Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.2 Lima Apr./Jun. 2023 Epub July 06, 2023
http://dx.doi.org/10.31403/rpgo.v69i2521
Case report
Primary retroperitoneal ectopic pregnancy
1 Obstetrics and Gynecology Service, "Dr. Urquinaona" Central Hospital, Maracaibo, Zulia State, Venezuela
Ectopic pregnancy accounts for 1.5%-2% of all pregnancies and is a common cause of pregnancy-related mortality during the first trimester. The most common location is the fallopian tube and less than 2% are abdominal pregnancies. Retroperitoneal ectopic pregnancy is an extremely rare type with a rather complex pathogenesis. This unusual location has a high risk of life-threatening complications. Early diagnosis is difficult because of the inability to differentiate signs, symptoms, chorionic gonadotropin concentrations, and imaging with ectopic pregnancies from unusual locations, such as the retroperitoneum. In addition, it is necessary to be careful with the diagnosis of these cases when the most common sites of appearance do not present alterations. Treatment consists of removal of trophoblastic tissue by laparotomy or laparoscopy. A case of primary retroperitoneal ectopic pregnancy is presented.
Key words: Pregnancy; ectopic; retroperitoneal
Introduction
Ectopic pregnancy is the implantation of the fertilized egg in a location other than the endometrium. It occurs in the fallopian tubes in 95% of the cases, while the ovarian and abdominal location is less frequent1,2. Abdominal ectopic pregnancy represents 2% of all cases and can be classified as primary or secondary. Implantation may occur in the cul-de-sac of Douglas or in the posterior part of the uterus, liver, spleen and diaphragm3,4. The retroperitoneal space is an exceptional site of implantation and there are fewer than 30 case reports of primary implantation2,5,6. A case of primary retroperitoneal ectopic pregnancy is presented.
Case report
A 26-year-old female patient with two pregnancies and two miscarriages came to the emergency room with abundant genital bleeding, accompanied by continuous severe pain in the lower hemiabdomen of approximately 12 hours of evolution, along with nausea and rectal pressure. The date of the last menstrual period was 7 weeks prior to the onset of symptoms. She reported menarche at 16 years of age with regular 28-day cycles lasting 7 days with moderate bleeding and no pain. She had a history of appendectomy at age 12 with no complications. In addition, a privately performed qualitative pregnancy test was positive.
Physical examination revealed moderate cutaneous-mucosal pallor and she was oriented in time, space and person. Blood pressure was 90/60 mmHg, respiratory rate was 20 breaths/minute and heart rate were 110 beats/minute. Abdominal evaluation found lower hemiabdomen pain with increased tenderness to both superficial and deep palpation, but no guarding. Gynecological examination found the uterus enlarged and intrapelvic, soft and smooth surfaces, smooth cervix, mild pain on palpation and mobilization. The adnexa were not palpable. There was bleeding in moderate amount of bright red color.
Transvaginal ultrasound evaluation showed an enlarged uterus with endometrial thickness of 15 millimeters, without evidence of intrauterine gestational sac. Both adnexa were normal and without tumors. However, a tumor of approximately 50 millimeters in diameter, slightly hyperechogenic and heterogeneous, with gestational sac and embryo inside without evidence of cardiac activity, was observed (Figure 1). There was free fluid in the Douglas cul-de-sac. Laboratory tests showed the following values: hemoglobin 7.8 g/dL, leukocytes 8,300/mL and platelets 353,000/mL. Chorionic gonadotropin concentrations were 59,756 mIU/mL. The rest of the liver and renal functional tests, urine examination, electrolytes and coagulation tests were within normal limits. In view of the findings, it was decided to perform emergency laparoscopic exploration.
During surgery, approximately 500 mL of free blood was found in the abdominal and pelvic cavity. The uterus was enlarged, with smooth surfaces and no evidence of bleeding. The left adnexa were normal. The right fallopian tube appeared normal, and the ipsilateral ovary was enlarged, but without evidence of macroscopic changes. There was no evidence of rupture, adhesions or bleeding of any of these structures. After removing all the free fluid in the cavity, a rounded tumor, approximately 20 millimeters in diameter, was observed adjacent to the right pelvic wall, with the appearance of a gestational sac covered by parietal peritoneum and together with hematoma extending from the right paracolic canal to the presacral area. The peritoneum was intact, bluish in color and bled when pressed. The retroperitoneal space was carefully dissected, the tumor was adjacent to the ureter, and the neighboring organs showed no obvious damage (Figure 2). The clots and gestational tissues were removed and irrigated with saline. It was then observed that part of the left ureter showed edema. Absorbable hemostatic cellulose was placed in the retroperitoneal space to prevent bleeding. After insertion of the drainage tube into the posterior peritoneal cavity, the peritoneum was closed and the surgery was concluded without complications.
