestational weight gain and perinatal outcome in an obstetric population in Lagos, Nigeria. Pan Afr Med J. 2021;39:136. doi: 10.11604/pamj.2021.39.136.25926 [ Links ]
Statement of ethical issues
Ethical responsibilities: Protection of persons. The authors declare that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Confidentiality of data: The authors declare that they have followed the protocols of the Central Hospital "Dr. Urquinaona" and the University of Zulia on the publication of patient data.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Funding: The authors certify that they have not received financial support, equipment, in working personnel or in kind from individuals, public and/or private institutions for conducting the study.
Received: August 25, 2022; Accepted: January 20, 2023











 text in
text in