Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.2 Lima Apr./Jun. 2023 Epub July 06, 2023
http://dx.doi.org/10.31403/rpgo.v69i2522
Case report
Primary ovarian leiomyoma
1Doctor en Medicina Clínica. Especialista en Ginecología y Obstetricia. Servicio de Obstetricia y Ginecología, Hospital Central “Dr. Urquinaona”, Maracaibo, Venezuela.
Leiomyoma is a common benign mesenchymal tumor that can develop wherever smooth muscle is present; rare as a primary ovarian tumor, its origin is still controversial. Primary ovarian leiomyoma is one of the rarest benign ovarian tumors, accounting for 0.5% 1% of benign tumors and is usually seen in women between 20 and 65 years of age. They are usually asymptomatic and appear incidentally during a pelvic examination or surgery for another cause but can occasionally manifest by abdominal pain and palpable mass. Definitive diagnosis is difficult before surgical removal. Because there are no pathognomonic symptoms and no characteristic imaging, the main differential diagnoses include fibroma, thecoma, sclerosing stromal tumor and leiomyosarcoma. Immunohistochemical staining is essential for accurate diagnosis and should be considered in the differential diagnosis of ovarian spindle cell tumors. A case of primary ovarian leiomyoma is presented.
Key words: Leiomyoma; Ovary; Ovarian neoplasms
INTRODUCTION
Primary ovarian leiomyoma is a rare solid tumor arising from ovarian smooth muscle cells and accounts for 0.5%-1% of benign ovarian tumors1). Most cases usually appear between the second and eighth decade of life. However, approximately 80% of cases occur in premenopausal women2). Histologic features and immunohistochemical staining are fundamental to make the diagnosis and to differentiate them from other ovarian tumors, such as fibroma, thecoma and sclerosing stromal tumor3). A case of primary ovarian leiomyoma is presented.
CASE REPORT
A 45-year-old nulliparous female patient presented with mild to moderate hypogastric pain of 4 months of evolution, accompanied by abdominal distension. She denied menstrual alterations and family and/ or personal history of importance, smoking, alcohol or illicit drug consumption and use of hormonal treatment.
Physical examination showed a non-painful pelvic lesion with regular borders, mobile, of hard consistency, located on the right side of the uterus and separated from it. On vaginal examination, the cervix was normal with evidence of genital bleeding from the uterine cavity. No pelvic lymphadenopathy was found. The rest of the physical examination was within normal limits.
Hematology, liver and renal function tests, inflammatory markers, coagulation profile, electrolytes and urine examination were unaltered. Serum tumor markers (human chorionic gonadotropin, CA-125, CA-19.9, alpha-fetoprotein, carcinoembryonic antigen, and lactate dehydrogenase) were within normal limits.
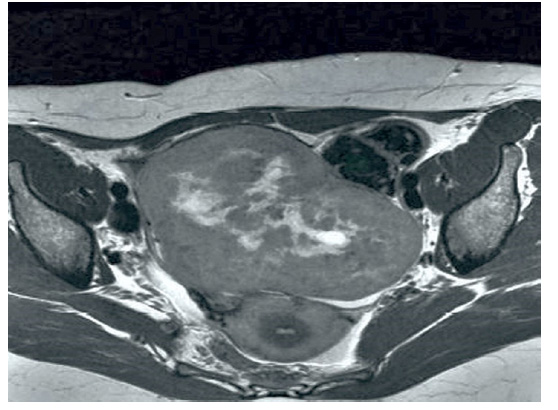
Pelvic ultrasound showed a solitary, solid, well-defined lesion, with some cysts inside, isoechoic pattern, homogeneous, located in the right adnexa, measuring 14 x 7 x 6 centimeters. There was a small amount of free fluid in the abdominal cavity. The uterus measured 7.4 x 4.5 millimeters and was separated from the tumor. There was no evidence of pathologic flow pattern on Doppler ultrasound evaluation. Magnetic resonance imaging confirmed the ultrasound findings showing encapsulated, well-defined tumor approximately 13 centimeters in diameter that showed low-intensity signals on T1and T2-weighted images. There was no evidence of omentum thickening or capsule penetration. The diagnosis was possible ovarian fibroma, so the patient was scheduled for surgery.
During laparotomy, approximately 150 mL of free fluid was found in the abdominal cavity. The right ovary was enlarged, with a large smooth-surfaced solid tumor without adhesions or infiltration of neighboring structures and clearly separated from the uterus. The frozen section biopsy was compatible with ovarian leiomyoma. Both the uterus and the contralateral adnexa were macroscopically normal. The pelvic and para-aortic nodes were not palpable. Total hysterectomy without adnexal preservation was performed at the patient's request and the surgical specimen was sent to anatomic pathology. The postoperative course was uneventful and the patient was discharged on the fourth postoperative day.
