Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.3 Lima July/Sep. 2023 Epub Oct 16, 2023
http://dx.doi.org/10.31403/rpgo.v69i2544
Original paper
Quality of work life and risk of sexual dysfunction in nurses
1. Faculty of Medicine, Universidad Científica del Sur, Lima, Peru
2. Neuroscience, Effectiveness and Public Health Research Group, Universidad Cientifica del Sur, Lima, Peru
Unsatisfactory personal experiences and relationships in the work environment are associated with negative sexual outcomes. Female sexual dysfunction (FSD) is the disturbance of any of the phases of orgasm. Quality of work life (QWL) is the worker's perception between work demands and coping techniques.
Objective:
To determine the association between quality of work life and the risk of female sexual dysfunction in nurses of a public hospital in Callao, Peru.
Methods:
Observational, cross-sectional, analytical study conducted in nurses of the Hospital Nacional Daniel Alcides Carrión (HNDAC) of the Constitutional province of Callao, Peru. The risk of FSD was measured with the Rosen test. CVL was measured with the CVP35 questionnaire. Statistical analysis was performed with the STATA version 15 program. A value of p<0.05 with a 95% CI was considered significant.
Results:
The study involved 168 nurses who responded completely. The dimensions of CVL associated with DSF were direct support (p=0.01), intrinsic motivation (p=0.003), the question on work disconnection (p=0.007), monthly income (p=0.003), marital status (p=0.001) and alcohol consumption (p=0.014). There was no association in the multivariate analysis.
Conclusion:
In the present study there was no association between dimensions of quality of work life and confounder-adjusted risk of female sexual dysfunction.
Key words: Work-life balance; Sexual dysfunction; Nurses; female
Introduction
Female sexual dysfunction (FSD) has increased worldwide, with prevalence varying by region. In Spain, a prevalence of up to 42.5% has been reported1, while in the Middle East it reaches 61%2. In Latin America, specifically in Mexico, the prevalence of FSD is 43%3, while in Peru, the risk in young university women reaches 39.9%4. Likewise, it has been published that women working in the health sector have a FSD of 85%, with 75% of alterations in sexual desire5.
‘Normal' female sexual function is defined on the basis of statistical values, cultural norms, or both4 and is divided into four stages: arousal, plateau, orgasm, and resolution. Sexual dysfunction is a disturbance in any of these stages and its prevalence is higher in adulthood and old age5. Although accurate diagnosis is made by a mental health professional through the application of the DSM-5 Manual6, screening instruments can be useful in estimating the risk of FSD.
Good sexual health can offer a number of benefits. Sexual intercourse is considered a form of mild-to-moderate intensity physical activity, similar to climbing two flights of stairs or walking briskly7. Regular sexual intercourse can enhance endothelial nitric oxide synthase (eNOS) expression and increase nitric oxide (NO) production, leading to vasodilation and explaining its cardiovascular benefits8. On an emotional level, pleasurable intercourse can reduce the burden of stress load and improve the quality of the couple's relationship, strengthening intimacy, trust, passion, and love7.
There are factors associated with the risk of FSD, such as marriage of 10 or more years, low frequency of sexual intercourse, dissatisfaction or poor communication with the partner, lack of affection in the marital relationship, sexual impotence of the partner, low level of education, age over 40 years, multiparity, postmenopausal state, medical history (pelvic surgeries, depression, consumption of certain medications, harmful habits), history of physical mistreatment, sexual abuse or both; as well as working in inadequate working conditions6.
Quality of work life (QWL) refers to the worker's perception of the balance between work demands and the coping strategies he/she uses9. This variable is composed of psychological and social factors that include subjective elements linked to personal experience at work, as well as objective factors that relate to the work environment and content10. In the case of health personnel in Spain, the QWL score was medium-high11, while in Latin America only 30% of employees reported having an QWL considered high12.
Regarding the association between QWL and the risk of FSD, unsatisfactory personal experiences and relationships in the work environment are associated with negative sexual outcomes, with work stress being an intervening variable in this relationship13. For some women, occupational stress was independently associated with reduced orgasm and lubrication14. For example, health care personnel working during epidemics were affected psychologically and sexually by the heavy workload. Reports during the COVID 19 pandemic indicate a marked association between decreased sexual desire (OR: 2.6; p=0.001) and being a health care worker15. Job stress is known to be frequent in nurses due to work overload in both inpatient and outpatient services16. The association between QWL and sexual health has not been fully studied in this occupational group in the context of the COVID 19 pandemic17. Therefore, our main objective was to determine the association between QWL and the risk of FSD adjusted for potential confounders in nurses at a public hospital in the constitutional province of Callao, Peru. Secondarily, we also identified some associated variables.
