Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Peruana de Ginecología y Obstetricia
On-line version ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.3 Lima July/Sep. 2023 Epub Oct 16, 2023
http://dx.doi.org/10.31403/rpgo.v69i2556
Case report
Management of fetal-fetal transfusion syndrome in COVID-19 pandemic: case report
1. Gynecologist and Obstetrician, Ayacucho Regional Hospital, Ayacucho, Peru.
2. Medical student, Faculty of Human Medicine, Universidad Peruana los Andes, Sociedad Científica de Estudiantes de Medicina Los Andes (SOCIEMLA), Huancayo, Perú.
3. Medical student, Universidad Nacional de San Cristóbal de Huamanga, Sociedad Científica Médico Estudiantil San Cristóbal (SOCIMESC), Ayacucho, Perú.
4. Specialist in Fetal Medicine and Surgery, Fetal Medicine Unit, Clínica Anglo-Americana.
The twin-to-twin transfusion syndrome (TTTS) is a potentially lethal complication that can occur in monochorionic twin pregnancies due to an imbalance in placental blood flow. Diagnosis is based on amniotic fluid discordance and classified using the Quintero staging system. The primary treatment is fetoscopic laser photocoagulation (FLP) of placental anastomoses. A successful case of FLP treatment in a monochorionic diamniotic twin pregnancy with TTTS during COVID-19 pandemic in Peru is presented.
Key words: Pregnancy; multiple; Twin-to-twin transfusion syndrome; Prenatal diagnosis; Fetoscopy; Surgery; fetal
Introduction
The frequency of monochorionic (MC) twin pregnancy is 1/250 pregnancies and represents 20% of all twin pregnancies1. In recent years there has been an increase in its incidence, so it is more common to observe obstetric and neonatal complications2. The most important complication in MC pregnancies is the twin-to-twin transfusion syndrome (TTTS), a complex condition in which there is an imbalance in the exchange of blood flow through the placental anastomoses3. This complication causes hypovolemia in one 'donor' twin and hypervolemia in the other 'recipient' generating a cascade of hormone-mediated renal and cardiovascular alterations in both twins. This can result in 80-100% perinatal mortality and 15-50% neurological morbidity in the survivors4.
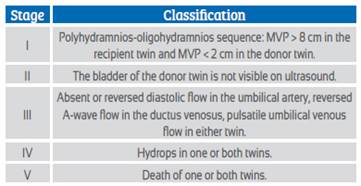
The diagnosis of TTTS requires the presence of significant amniotic fluid discordance5 where the 'donor' twin has oligohydramnios, defined as a maximum vertical pocket (MVP) of amniotic fluid less than 2 cm, and the 'recipient' twin has polyhydramnios, defined as a MVP of amniotic fluid greater than 8 cm6. Quintero staging is currently used to classify TTTS and estimate survival (Table 1)7,8. Mild cases are usually managed expectantly, while severe cases require fetoscopy and laser photoablation of the anastomosis (LPA) between 16-26 weeks of gestation9.
It is reported that with LPA treatment it is possible to obtain survival of at least one fetus in 85% of cases and of both fetuses in 50% of operated cases, being lower in Quintero stages III/IV10,11. On the other hand, there are potential complications of fetoscopy such as premature rupture of membranes, preterm labor, and bleeding2.
Early diagnosis and timely therapy, such as LPA, can significantly improve the survival and longterm outcome of twins affected by TTTS. Thus, careful prenatal surveillance is essential in biamniotic monochorionic twin pregnancies to warn of severe complications such as TTTS.
During the first months of the COVID-19 pandemic, Peru experienced a period of strict confinement in which reference hospitals in large cities were collapsed due to the large number of patients with COVID-19.
Case report
We present the clinical case of a 29-year-old female, mestizo, G2 P1001, with a history of previous cesarean section evaluated at the fetal medicine unit of the Ayacucho Regional Hospital (HRA), Peru. The 13-week ultrasound (Figure 1) showed a biamniotic monochorionic twin gestation without further observations.