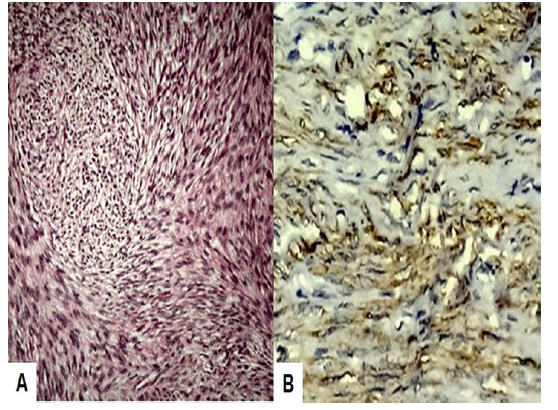
Anatomopathologic evaluation showed that the right ovary had a solid, smooth, firm tumor separated from the uterus. Cut section revealed grayish-white, well-circumscribed, encapsulated tumor with a thick nodular appearance, measuring 13 centimeters in diameter, with compressed ovarian stroma. Microscopic examination showed fascicles and interlacing bundles of dense cells with elongated rod-shaped nuclei, interspersed with foci of collagen deposits, thickened blood vessels and some areas of hyalinization, with no evidence of nuclear pleomorphism, atypia and/or necrosis. The mitotic count was less than 1 per 10 high power fields. With immunohistochemical staining, the cells were strongly positive for smooth muscle actin and diffusely positive for desmin and vimentin, but negative for inhibin. The Ki-67 proliferation index was less than 1%. Ascitic fluid cytology did not show the presence of neoplastic cells. Both the uterus and the left adnexa were unaltered. Histopathological findings confirmed the diagnosis of primary ovarian leiomyoma.
DISCUSSION
Ovarian tumors can be classified into several categories according to their origin. Although most primary tumors arise from surface epithelium, sex-stromal cords and germ cells, there are varieties of rare neoplasms arising from other sometimes unknown lineages2). Primary ovarian leiomyoma was first described in 1862 and there are reports of about 80 cases4). They are usually benign, asymptomatic tumors, smaller than 3 centimeters in diameter5,6).
The histogenesis of primary ovarian leiomyomas is not yet well established. Some authors suggest that they probably arise from smooth muscle cells of ovarian hilar blood vessels, ovarian ligament, multipotential ovarian stromal cells, germ cells undifferentiated by cortical smooth muscle metaplasia of the endometriotic stroma, smooth muscle present in mature cystic teratomas and/or from the wall of the mucinous cystic tumor7-9). Most patients with primary ovarian leiomyomas are nulligesta, suggesting that estrogens may play a pivotal role in their appearance and development. Another hypothesis suggests that they may arise in ovaries with abnormalities during embryonic development10).
Primary ovarian leiomyomas are usually asymptomatic and are usually detected during routine physical examination, surgical interventions, or autopsies. However, large tumors may be symptomatic. Abdominal pain is the most common symptom and on rare occasions they may present with hydrothorax, ascites, hydronephrosis, Meigs syndrome or polymyositis2,5). Most cases are unilateral, although there are some cases of bilateral presentation in pediatric/young adult patients, especially under 35 years of age2,9). These tumors do not produce menstrual disturbances or abnormal genital bleeding. Some tumors may be accompanied by hilum cell hyperplasia resulting in virilization due to testosterone production11).
Preoperative evaluation of primary ovarian leiomyomas includes ultrasonography, MRI and tumor markers. Ultrasonography shows a solid tumor isoechoic with the myometrium, making it difficult to differentiate from other solitary tumors. Resonance imaging can be a useful diagnostic adjunct12,13). However, it is not able to distinguish between leiomyoma, fibroma, tecoma or leiomyosarcoma4).
The correct diagnosis of primary ovarian leiomyoma requires the identification of smooth muscle cells in the tumor. But due to their rarity, other tumors should be included among the differential diagnoses such as fibromas, thecomas, fibrotecomas, sclerosing stromal tumors and sex cord stromal tumors1). They should also be differentiated from ovarian leiomyosarcoma,but due to the rarity of both tumors the characteristics of malignancy have not yet been well defined. Traditionally, the criteria to be considered are mitotic count, cytologic atypia and tumor necrosis to consider the possibility of malignancy5).
Another distinctive feature of primary ovarian leiomyomas is that they must appear completely within the ovary without coexistent uterine myomas5). However, different studies have described coexistence with uterine leiomyomas. One study found that more than half of the cases of ovarian leiomyomas were associated with uterine leiomyomas with similar histologic features14).
Masson's trichrome staining helps to differentiate fibrous and smooth muscle components in the lesion15). Immunohistochemical stains have great diagnostic utility4). Smooth muscle alpha-actin and inhibin allow differentiation from fibromatous tumors. Diffuse positivity to desmin of tumor cells is typical of leiomyomas, whereas fibromatous tumors collectively are negative or show only focal positivity. Thecomas are strongly positive for α-inhibin and do not express smooth muscle alpha-actin3).
The treatment of choice for patients with primary ovarian leiomyomas is complete surgical resection (oophorosalpingectomy or oophorectomy) with or without hysterectomy. However, in young women other fertility preserving procedures should be considered2).