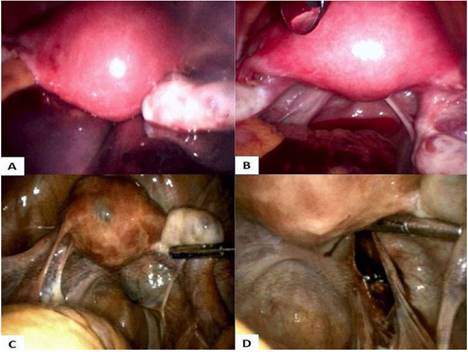
Figure 2 Laparoscopic findings. A) Retroperitoneal hematoma located in the right paracolic space and presacral area. B) Uterus and pelvic peritoneum were intact. C) Tumor in retroperitoneum. D) After resection of the retroperitoneal ectopic pregnancy.
Histopathological analysis of the tumor showed chorionic villi with normal embryo, gestational sac and peritoneal tissue. The definitive diagnosis was retroperitoneal ectopic pregnancy (Figure 3).
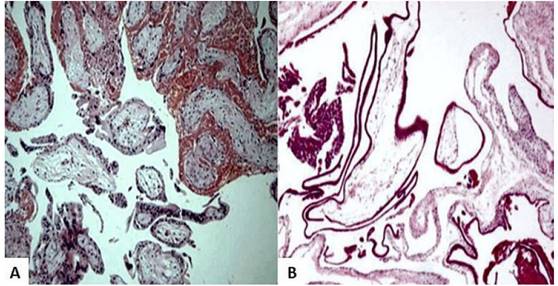
Figure 3 Microscopic image of the lesion. A) Chorionic villi. B) Chorionic villi and trophoblastic tissue adhered to the peritoneal tissue (hematoxylin-eosin staining, 100x).
The patient evolved satisfactorily and the postoperative course was uneventful, being discharged on the third day. Chorionic gonadotropin concentrations at discharge were 430 mIU/mL. Blood concentrations of gonadotropin were measured weekly and reached undetectable values 29 days after surgery.
Discussion
Ectopic pregnancy represents approximately 2% of all pregnancies and its incidence has increased 6-fold in the last two decades. It is a common emergency in obstetrics and accounts for 13% of all pregnancy-related deaths7. Its pathogenesis is unknown, although adhesive changes in the pelvis, including the fallopian tubes, have been proposed as a possible cause8.
Abdominal ectopic pregnancy is the rarest form of ectopic pregnancy (1.4% of all ectopic pregnancies) with mortality rates 8 times higher compared to non-abdominal ectopic pregnancies and approximately 90 times higher than that of intrauterine pregnancy2. This is because it is difficult to diagnose and is associated with higher morbidity and mortality, especially due to massive hemorrhage when implanted near large caliber blood vessels9. The most common sites of abdominal pregnancy are the fornix of Douglas, posterior uterine wall, infundibulopelvic ligaments, anterior abdominal wall, omentum, liver, spleen and diaphragm. In exceptional cases, embryo implantation occurs in the retroperitoneal space8.
Ectopic pregnancies can be classified as primary or secondary. Most cases are secondary since the fertilized eggs implanted in the fallopian tubes or ovaries probably become detached and secondarily reach the abdominal cavity to implant2. Only a small fraction of cases meets the criteria for primary abdominal ectopic pregnancy: normal fallopian tubes and ovaries without evidence of recent or old damage, absence of utero-peritoneal fistula, implantation site limited exclusively to the peritoneal surface and diagnosed early to exclude the possibility of secondary implantation10.
