Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.2 Lima Apr./Jun. 2023 Epub July 06, 2023
http://dx.doi.org/10.31403/rpgo.v69i2520
Case report
Management of vulvar Behçet's disease: case report.
1Universidad Libre, Cali, Colombia
Behçet's disease (BD) is an inflammatory, multisystemic, relapsing-remitting disorder of unknown etiology. A key feature of the disease is orogenital ulceration that causes considerable morbidity with great impact on patient’s quality of life. Its medical management consists of a scheme with colchicine, steroids or immunomodulators. We report the case of a patient with genital lesions who consulted on multiple occasions, receiving antibiotics and even surgical management, with refractory response to these interventions. Subsequently, due to the characteristics of the lesion and clinical behavior, Behçet's disease was suspected and medical management with oral steroids and cures with phytostimulin was initiated. The genital ulcers were resolved, and the patient was subsequently taken to surgery for correction of the vulvar synechiae.
Key words: Vulvar diseases; Behçet syndrome; Systemic vasculitis
INTRODUCTION
Behçet's disease (BD) is a chronic, multisystemic, inflammatory disorder of peri-vasculitis, first described by the Turkish dermatologist Hulusi Behçet in 1937. It is characterized by recurrent mucocutaneous lesions. Other clinical manifestations include ocular inflammation, rheumatologic involvement, vascular and central nervous system complications. The etiology and pathogenesis are not fully elucidated. Symptoms are considered to be based on the correlation of intrinsic (genetic) and extrinsic (microbial and/or environmental) factors, as well as hormonal and immune system dysregulation1).
The onset of BD usually occurs between the third or fourth decade of life with an almost equal proportion between men and women, although men tend to have more severe symptoms2). The prevalence is higher in Middle Eastern countries such as Turkey where it occurs in approximately 370/100,000 inhabitants and in Iran with a prevalence of 80/100,000; it is also found in Central Asian and Far Eastern countries3). In Colombia, a prevalence of 0.001% was estimated in people over 18 years of age, and in the United States it is estimated to be between 0.3-6.6/100,000 inhabitants4). This epidemiological behavior is related to the existence of a genetic predisposition that facilitates the presentation and diagnosis of BD5).
The therapeutic spectrum is broad, ranging from colchicine monotherapy for the most limited forms (cutaneomucosal or articular) to corticosteroids; immunosuppressive treatments and biotherapies are used for the most severe or refractory forms. The intensity of the treatment is graded according to the type of manifestation, the desired speed of efficacy and the threat to the functional or vital prognosis6,7). Regarding surgical management as a treatment for skin lesions, there is insufficient evidence in the literature. A diagnostic test is the positive patergia test, which consists of a hypersensitivity reaction of the skin tissues to trauma, so that any surgical procedure may favor the exacerbation of the lesions and, particularly in the case of the genital area, there is a greater risk of superinfection or synechiae8).
CASE REPORT
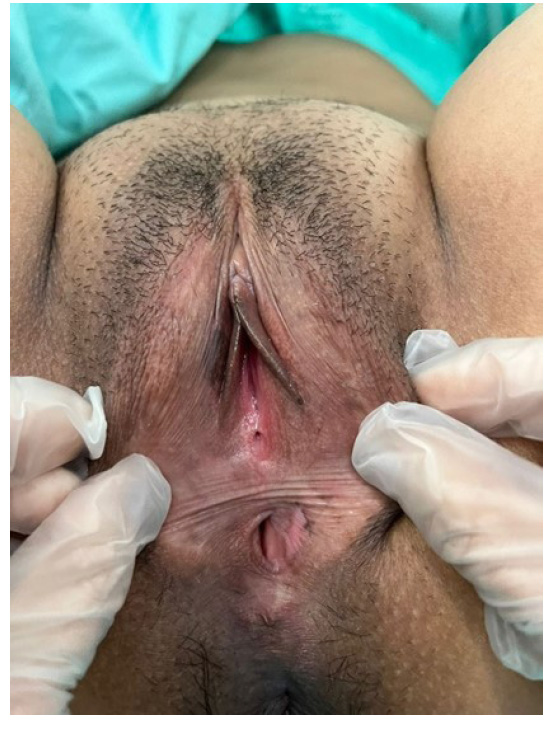
A 29-year-old female patient consulted for a 7-day clinical picture characterized by general malaise, headache, myalgias, arthralgias and unquantified fever, as well as a single lesion on the left labia majora of the vagina accompanied by burning sensation. With initial diagnosis of genital herpes and treatment with acyclovir 400 mg every 8 hours, on the second day of medical management she presented aphthous ulcers in oral mucosa, progression of vulvar lesions, pain and purulent discharge. She had a new consultation (Figure 1), being diagnosed as superinfected herpes and antibiotic management with intravenous clindamycin and enterostomal therapy was added.