In conclusion, primary ovarian leiomyoma is a rare benign tumor. It should be considered as a differential diagnosis from other benign solid ovarian tumors such as fibroma, thecoma, sclerosing stromal tumor. Histologic features and immunohistochemistry help to reach a definitive diagnosis.
REFERENCES
1. Wang QM, Zhao Y, Ma Y, Yao LT, Han X. One case report of giant atypical leiomyoma of the ovary. Medicine (Baltimore). 2018;97(40):e12526. doi: 10.1097/MD.0000000000012526 [ Links ]
2. Raje S, Arvind S, Rao G, Chawla L. Primary ovarian leiomyoma. Gynecol Minim Invasive Ther. 2020;9(3):182-183. doi: 10.4103/ GMIT.GMIT_14_19 [ Links ]
3. Rajabi P, Hani M, Bagheri M, Mirzadeh F. Large ovarian leiomyoma in young woman. Adv Biomed Res. 2014;3:88. doi: 10.4103/2277-9175.128001 [ Links ]
4. Ozcimen EE, Oktem M, Zeyneloglu HB, Ozdemir BH, Kuscu E. Primary leiomyoma of the ovary in a young woman: literature review and report of a case. Eur J Gynaecol Oncol. 2006;27(3):310-2. [ Links ]
5. Liang G, Wu Z, Zhu L, Ruan F. Case report: Primary ovarian leiomyoma: A clinical analysis of case series and literature review. Front Med (Lausanne). 2022;9:822339. doi: 10.3389/fmed.2022.822339 [ Links ]
6. Blue NR, Felix JC, Jaque J. Primary ovarian leiomyoma in a premenarchal adolescent: first reported case. J Pediatr Adolesc Gynecol. 2014;27(4):e87-8. doi: 10.1016/j.jpag.2013.07.011 [ Links ]
7. Hacivelioglu S, Erkanli S. A large pedunculated leiomyoma with two-sided cystic degenerations mimicking a bilateral ovarian malignancy: a case report. Eur J Gynaecol Oncol. 2014;35(2):192-4. [ Links ]
8. Alshwairikh K, AlOtaibi W, Alshammari S, Alshammari T, Hakami R, Alswayyed M, et al. Cystic Ovarian Leiomyoma in a Patient with Progressive Abdominal Pain. Am J Case Rep. 2021;22:e930299. doi: 10.12659/AJCR.930299 [ Links ]
9. Meel M, Hemrajani D, Kumar M, Agnani B. Symptomatic primary ovarian leiomyoma in a postmenopausal woman: A rare entity. J Midlife Health. 2020 Jul;11(3):175-7. doi: 10.4103/jmh. JMH_105_19 [ Links ]
10. Bharti S, Khera S, Sharma C, Balakrishnan A. Unilateral primary ovarian leiomyoma masqueraded as ovarian fibroma: A histopathological diagnosis. J Family Med Prim Care. 2021;10(9):3494-7. doi: 10.4103/jfmpc.jfmpc_2546_20 [ Links ]
11. Parish JM, Lufkin EG, Lee RA, Gaffey TA. Ovarian leiomyoma with hilus cell hyperplasia that caused virilization. Mayo Clin Proc. 1984;59(4):275-7. doi: 10.1016/s0025-6196(12)61262-2 [ Links ]
12. Alshwairikh K, AlOtaibi W, Alshammari S, Alshammari T, Hakami R, Alswayyed M, et al. Cystic ovarian leiomyoma in a patient with progressive abdominal pain. Am J Case Rep. 2021;22:e930299. doi: 10.12659/AJCR.930299 [ Links ]
13. Kurai M, Shiozawa T, Noguchi H, Konishi I. Leiomyoma of the ovary presenting with Meigs' syndrome. J Obstet Gynaecol Res. 2005;31(3):257-62. doi: 10.1111/j.1447-0756.2005.00285.x [ Links ]
14. Kitamura Y, Ito F, Kokabu T, Mori T, Kusuki I, Kitawaki J. Primary ovarian leiomyoma associated with multiple uterine leiomyomas. Gynecol Minim Invasive Ther. 2021;10(1):50-52. doi: 10.4103/GMIT.GMIT_97_19 [ Links ]
15. Kim M. Laparoscopic management of a twisted ovarian leiomyoma in a woman with 10 weeks' gestation: Case report and literature review. Medicine (Baltimore). 2016;95(44):e5319. doi: 10.1097/MD.0000000000005319 [ Links ]
Declaration of ethical aspects
Ethical responsibilities: Protection of persons. The author declares that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Confidentiality of data: The author declares that he has followed the protocols of the Hospital Central de Maracaibo on the publication of patient data.
Right to privacy and informed consent: The author has obtained the informed consent of the patient and/ or subject referred to in the article. This document is in the possession of the corresponding author.
Funding: The author certifies that he/she has not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the realization of the study.
Received: January 24, 2023; Accepted: March 01, 2023











 text in
text in