The pathogenesis of primary retroperitoneal ectopic pregnancy is complex and not yet well understood. However, there are several theories that attempt to explain it. The retroperitoneal sinus theory proposes that the blastocyst transits through a communication between the fallopian tube and the retroperitoneal space, especially in patients with a history of pelvic surgery11. Some communications have reported that the fertilized ovum can migrate through lymphatic vessels, as do metastatic cells, consistent with the lymphatic migration theory. This is supported by the fact that retroperitoneal ectopic pregnancies appear near retroperitoneal vessels and that both vessels and lymphatic tissues are enlarged at the implantation site12. However, these changes in the lymphatic tissues have been reported in few cases. Another theory suggests that the embryo may initially implant on the posterior peritoneal surface and reach the retroperitoneal space after trophoblastic invasion. The peritoneal defect would indicate the original location of penetration13.
Preoperative diagnosis of retroperitoneal ectopic pregnancy is a real challenge. Symptoms are similar to the symptomatology of ectopic pregnancy in other locations (nausea, vomiting, constipation, amenorrhea and vaginal bleeding). Most cases present with variable abdominal pain. As the gestational sac grows, pressure increases on the surrounding peritoneal surface, which would increase the frequency and severity of pain. If there is invasion of neighboring organs, such as bowel or bladder, symptoms may simulate obstruction or inflammation of these organs4.
The main diagnostic tool is transvaginal ultrasound together with quantitative determination of serum human chorionic gonadotropin values. However, if the location is extrapelvic, ultrasonography is of little use and the diagnosis may be difficult to make. Computed tomography and magnetic resonance imaging are useful diagnostic tools. In addition, they can help visualize the relationship between the gestational sac and neighboring organs-blood vessels. Computed tomography images show the placental position better, compared to ultrasound or MRI, but their use in pregnancy is limited by fetal exposure to ionizing radiation14.
There are no single, well-defined therapeutic guidelines for the management of retroperitoneal ectopic pregnancy2. The ideal surgical approach is surgical removal of the retroperitoneal gestational sac. The traditional treatment is laparotomy with removal of the embryo with or without placental tissue. In hemodynamically stable cases, the laparoscopic approach may be the technique of choice, as it can reduce operative time, minimize blood loss, hospital stay and cost of surgery. However, it is necessary to consider the location of the ectopic pregnancy, degree of tissue involvement, knowledge of the anatomical structure of the retroperitoneum and experience of the surgeon. Therefore, it is necessary to exclude retroperitoneal vascular involvement with MRI, especially in pregnancies with advanced gestational age15. The removal of placental tissue in ectopic pregnancy with gestational age greater than 12 weeks is controversial. The general recommendation is to completely remove the trophoblastic tissue and, if possible, to perform ligation of the blood vessel. Remnants of placental tissue can cause intestinal obstruction, peritonitis, massive hemorrhage and hypovolemic shock4.
The use of methotrexate (systemic or by selective arterial embolization) is widely accepted as an adjuvant treatment to control the risk of bleeding from placental remnants and to decrease the amount of persistent trophoblastic tissue after surgery. There are case reports of early abdominal ectopic pregnancies successfully treated with systemic methotrexate without additional surgery5. However, surgical treatment is indicated when there is ruptured ectopic pregnancy, serum chorionic gonadotropin concentrations equal to or greater than 5,000 IU/L, fetal cardiac activity or suspected heterotopic pregnancy5,16.
In conclusion, primary retroperitoneal ectopic pregnancy is a diagnostic challenge due to its low frequency and different clinical manifestations. In those cases where suspicion exists, attention should be paid to look for nonspecific signs and symptoms when findings at the most common sites of ectopic pregnancy location do not present positive results. Both surgery, laparotomy or laparoscopy and medical treatment with methotrexate are useful in the treatment of cases of retroperitoneal ectopic pregnancy.