Methods
An observational, cross-sectional, analytical study was conducted following the recommendations of the strategy for strengthening the reporting of observational studies in epidemiology (STROBE)18. The study population consisted of nurses from the Hospital Nacional Daniel Alcides Carrión (HNDAC) in the Constitutional province of Callao, Peru. The HNDAC has 565 inpatient beds and is one of the hospitals with the highest workload in the entire region19.
The study included nurses with an active work contract with the HNDAC, with a minimum of 12 months of experience and who agreed to participate, as long as they did not have a history of depression. Files that did not have data on the main variables were excluded. The sample size was calculated using the mean comparison formula of our quantitative independent variable (QWL) divided into two groups according to the presence or absence of our outcome variable (FSD). We used the online statistical program OpenEpi Version 3.1, with a confidence level of 95% and a statistical power of 80%. The research team conducted a pilot study in 202120, the results of which are available online. From these results, a mean difference of 1.08 was considered. The minimum required size was 86 participants for the group with RDSF and 68 for the group without RDSF.
To carry out the data collection, nurses were asked to voluntarily participate in their workplaces, giving them the option of completing the survey in physical or digital format through a form on the Google Forms platform. The time required to complete the survey was around 30 minutes, but an extension of up to 24 hours was allowed if requested by the research subject. Non-probability convenience sampling was carried out during the recruitment period, from January to June 2022.
The dependent variable was the risk of female sexual dysfunction (RFSD) measured with the female sexual function index (FSFI) developed by Rosen et al. in 2000 and translated into Spanish in 200421. This instrument is free and available online22. It consists of 19 questions covering 6 sexual domains (desire, arousal, lubrication, orgasm, satisfaction, and pain), each with 5 to 6 response options. The score for each domain is multiplied by a coefficient and summed to obtain the total score, which ranges from 2 to 36 points. The average score per domain and the total score were calculated, with a lower score being an indicator of higher risk of RFSD. In addition, a categorization of the variable was established considering a score less than or equal to 26 points as a present risk of sexual dysfunction23. In 2020 the validation of the FSFI was published in a sample of Colombian women, obtaining a sensitivity of 87.7%, a specificity of 73.9% and an area under the curve of 85.9%24.
The independent variable, QWL, was measured with the professional quality of life questionnaire (CVP-35), based on the demand control model formulated by Karasek25, validated, and adapted to Spanish by Cabezas26, which is freely available. This questionnaire consists of 35 questions grouped into 3 categories: direct support (13 questions), intrinsic motivation (9 questions) and workload (11 questions), in addition to including two questions outside the aforementioned categories relating to overall quality of work life and the ability to disconnect from work. Each question was rated on a Likert-type scale from 1 to 1026. The final score was the average obtained in each dimension. For the first two dimensions, it was considered that the higher the score, the better the QWL, while for the workload dimension, the higher the score, the lower the QWL. Previous studies in the Spanish population have shown that the internal consistency of each dimension is acceptable (Cronbach's α between 0.7)27
Sociodemographic data were collected including age, marital status (single, married, cohabiting, widowed, divorced/separated), and number of children. In addition, medical history was collected, such as harmful habits (alcohol, tobacco), atherosclerotic cardiovascular diseases such as diabetes or arterial hypertension (AHT), and nutritional status was assessed through body mass index (BMI) according to the World Health Organization (WHO) classification6. Descriptive data were also collected on the work component, including the services in which they worked (adult outpatient clinic, child outpatient clinic, adult hospitalization, child hospitalization, emergency and critical care, recovery, and sterilization center), average salary, number of shifts per month, hours of work per day and number of institutions in which they worked.
The data were compiled in a collection matrix in the Microsoft Excel program and the double digitization technique was used for quality control. Statistical analysis was performed using STATA version 15 and no missing values were considered in any of the analyses. Numerical variables were summarized by median and interquartile range, while categorical variables were summarized with absolute and relative frequencies. The Shapiro-Wilk statistical test was used to assess normality. The association of numerical variables in two groups was estimated using the Mann Whitney U test, while the Fisher exact test was used for categorical variables. The strength of association between QWL and DSF risk was assessed using Poisson-type generalized linear models with robust variance to calculate crude (cPR) and adjusted (aPR) prevalence ratios. A model was constructed that included the associated variables in the bivariate analysis as well as some potential theoretical confounders such as age, alcohol, smoking, comorbidities, and obesity. A value of p<0.05 with a 95% confidence interval was considered significant.