Figure 1 aphtous ulcers in the oral mucosa and, in the vulvar region, edema in labia majora and minora, ulcerated lesions with presence of devitalized and granulation tissue.
After the first healing of the lesions, she presented vulvar edema, exacerbation of pain, fever of 39°C and bleeding in the lesions. She was evaluated by internal medicine and autoimmune disease was initially suspected, to rule out vasculitis or Behçet's disease. This diagnostic impression was associated with the history that in 2019 she presented with arthralgias and exanthema on the back of the hands, self-limited, with a report of positive antinuclear antibodies (ANAS), in addition to a family history of a sister with lupus and death of the maternal aunt due to complications associated with lupus. The specialist decided to initiate broad-spectrum antibiotic treatment with piperacillin/tazobactam 4.5 g every 8 hours intravenous and vancomycin 500 mg intravenous every 12 hours, in addition to requesting an immunological profile and evaluation by gynecology. This specialist also decided to perform surgical debridement plus specimen collection for biopsy and to add to the medical management aluminum hydroxide with nystatin and lidocaine mouthwash every 8 hours (Figure 2).
The day after the surgical procedure and already in charge of gynecology, dermatology consultation was requested, which did not rule out Behçet's disease and started prednisolone 50 mg per day orally. Gynecology suspended the broad-spectrum antibiotic therapy and started management with doxycycline 100 mg every 12 hours for 7 days, in addition to cures with phytostimulin. Two days later, there was resolution of the vulvar ulcers and clinical improvement of the pain. Acute phase reactants and positive ANAS were found to be increased.
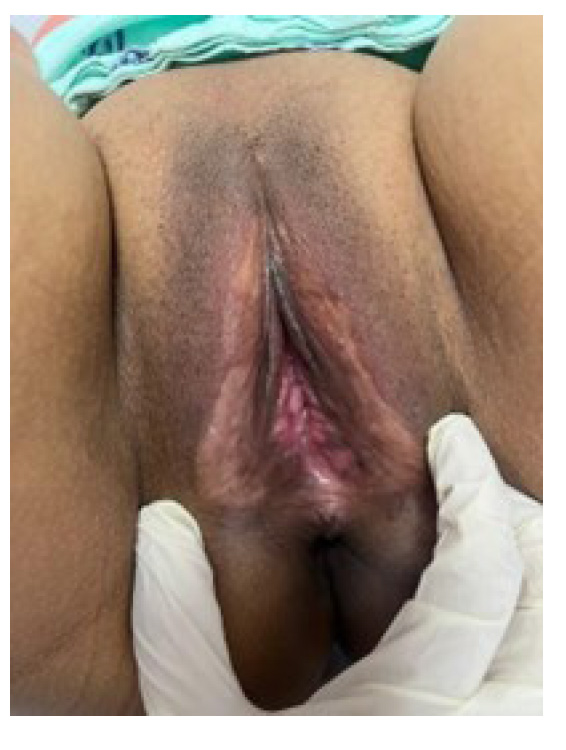
One week later, the patient was discharged. During the follow-up appointment with gynecology at one week, there was evidence of resolution of 90% of the lesions and formation of partial vulvar synechiae, which were asymptomatic. The pathology report was leukocytoclastic vasculitis. The patient was also evaluated by rheumatology, with a request for HLA-B, which was negative. Given the adequate clinical evolution, the patient underwent surgical resection of the vulvar synechiae, with good evolution and recovery of the vulvar anatomy (Figures 3 and 4).