REFERENCES
1. Xu H, Cheng D, Yang Q, Wang D. Multidisciplinary treatment of retroperitoneal ectopic pregnancy: a case report and literature review. BMC Pregnancy Childbirth. 2022;22(1):472. doi: 10.1186/s12884-022-04799-5 [ Links ]
2. Eisner SM, Ebert AD, David M. Rare ectopic pregnancies - A literature review for the period 2007 - 2019 on locations outside the uterus and fallopian tubes. Geburtshilfe Frauenheilkd. 2020;80(7):686-701. doi: 10.1055/a-1181-8641 [ Links ]
3. Barel O, Suday RR, Stanleigh J, Pansky M. Laparoscopic removal of an abdominal pregnancy in the pelvic sidewall. J Minim Invasive Gynecol. 2019;26(6):1007-8. doi: 10.1016/j. jmig.2018.12.020 [ Links ]
4. Ouassour S, Filali AA, Raiss M, Bezad R, Tazi Z, Alami MH, Bennani J, Dafiri R. Retroperitoneal ectopic pregnancy: Diagnosis and therapeutic challenges. Case Rep Surg. 2017;2017:9871865. doi: 10.1155/2017/9871865 [ Links ]
5. Anh ND, Hai NX, Ha NT, Toan NK, Thuong PH, Duc NM. Retroperitoneal ectopic pregnancy after in vitro fertilization: A case report of a patient with bilateral salpingectomy. Radiol Case Rep. 2021;17(3):721-4. doi: 10.1016/j.radcr.2021.12.011 [ Links ]
6. OuYang Z, Wei S, Wu J, Wan Z, Zhang M, Zhong B. Retroperitoneal ectopic pregnancy: A literature review of reported cases. Eur J Obstet Gynecol Reprod Biol. 2021;259:113-8. doi: 10.1016/j.ejogrb.2021.02.014 [ Links ]
7. Lu Q, Zhang Z, Zhang Z. Laparoscopic management of retroperitoneal ectopic pregnancy. J Minim Invasive Gynecol. 2019;26(3):405-6. doi: 10.1016/j.jmig.2018.07.007 [ Links ]
8. Zhang M, Qin LL. A case of retroperitoneal para-aortic ectopic pregnancy detected by sonography. J Clin Ultrasound. 2018;46(6):412-4. doi: 10.1002/jcu.22554 [ Links ]
9. Tegene D, Nesha S, Gizaw B, Befikadu T. Laparotomy for advanced abdominal ectopic pregnancy. Case Rep Obstet Gynecol. 2022;2022:3177810. doi: 10.1155/2022/3177810 [ Links ]
10. Abedin Y, Chadha K. Case of ruptured ectopic pregnancy in the uterosacral ligament and review of the literature. Case Rep Obstet Gynecol. 2020;2020:5897341. doi: 10.1155/2020/5897341 [ Links ]
11. Jones DD, Kummer T, Schoen JC. Ruptured ectopic pregnancy with an intrauterine device: case report and sonographic considerations. Clin Pract Cases Emerg Med. 2020;4(4):559-63. doi: 10.5811/cpcem.2020.7.48258 [ Links ]
12. Pak JO, Durfee JK, Pedro L, Osborne A, Larkins-Pettigrew M. Retroperitoneal ectopic pregnancy. Obstet Gynecol. 2018;132(6):1491-3. doi: 10.1097/AOG.0000000000002965 [ Links ]
13. Tong A, Pu Y, Ye J, Qi X. Complete resection of retroperitoneal ectopic pregnancy adherent to the inferior vena cava by laparoscopy. J Minim Invasive Gynecol. 2022;29(7):810-1. doi: 10.1016/j.jmig.2022.03.009 [ Links ]
14. Yang Y, Liu Z, Song L, Liu H, Li L, Meng Y. Diagnosis and surgical therapy of the retroperitoneal ectopic pregnancy: A case report. Int J Surg Case Rep. 2018;49:21-4. doi: 10.1016/j.ijscr.2018.05.027 [ Links ]
15. Veleminsky M, Stepanek O, Koznar P, Michal M, Mainzerová P, Stikova Z. A rare case of ectopic pregnancy - retroperitoneal ectopic pregnancy. Neuro Endocrinol Lett. 2018;39(3):156-9. [ Links ]
16. Dardalas I, Rigopoulos P, Pourzitaki C. Treatment of ectopic pregnancy with methotrexate. Arch Gynecol Obstet. 2019 Oct;300(4):1093-4. doi: 10.1007/s00404-019-05248-z [ Links ]
Statement of ethical issues
Ethical responsibilities: Protection of persons. We authors declare that the procedures followed conformed to the ethical standards of the committee on responsible human experimentation and in accordance with the World Medical Association and the Declaration of Helsinki.
Confidentiality of data: The authors declare that the protocols of the Ecuadorian Institute of Social Security on the publication of patient data were followed.
Right to privacy and informed consent: The authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Funding: We the authors certify that we have not received financial, equipment, personal or in-kind support from individuals, public and/or private institutions for the conduct of the study.
Received: August 31, 2022; Accepted: January 20, 2023











 text in
text in 