The study was approved by the Institutional Research Ethics Committee of the University (CIEI-Científica) with official letter number 1872020-PREB15; the confidentiality of the participants was maintained using a system of codification of personal data.
Results
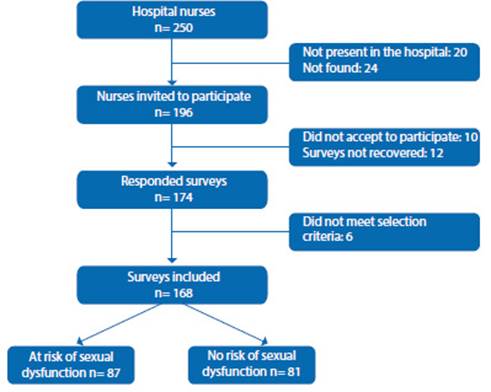
Data from 168 nurses who met the established selection criteria were analyzed (Figure 1). Univariate analysis found that the median age was 37 years and 40.5% (n=68) were single. In addition, 67.5% of the nurses reported consuming alcohol at least 1 time per month. In terms of QWL, a mean of 6.19 was obtained for the direct support dimension, 5.86 for the workload dimension, and 7.77 for the intrinsic motivation dimension. RSFD was present in 81 of the 168 nurses (see Tables 1 and 2).
Table 1 Sociodemographic characTeriSTicS of nurSeS according To riSk of Sexual dySfuncTion* (n=168).

X=mean, SD=standard deviation, p50=median, IQR=interquartile range.
a=Mann Whitney U test, b=Fisher's exact test.
*Risk of sexual dysfunction was assessed with the Rosen test: with risk of sexual
dysfunction <= 26 points, without risk of sexual dysfunction > 26 points.
HT=hypertension, DM=diabetes mellitus.
Table 2 Job characTeriSTicS of nurSeS according To riSk of Sexual dySfuncTion * (n=168).

OR=operating room, p50=median, IQR=interquartile range, QWL=quality of work life.
a=Mann Whitney U test, b=Fisher's exact test.
*Risk of sexual dysfunction was assessed with the Rosen test: with risk of sexual dysfunction<=26 points, without risk of sexual dysfunction > 26 points.
**The QWL was measured with the CVP-35: with median comparison.
Bivariate analysis found that several dimensions of the QWL were significantly associated with RSFD, including direct support (p=0.01), intrinsic motivation (p=0.003) and the work disengagement question (p=0.007). In addition, monthly income (p=0.003), marital status (p=0.001) and alcohol consumption (p=0.014) also showed a significant association with RSFD. All these results are presented in Tables 1 and 2.
To answer the research question, a Poisson regression analysis with adjusted model (for the variables age, marital status, alcohol consumption, working hours, monthly income, and the scores of each dimension) was carried out. No association was found between the QWL and RSFD dimensions (direct support PR: 1.02, CI: 0.89-1.17, p: 0.739; intrinsic motivation PR: 0.91, CI: 0.77-1.17, p: 0.272 and workload PR: 1.05, CI: 0.94-1.17, p: 0.330). However, an association was observed between age (PR: 1.02, CI: 1.00-1.03, p: 0.002), marital status (married PR: 0.51, CI: 0.330.79, p: 0.003 and cohabiting PR: 0.32, CI: 0.140.70, p: 0.004) and monthly income (PR: 0.99, CI:0.99-1.00, p: 0.019) and the dependent variable. These variables were adjusted for all the variables in the crude analysis (see Table 3).
Table 3 aSSociaTion beTween Qwl and riSk of Sexual dySfuncTion: crude and adJuSTed analySiS (n= 168).

QWL=quality of working life, PR=prevalence ratio, CI=confidence interval, HT=hypertension, DM=diabetes mellitus.
* Alcohol consumption was considered to be present if alcoholic beverages were consumed at least every two weeks.
