Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.3 Lima July/Sep. 2023 Epub Oct 16, 2023
http://dx.doi.org/10.31403/rpgo.v69i2555
Case report
Prenatal diagnosis of harlequin ichthyosis. Case report
1Doctor en Medicina Clínica. Especialista en Ginecología y Obstetricia. Servicio de Obstetricia y Ginecología, Hospital Central “Dr. Urquinaona”, Maracaibo, Venezuela.
Harlequin ichthyosis, also known as diffuse fetal keratosis, is an extremely rare and phenotypically severe hereditary skin disorder with autosomal recessive inheritance. This disease is caused by mutations in the adenosine triphosphate-binding cassette transporter protein (ABCA12) gene. Prenatal ultrasonography and genetic analysis are important for prenatal diagnosis. Prenatal ultrasonographic diagnosis is difficult, and findings include ectropion plates, an abnormal auricular pinna, a flat nose, thickened skin with an armor-like appearance, thickened lips with sustained open mouth (fish mouth) status, and flexion fixation of the extremities. These are usually found during the third trimester. Three-dimensional ultrasonography contributes to the evaluation of facial morphology. The prognosis is generally poor. Affected neonates usually do not survive beyond the first days of life. A case of prenatal diagnosis of harlequin ichthyosis is presented.
Key words: Ichthyosis; harlequin; Prenatal diagnosis; Ultrasonography; Skin pathology
INTRODUCTION
Autosomal recessive congenital ichthyoses are a group of skin disorders of genetic origin and heterogeneous phenotypes. They include harlequin ichthyosis, lamellar ichthyosis and bullous congenital ichthyosiform erythroderma1). Harlequin ichthyosis, also known as diffuse fetal keratosis, is a severe, very rare and usually fatal disorder2). Its incidence is 1 per 300,000 live births. Its inheritance pattern is autosomal recessive due to mutation of the adenosine triphosphate-binding protein A12 (ABCA12) gene, which causes alterations in lipid transport in the epidermis(3,4).
Harlequin ichthyosis is a condition with a peculiar clinical appearance, as the cutaneous alteration and accumulation of scales produce widespread hyperkeratotic plaques, whitish or dark brown in color, with deep fissures almost all over the body. Other features include ectropion, fish mouth and limb contractures(1). Ultrasonography and genetic analysis are useful tools for prenatal diagnosis(3). A case of prenatal diagnosis of harlequin ichthyosis is presented.
CASE REPORT
An 18-year-old, primigravid female patient was referred for prenatal high-risk consultation for abnormal fetal facial findings on routine fetal ultrasound at 28 weeks. The patient regularly attended prenatal consultation at her center and the pregnancy had been uncomplicated. Routine ultrasound at 12 and 20 weeks showed no fetal abnormalities. The results of noninvasive prenatal tests for Down syndrome, neural tube defects and trisomy 18 were negative. The parents were distantly related and denied a history of family genetic disorders, hereditary skin disorders or contact with pesticides and radioactive substances.
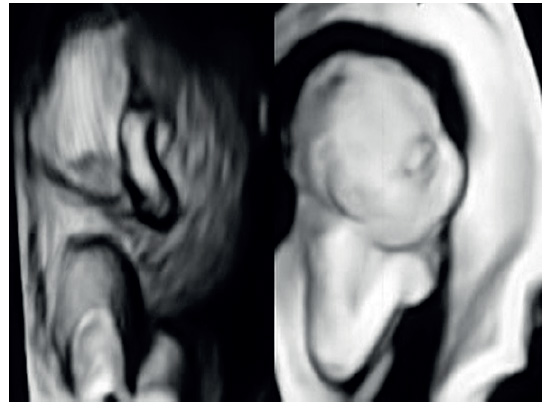
Standard ultrasound showed intrauterine pregnancy with male fetus in breech presentation and biometry corresponding to 24 weeks. Amniotic fluid volume was decreased for gestational age (below the 10th percentile) with echogenic and cloudy appearance and dense floating particles. Fetal facial features included markedly thickened upper and lower lip and fish mouthlike shape, bilateral eyelid eversion (ectropion), short nasal bone with flat nose, deformed ears, and congenital cataract. In addition, deformed spine, limb anomalies with hypoplastic and flexed fingers and toes were also observed (Figure 1). Fetal movements were scarce. Three-dimensional ultrasound imaging confirmed the abnormal findings (Figure 2). Prenatal diagnosis suggested the possibility of harlequin ichthyosis. The parents gave permission to perform amniocentesis to evaluate the fetal karyotype, which showed no chromosomal abnormalities.