DISCUSSION
The presence of oral and genital ulcers is a distinctive clinical feature of BD in the context of a patient with suspected autoimmunity, especially when there is concurrence of joint, ocular, cutaneous and neurological symptoms4,5).
Genital ulcers are common in women between the ages of 20-40 years and can occur on the labia, vulva and vagina. The frequent occurrence of genital ulcers in this age group may be related to a combination of environmental and hormonal factors. Most genital ulcers in women are of herpetiform morphology, although minor and major aphthous ulcers also occur1,9). In the clinical approach, it is recommended to perform a genetic study of major histocompatibility complex (HLA) typing and the pathergy test, since, although a rare disease in our environment, it can be clinically and pathologically underdiagnosed. It is important to know its different clinical manifestations and the requirement of a multidisciplinary approach4,10).
REFERENCES
1. Senusi A, Seoudi N, Bergmeier LA, Fortune F. Genital ulcer severity score and genital health quality of life in Behçet's disease. Orphanet J Rare Dis. 2015;10(1). doi: 10.1186/ s13023-015-0341-7 [ Links ]
2. Tursen U, Gurler A, Boyvat A. Evaluation of clinical findings according to sex in 2313 Turkish patients with behcet's disease. Intern J Dermatol. 2003;42(5):346-51. doi:10.1046/j.1365-4362.2003.01741.x [ Links ]
3. Davatchi F, Shahram F, Chams-Davatchi C, Shams H, Nadji A, Akhlaghi M, et al. Behcet's Disease: From east to West. Clin Rheumatol. 2010;29(8):823-33. doi: 10.1007/s10067-0101430-6 [ Links ]
4. Padilla-Ortiz D, Chamorro-Melo M, Santos AM, Arias-Correal J, Reyes-Martínez V, Rueda JC, et al. Enfermedad de Behçet: Un reto diagnóstico en Reumatología. Descripción de una serie de casos Y revisión de la literatura. Rev Colomb Reumatol. 2020;27(4):308-16. doi: 10.1016/j.rcreu.2020.01.003 [ Links ]
5. Arévalo-Rodríguez I, Sierra F, Quintana G. Detección de antígenos leucocitarios humanos para el diagnóstico de la enfermedad de Behcet. Bogotá D.C.: Fundación Universitaria de Ciencias de la Salud, IETS; 2014. [ Links ]
6. Gilworth G, Chamberlain MA, Bhakta B, Haskard D, Silman A, Tennant A. The development of the BD-QoL: a quality-of-life measure specific to Behçet's disease. J Rheumatol. 2004;31:931-7. [ Links ]
7. Hié M, Amoura Z. Enfermedad de Behçet. EMC Aparato Locomotor. 2017;50(3):1-9. doi.org/10.1016/S1286935X(17)86067-6 [ Links ]
8. Zúñiga Villegas A, Kriebel Haehner M, Morún Calvo D, Monge Luna LD. Enfermedad de Behcet: Reporte de caso y revisión de literatura. Rev Ciencia Salud Integrando Conocimientos. 2020;4(6). doi.org/10.34192/cienciaysalud. v4i6.227 [ Links ]
9. Faezi ST, Chams-Davatchi C, Ghodsi SZ, Shahram F, Nadji A, Akhlaghi M, et al. Genital aphthosis in Behçet's disease: Is it associated with less eye involvement? Rheumatol Intern. 2014;34(11):1581-7. doi:10.1007/s00296-014-3011-5 [ Links ]
10. Paucar-Lescano PK. Presentación Muco-Cutánea de la enfermedad de Behcet. Corcordancia de enfoques terapéuticos. Reporte de Caso y Revisión de Literatura. Rev Peru Invest Salud. 2022;6(2):107-14. https://doi.org/10.35839/ repis.6.2.1122 [ Links ]
Received: September 15, 2022; Accepted: February 19, 2023











 text in
text in