**Adjusted: adjusted for all variables.
Discussion
In this study, no evidence was found to suggest an association between the dimensions of the QWL and RSFD adjusted for sociodemographic variables, harmful habits, comorbidities, and monthly income. In particular, low scores on the direct support dimension were not significantly associated with a higher prevalence of RSFD. However, it is important to keep in mind that this study was conducted in the context of the COVID-19 pandemic, which could have led to all research subjects having similar scores on several of the items measured by this dimension. In addition, the sample size limited only to the direct support dimension of the CVP-35 may have limited the ability to detect significant associations in other dimensions. Despite this, it was observed that older age, lack of a current partner, and low financial remuneration were significantly associated with a higher prevalence of RSFD. These findings may be of interest for the implementation of workplace health policies and programs aimed at RSFD prevention.
In our research, nurses with RSFD had lower median scores on the direct support and intrinsic motivation dimensions of the QWL score compared with those without RSFD, suggesting a possible relationship between QWL and sexual dysfunction. This is consistent with previous studies that have found a high prevalence of sexual dysfunction in nurses and other health care professionals associated with factors such as job stress, job dissatisfaction, and an unsupportive work environment. For example, Von Hippel C. et al. in 2019 reported that 50% of sexually active middle-aged nurses may have sexual dysfunction28 and Yan Y. et al. found that in them sexual dysfunction was associated with low pay9. In addition, Papaefstathiou E. et al. found that job stress was negatively related to lubrication (p=0.031) and orgasm (p=0.012) in health care workers17. These results highlight the importance of addressing the quality of work life and emotional well-being of health care professionals as a measure to prevent and treat sexual dysfunction.
The median age of the nurses was 37 years, being slightly higher in women with RSFD (39 years). We found that for each year of age the prevalence of RSFD increased by 2% (PR: 1.02, p: 0.002). The risk of sexual dysfunction increases with age, reaching 22% for women between 50-65 years and up to 47% in women between 66-74 years29. In addition, several authors have found that the frequency of sexual activity also decreases with increasing age. G. Ribes et al. mention that with increasing age, the frequency of sexuality in its genital dimension and sexual desire decreases, being more frequent in women30. Mary Ni Lochlainn BSc et al. publish data where 68% of postmenopausal women present sexual problems31. The explanation for this phenomenon could be found in the presence of medical, pharmacological, and biological factors. In women from middle age onwards, menopause and climacteric age produce changes in the adequate lubrication of the vaginal canal, decreasing sexual interest32.
Regarding the marital status of the nurses in our study, we found that the most common was currently being in a couple (married and cohabiting), which was protectively associated with RSFD (married: PR 0.51 p=0.03; cohabiting PR:0.32 p: 0.004). These findings are consistent with the results of a study conducted in Cameroon, where women with a history of being married or in a relationship were found to be less likely to have FSD33. In addition, another study evaluating the prevalence of dysfunction in patients with comorbidities found that those who were widowed (p=0.314) or divorced (p= 0.824) were at higher risk of sexual dysfunction compared to those who were married (p=0.003) and cohabiting (p=0.004)34. It is possible that this is due more to feelings and type of relationship than to the frequency of sexual intercourse, since sexual arousal is a consequence of desire, and the latter has a relationship with emotional intimacy as a motivator of sexual response35.
In the present study, we found that the median monthly income was 4,000 soles for women without RSFD and 3,500 soles for women with RSFD. A significant inverse association was observed between RSFD and monthly economic income (PR: 0.99, p: 0.019), i.e., for every one sol increase in salary, RSFD decreased by 1%. Similar findings were published in a study conducted in China, where participants with a salary higher than 5,000 yuan/ month did not present RSFD compared to those with a salary lower than 3,000 yuan/month who showed a higher RSFD (OR = 1.820, CI95% = 1.265 to 2.618)8. In addition, another study conducted in Ecuador also found that economic position associated with low income increased RSFD36 as well as symptom severity by age.
Our study has certain limitations. Since it is a cross-sectional study, we have not been able to evaluate the variable of temporality and, therefore, we can only show associations, but not causality. Given that there are no previous studies on this topic in Latin America, we believe that this work represents a first approximation to the phenomenon. An accurate diagnosis of sexual dysfunction would require a good clinical history including medical and sexual history, as well as a physical examination and, if necessary, laboratory tests. However, the Rosen test tool has a high sensitivity (87.7%) and specificity (73.9%)24, has been validated in many countries around the world and is accepted for the screening of this health problem. Regarding the tool used to assess CVP, it has demonstrated acceptable internal consistency, although we have not found previous publications reporting its sensitivity and/or specificity results.