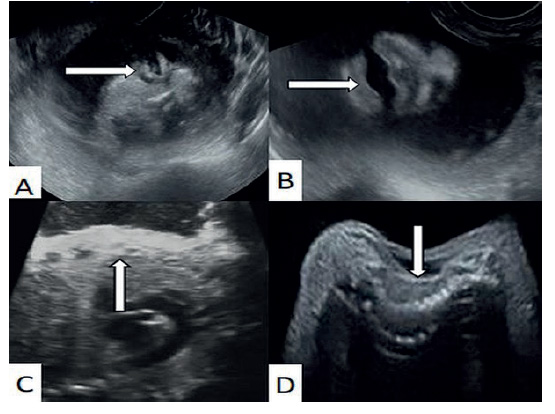
Figure 1 Ultrasound image of harlequin ichthyosis. The arrow points to A) Ectropion, B) O-shaped mouth, C) thickened skin and D) spinal deformity
At 30 weeks, the patient attended the obstetric emergency room due to uterine contractions, vaginal bleeding and decreased fetal movements. Ultrasound evaluation showed absence of fetal heart rate, for which reason uterine evacuation was decided. Stillbirth of 1,300 grams and 25 centimeters in length was obtained. On physical examination the skin was dry and thickened (consistent with hyperkeratosis), irregularly divided by deep erythematous fissures between thick, yellowish plaques, resembling thick scales that affected the entire body surface. There was also eversion of upper and lower eyelids, fish mouth, flat flared nose and abnormally flattened ears with fused lobes. The extremities were in a persistent semi-flexed position, with contractures in the fingers and incurved toes (Figure 3).
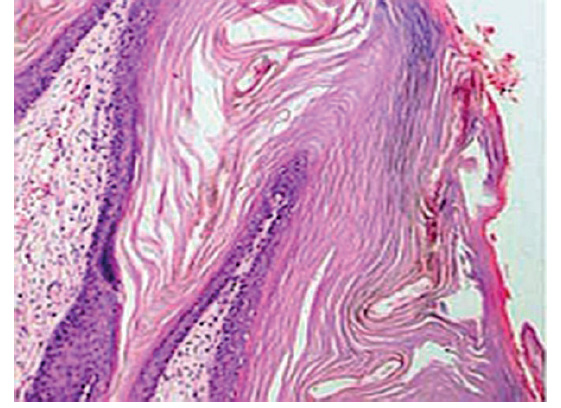
A skin sample was taken from the thorax and sent to anatomic pathology. Microscopic evaluation showed extremely thick stratum corneum, indicative of hyperkeratosis, with sparse skeletal muscle cells in dermis and subcutaneous cellular tissue (Figure 4). DNA sequencing revealed the homozygous ABCA12 variant indicative of autosomal recessive congenital ichthyosis. All findings were compatible with a diagnosis of harlequin ichthyosis.
DISCUSSION
Harlequin ichthyosis is a form of severe genodermatosis characterized by hyperkeratosis and desquamation of the epidermis(5). Its estimated incidence is 1 case per 300,000 births, without sexual predisposition, with autosomal recessive floating in the amniotic fluid (snowflake sign)(6). Ultrasound diagnosis can usually be made with certainty in the third trimester, because skin keratinization begins at 22-24 weeks of gestation. Three-dimensional ultrasonography contributes to the evaluation of facial morphology. However, it does not replace two-dimensional ultrasonography3).
DNA sequencing analysis in cases of harlequin ichthyosis is reliable and conclusive4). Diagnosis is based on identifying ABCA12 mutations(1). The protein is a member of the superfamily of ATP-dependent transporters, which bind and hydrolyze various molecules across membranes or vesicles8). This protein is present in lamellar granules of keratinocytes that regulate lipid trafficking9). The diagnosis can be confirmed by chorionic villus sampling or amniotic fluid sampling10). In patients with a family history, fetoscopy with skin biopsy and ultrastructural examination of amniotic fluid cells may be useful, although it is not currently recommended due to advances in non-invasive tests such as ultrasound(11).
The main differential diagnosis of harlequin ichthyosis in the prenatal period is Neu-Laxova syndrome. Fish mouth, absence of microcephaly and lack of edema are typical of harlequin ichthyosis, while cataracts and short umbilical cord are characteristic of Neu-Laxova syndrome11). On the other hand, fetal harlequin ichthyosis can be confused with fetal macroglossia and fetal congenital tumor-like fetal angioma12). However, macroglossia is always associated with genetic disorders such as Down syndrome and Beckwith-Wiedemann syndrome13). The thickened tongue in fetal congenital hemangioma usually shows increased blood flow on color Doppler(14).
Differential diagnoses in neonates include arthrogryposis, aplasia cutis, Gaucher disease, Sjogren-Larsson syndrome, Conradi-Hunermann-Happle syndrome and trichothiodystrophy(15). Severe cases can easily be misdiagnosed as epidermolysis bullosa or syndromic ichthyosis(9).
Those neonates with harlequin ichthyosis have a distinctive clinical appearance, with thickened, whitish to yellowish, armor-like skin, with fissures dividing the skin into polygonal or diamond-shaped sections and reddish cracks all over the body(7). This is accompanied by ectropion and a persistently open, round mouth. There is no definitive treatment for this condition. The prognosis is poor and the likelihood of neonatal death is high, despite supportive medical treatment. Most deaths occur shortly after delivery due to infections, heat loss, dehydration, electrolyte disturbances or respiratory distress3).
In conclusion, harlequin ichthyosis is an autosomal recessive genetic disorder, rare and usually fatal in the first days of life. Prenatal genetic diagnosis should be advised for couples with previously affected children. Characteristic features on prenatal ultrasound tend to appear late, so evaluations should be repeated in the third trimester, even when the second trimester anatomic examination is normal.
REFERENCES
1. Weledji EP. An overview of gastroduodenal perforation. Front Surg. 2020;7:573901. doi: 10.3389/fsurg.2020.573901 [ Links ]
2. Laila B, Vinciane L, Michael V, Patrick F, Awada A, Maria GG, et al. Diagnosis, pathophysiology, and treatment of SIRT-induced gastroduodenal ulcers: A systematic literature review. Surg Oncol. 2020;35:520-6. doi: 10.1016/j.suronc.2020.10.014 [ Links ]
3. Shirazi M, Zaban MT, Gummadi S, Ghaemi M. Peptic ulcer perforation after cesarean section; case series and literature review. BMC Surg. 2020;20(1):110. doi: 10.1186/s12893-020-00732-9 [ Links ]
4. Engemise S, Oshowo A, Kyei-Mensah A. Perforated duodenal ulcer in the puerperium. Arch Gynecol Obstet. 2009;279(3):407- 10. doi: 10.1007/s00404-008-0722-4 [ Links ]
5. Søreide K, Thorsen K, Harrison EM, Bingener J, Møller MH, Ohene-Yeboah M, et al. Perforated peptic ulcer. Lancet. 2015;386(10000):1288-98. doi: 10.1016/S0140-6736(15)00276-7 [ Links ]
6. Choi YS, Heo YS, Yi JW. Clinical characteristics of primary repair for perforated peptic ulcer: 10-year experience in a single center. J Clin Med. 2021;10(8):1790. doi: 10.3390/jcm10081790 [ Links ]
7. Bojanapu S, Malani RA, Ray S, Mangla V, Mehta N, Nundy S. Duodenal perforation: Outcomes after surgical management at a tertiary care centre - a retrospective cross-sectional study. Surg Res Pract. 2020;2020:8392716. doi: 10.1155/2020/8392716 [ Links ]
8. Jidha TD, Umer KM, Beressa G, Tolossa T. Perforated duodenal ulcer in the third trimester of pregnancy, with survival of both the mother and neonate, in Ethiopia: a case report. J Med Case Rep. 2022;16(1):322. doi: 10.1186/s13256-022-03562-w [ Links ]
9. Dongo AE, Uhunmwagho O, Kesieme EB, Eluehike SU, Alufohai EF. A five-year review of perforated peptic ulcer disease in Irrua, Nigeria. Int Sch Res Notices. 2017;2017:8375398. doi: 10.1155/2017/8375398 [ Links ]
10. Ansari D, Torén W, Lindberg S, Pyrhönen HS, Andersson R. Diagnosis and management of duodenal perforations: a narrative review. Scand J Gastroenterol. 2019;54(8):939-44. doi: 10.1080/00365521.2019.1647456 [ Links ]
11. Ali AM, Mohamed AN, Mohamed YG, Kelesoglu SI. Clinical presentation and surgical management of perforated peptic ulcer in a tertiary hospital in Mogadishu, Somalia: a 5-year retrospective study. World J Emerg Surg. 2022;17(1):23. doi: 10.1186/s13017-022-00428-w [ Links ]
12. Malgras B, Placé V, Dohan A, Lo Dico R, Duron S, Soyer P, et al. Natural history of pneumoperitoneum after laparotomy: findings on multidetector-row computed tomography. World J Surg. 2017;41(1):56-63. doi: 10.1007/s00268-016-3648-1 [ Links ]
13. Häger RM, Daltveit AK, Hofoss D, Nilsen ST, Kolaas T, Øian P, Henriksen T. Complications of cesarean deliveries: rates and risk factors. Am J Obstet Gynecol. 2004;190(2):428-34. doi: 10.1016/j.ajog.2003.08.037 [ Links ]
14. Yang YJ, Bang CS, Shin SP, Park TY, Suk KT, Baik GH, et al. Clinical characteristics of peptic ulcer perforation in Korea. World J Gastroenterol. 2017;23(14):2566-74. doi: 10.3748/wjg.v23.i14.2566 [ Links ]
15. Gupta S, Alawad AA, Dacosta K, Mahmoud A, Mohammed T. Operative versus non-operative management for perforated peptic ulcer disease. Ann Med Surg (Lond). 2022;82:104643. doi: 10.1016/j.amsu.2022.104643 [ Links ]
Declaration of ethical aspects
Acknowledgement of authorship: The author declares that he/she has contributed to the idea, study design, data collection, data analysis and interpretation, critical review of the intellectual content, and final approval of the manuscript we are submitting.
Ethical responsibilities: Protection of persons. The author declares that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Confidentiality of data: The author declares that he has followed the protocols of the Hospital Central de Maracaibo on the publication of patient data. Right to privacy and informed consent: The author has obtained the informed consent of the patient and/ or subject referred to in the article. This document is in the possession of the corresponding author.
Financing: The author certifies that he/she has not received financial support, equipment, personnel or in-kind support from individuals, public and/or private institutions for the conduct of the study.
Received: March 26, 2023; Accepted: April 26, 2023











 text in
text in