Although psychological variables (stress, anxiety, depression)12 have been demonstrated as causes of sexual dysfunction, we did not include them in our study because adding more questions to our data collection instrument would have increased the rejection rate. The sample size was calculated for only one dimension of the CVP questionnaire (the direct support dimension) because of its feasibility, which limits the generalizability of the results. In addition, the use of non-probability convenience sampling means that the population studied is not representative. Despite these limitations, we believe that the research question is interesting and that the results of RFSD prevalence are relevant from a public health point of view.
The main strength of our study lies in having identified a high prevalence of female sexual dysfunction, which is an easily identifiable health problem through screening and is treatable. Moreover, its prevalence is expected to in-crease with age, reaching an estimated 43% in the 40-49 age group37. We believe that these results can improve health strategies to prevent and identify sexuality-related problems in health personnel.
Conclusions and recommendations
After performing the analysis of the data obtained, we can conclude that no significant association was found between the different dimensions of quality of work life (QWL) and work-related sexual dysfunction (WRSD), when adjusting for possible confounding factors. The direct support dimension, although it obtained low scores, did not have a significant impact on the prevalence of RSFD. In addition, it is important to note that due to the context of the COVID-19 pandemic, several of the items in this dimension obtained similar scores. It is possible that the limitation of the sample size to only the direct support dimension of the CVP-35 may have influenced the lack of association in the other dimensions. On the other hand, an association was found between age, marital status, and monthly income with the dependent variable, suggesting that these variables may influence the occurrence of RSFD.
It is recommended to future researchers in the field of female sexual dysfunction (FSD) that, for a more accurate diagnosis, complete medical histories should be taken, including medical and sexual history, and physical examinations and, if necessary, laboratory tests should be performed. Likewise, it is suggested that tools with fewer questions be designed to evaluate or screen for FSD and thus reduce the rejection rate in data collection. In addition, it would be convenient to explore variables that were not explored in depth in this study, such as the presence of metabolic diseases, pregnancy, partner abuse and religion. On the other hand, it is recommended to carry out multicenter studies at the national level that include the male population in order to increase the sample size and representativeness of the sample. It is important to mention that, according to data from the Ministry of Health, only 7.8% of nurses work in Metropolitan Lima, equivalent to a total of 688 nursing professionals38. These findings point to the need to improve the sexual health care of nursing professionals and to conduct more studies in the Peruvian context.
REFERENCES
1. Portillo S, Pérez T. Disfunción sexual femenina: estudio de prevalencia en mujeres premenopáusicas. Rev Of la Soc Española Ginecol y Obstet. 2017;60(4):320-7. Available from: https://sego.es/documentos/progresos/v60-2017/n4/03_TIRSO_Trabajo_San.pdf?fbclid=IwAR3Bp3e3eN3tg7JHkLEFZVtOsiHjAgfpKhTxY9OghXWFE8dNIxwfOz33jMk [ Links ]
2. Maasoumi R, Elsous A, Hussein H, Taghizadeh Z, Baloushah S. Female sexual dysfunction among married women in the Gaza Strip: an internet-based survey. Ann Saudi Med. 2019 Oct;39(5):319-27. doi: https://doi.org/10.5144/0256-4947.2019.319 [ Links ]
3. López R, Cantellano M, Staufert J, Gómez J. Prevalence of female sexual dysfunction at a tertiary care hospital in Mexico City. Rev Mex Urol. 2018;78(3):5. doi: https://doi.org/10.24245/revmexurol.v78i3.1747 [ Links ]
4. Escajadillo N, Mezones E, Castro J, Córdova W, Blümel JE, Pérez FR, et al. Sexual Dysfunction Risk and Associated Factors in Young Peruvian University Women. J Sex Med. 2011 Jun;8(6):1701-9. doi: 10.1111/j.1743-6109.2011.02259.x [ Links ]
5. Hurtado C. Disfunción sexual relacionadocon el estrés laboral del personal de salud que trabaja en el área de Medicina Interna del Hospital IESS Ibarra 2017. 2017; Available from: http://repositorio.utn.edu.ec/handle/123456789/7580 [ Links ]
6. Kingsberg SA, Woodard T. Female sexual dysfunction: Focus on low desire. Obstet Gynecol. 2015;125(2):477-86. doi: 10.1097/AOG.0000000000000620 [ Links ]
7. Wright H, Jenks RA. Sex on the brain! Associations between sexual activity and cognitive function in older age. Age Ageing. 2016 Mar;45(2):313-7. doi: 10.1093/ageing/afv197 [ Links ]
8. Liu H, Waite LJ, Shen S, Wang DH. Is Sex Good for Your Health? A National Study on Partnered Sexuality and Cardiovascular Risk among Older Men and Women. J Health Soc Behav. 2016 Sep 6;57(3):276-96. doi: 10.1177/0022146516661597 [ Links ]
9. Yang YQ, Xu Q, Tong WJ, Gao CL, Li HM. Sexual Dysfunction among Chinese Nurses: Prevalence and Predictors. Biomed Environ Sci. 2017;30(3):229-34. doi:10.3967/bes2017.032 [ Links ]
10. Sosa O, Cheverría S, Rodriguez E. Calidad de vida profesional del personal de enfermería. Rev Enferm Inst Mex Seguro Soc. 2010;18(3):153-8. doi: 10.1590/1518-8345.1149.2713 [ Links ]
11. Mazuecos FJ. Continuing Education and Professional Life Quality of the Nursing Community of Madrid. Eur J Soc Behav Sci. 2017;18(1):15-24. doi: 10.15405/ejsbs.202 [ Links ]
12. Díaz C. Factores asociados a disfunción sexual en mujeres atendidas en un hospital nivel III-Chiclayo-Perú. Rev Chil Obs Ginecol. 2017;82(4). doi: http://dx.doi.org/10.4067/s0717-752620170004003686 [ Links ]
13. Rivera R, Lara A. Calidad de Vida Laboral del Personal de enfermería en una institución de salud privada. Coloq Panam Investig en Enfermería. 2018. doi: 10.1590/1518- 8345.1149.2713 [ Links ]
14. Stamatiou K, Margariti M, Nousi E, Mistrioti D, Lacroix R, Saridi A. Female Sexual Dysfunction (FSD) in Women Health Care Workers. Mater Socio Medica. 2016;28(3):178. doi: 10.5455/msm.2016.28.178-182 [ Links ]
15. De Rose AF, Chierigo F, Ambrosini F, Mantica G, Borghesi M, Suardi N, et al. Sexuality during COVID lockdown: a cross-sectional Italian study among hospital workers and their relatives. Int J Impot Res. 2021;33(1):131-6. doi: 10.1038/s41443-020-00393-5 [ Links ]
16. Bulut EC, Ertas K, Bulut D, Koparal MY, Çetin S. The effect of COVID-19 epidemic on the sexual function of healthcare professionals. Andrologia. 2021 Apr 13;53(3). doi: 10.1111/ and.13971 [ Links ]
17. Papaefstathiou E, Apostolopoulou A, Papaefstathiou E, Moysidis K, Hatzimouratidis K, Sarafis P. The impact of burnout and occupational stress on sexual function in both male and female individuals: a cross-sectional study. Int J Impot Res. 2020 Sep 26;32(5):510-9. doi: 10.1038/s41443-019-0170-7 [ Links ]
18. Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(5):31. doi: 10.4103/sja.SJA_543_18 [ Links ]
19. Barrios S, Catoni MI, Arechabala MC, Palma E, Ibacache Y, Richard J. Carga laboral de las enfermeras en Unidades de Hemodiálisis Crónica según dependencia y riesgo de los pacientes. Rev Med Chil. 2017 Jul;145(7):888-95. doi: 10.4067/s0034-98872017000700888 [ Links ]
20. Andrade A, Rosales C. Estudio piloto. Asociación entre la calidad de vida laboral y el riesgo de disfunción sexual en enfermeras de un hospital del Callao, Perú. 2022. doi: https://doi.org/10.6084/m9.figshare.20540445.v1 [ Links ]
21. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191- 205. doi: 10.1080/009262300278597 [ Links ]
22. Blümel J, Binfa L, Cataldo P, Carrasco A, Izaguirre H, Sarrá S. Índice de función sexual femenina: un test para evaluar la sexualidad de la mujer. Rev Chil Obstet Ginecol. 2004;69(2):7. doi: 10.4067/S0717-75262004000200006 [ Links ]
23. Valenzuela P, Contreras G, Manriquez S. Índice de función sexual en trabajadoras de la salud. Rev Chil Obstet Ginecol. 2014;79(2):92-101. doi: 10.4067/S0717-75262014000200005 [ Links ]
24. Rincón A, Parra W, Álvarez A, Peñuela C, Rosero F, Espitia F, et al. Temporal stability and clinical validation of the Spanish version of the female sexual function inventory (FSFI). Women Health. 2021 Feb 7;61(2):189-98. doi: 10.1080/03630242.2020.1819940 [ Links ]
25. Karasek R. The Political Implications of Psychosocial Work Redesign: A Model of the Psychosocial Class Structure. Int J Heal Serv. 1989 Jul 1;19(3):481-508. doi: 10.2190/66AMQ4PF-PUHK-5BT1 [ Links ]
26. Cabezas C. Síndrome de desgaste profesional, estrés laboral y calidad de vida profesional. Form Médica Contin. 1998;5:491-2. [ Links ]
27. Lizán L. Características métricas del Cuestionario de Calidad de Vida Profesional. Gac Sanit. 2004;18(6):489-489. doi: 10.1157/13069771 [ Links ]
28. Von C, Adhia A, Rosenberg S, Austin SB, Partridge A, Tamimi R. Sexual Function among Women in Midlife: Findings from the Nurses' Health Study II. Women's Heal Issues. 2019 Jul;29(4):291-8. doi: 10.1016/j.whi.2019.04.006 [ Links ]
29. Espitia FJ. Prevalencia y caracterización de las disfunciones sexuales en mujeres, en 12 ciudades colombianas, 2009- 2016. Rev Colomb Obstet Ginecol. 2018 Mar 28;69(1):9. doi: 10.18597/rcog.3035 [ Links ]
30. Ribes G, Cour F. La sexualité du couple âgé : état des lieux, prise en charge. Progrès en Urol. 2013 Jul;23(9):752-60. doi: 10.1016/j.purol.2012.10.011 [ Links ]
31. Ni M, Kenny RA. Sexual Activity and Aging. J Am Med Dir Assoc. 2013 Aug;14(8):565-72. doi: 10.1016/j.jamda.2013.01.022 [ Links ]
32. Simona JA, Davis SR, Althof SE, Chedraui P, Clayton AH, Kinsberg SA, et al. Bienestar sexual después de la menopausia: documento técnico de la Sociedad Internacional de la Menopausia. Rev Colomb Menopaus. 2018;24(4):27-47. http://www.revurologia.sld.curcurologia@infomed.sld.cuhttp//www.revurologia.sld.cu [ Links ]
33. Halle GE, Timti LF, Tanue EA, Ekukole CM, Yenshu EV. Prevalence and Associated Factors of Female Sexual Dysfunction Among Sexually Active Students of the University of Buea. Sex Med. 2021 Oct;9(5):100402. doi: 10.1016/j.esxm.2021.100402 [ Links ]
34. Asefa A, Nigussie T, Henok A, Mamo Y. Prevalence of sexual dysfunction and related factors among diabetes mellitus patients in Southwest Ethiopia. BMC Endocr Disord. 2019 Dec 18;19(1):141. doi: 10.1186/s12902-019-0473-1 [ Links ]
35. Faubion SS, Rullo JE. Sexual dysfunction in women: A practical approach. Am Fam Physician. 2015;92(4):281-8. Available from: https://www.aafp.org/pubs/afp/issues/2015/0815/p281.html [ Links ]
36. Yánez D, Castelo C, Hidalgo LA, Chedraui PA. Sexual dysfunction and related risk factors in a cohort of middle-aged Ecuadorian women. J Obstet Gynaecol (Lahore). 2006 Jan 2;26(7):682-6. doi:10.1080/01443610600914021 [ Links ]
37. López RP, Cantellano M, Staufert JR, Gómez J, Herrera JA, Preciado DA. Prevalence of female sexual dysfunction at a tertiary care hospital in Mexico City. Rev Mex Urol. 2018;78(3):169-75. doi: 10.1097/GME.0000000000001305 [ Links ]
38. Velázquez A, Grillo P, Minaya P, Nuñez M. Compendio Estadístico : Información de Recursos Humanos del Sector Salud , Perú 2013 - 2015. Available from: Minist Salud. 2015;26. http://bvs.minsa.gob.pe/local/MINSA/10896.pdf [ Links ]
Received: April 02, 2023; Accepted: June 27, 2023











 text in
text in