Figure 1 Visualization of the insertion of the amniotic membrane forming an inverted T (‘T’ sign), which invariably indicates a biamniotic monochorionic twin gestation.
Due to the gap in appointments, the next ultrasound was performed at 21 weeks of gestation when amniotic fluid discordance was vidente with a vertical shaft of 7.0 cm and 0.8 cm for the recipient and donor twins, respectively (Figure 2ª). Donor twin 1 had growth below the 10th percentile and no bladder visualization (Figure 2b). Recipient twin 2 had growth at the 19th percentile with bladder visualization (Figure 2b). The diagnosis of Quintero stage II TTTS was proposed.

Figure 2 Ultrasound image of gestation at 21 weeks. 2a. Polyhydramnios-oligohydramnios sequence. 2b. Bladder barely visible in the donor twin and distended in the recipient twin.
In April 2020, at the beginning of the COVID-19 quarantine and with all the restrictions, referral to the Instituto Nacional Materno Perinatal (INMP) in Lima, Peru, was proposed. The referral and management were coordinated with the various specialties and logistic actors involved so that the patient could undergo treatment and counter-referral in the same transfer ambulance, since transfers for hospitalization were not accepted due to the saturation of the institutions. The surgery was performed by the INMP fetal surgery team only two hours after her arrival at the institution (Figure 3). The patient was able to return in the same ambulance two hours after the fetal surgery, and the entire recovery process was carried out at the Ayacucho Regional Hospital.

Figure 3 Endoscopic image of placental vessels, 3a before photoablation and 3b during photoablation with laser energy.
The patient evolved favorably after the procedure with amniotic fluid vertical pockets of 38 and 35 mm, respectively, and cervicometry of 17 mm.
Forty days after the fetoscopy, the patient was hospitalized for premature rupture of membranes. She underwent emergency cesarean section and confirmed the diagnosis of placen-tal abruption in 10%. Two live newborns of 920 g and 1,010 g were obtained that remained in the neonatal intensive care unit of the ARH for 83 days. The infants evolved favorably until the day of their discharge and were in good health at the time of writing this article.
Discussion
TTTS is a complication that affects about 10-15% of monochorionic pregnancies12. It occurs when there is predominantly unidirectional intergemellar blood flow through pathologic placental vascular anastomoses. The diagnosis of chorionicity is important and determines the prognosis of these pregnancies13. In our case, we were able to determine chorioamniocity in the first trimester allowing early diagnosis and subsequent timely treatment of TTTS.
TTTS is currently classified using the Quintero staging system. At the time of preoperative evaluation at INMP it was classified as Quintero stage III and emergency fetal surgery was performed12. LPA is the treatment of choice for severe cases before 27 weeks and has been shown to improve perinatal outcomes. It is important to keep in mind that complications may arise during the LPA procedure, such as premature rupture of membranes, recurrence of TTTS, polycythemia anemia sequence, among others12. Our patient presented preterm premature rupture of membranes resulting in severe oligohydramnios. However, both babies survived after 83 days of hospitalization with no apparent perinatal sequelae at discharge. They are currently two years old and the mother reports that in the pediatric controls the development shown has been adequate with no observations or need for referral to another specialty.
TTTS is an obstetric emergency in which both fetuses require immediate attention and treatment which should not be deferred due to dis tance or transportation problems. The health system must guarantee the correct referral to centers with diagnostic and therapeutic capacity and medical teams with proven experience. That is the important reason to communicate this case which occurred in a very adverse scenario in the country. At a time when all resources were destined to COVID-19 and when no cases were being referred for fetal surgery, it was possible to coordinate a referral and counter-referral that resulted in the benefit of the patient and her twins, in addition to strengthening fetal surgery with excellence in the country13.
In conclusion, twin-to twin transfusion syndrome is an important complication in monochorionic twin pregnancies where early and timely diagnosis is the mainstay of management. Timely referral to a center with resolution capacity for fetoscopy has a great impact on the reduction of perinatal mortality due to this complication.
REFERENCES
1. E G, Ju O, Jm M. A systematic approach to the differential diagnosis and management of the complications of monochorionic twin pregnancies. Fetal Diagn Ther [Internet]. 2012;32(3). doi: https://doi.org/10.1159/000342751 [ Links ]
2. Pandya VM, Stirnemann J, Colmant C, Ville Y. Current Practice and Protocols: Endoscopic Laser Therapy for Twin-Twin Transfusion Syndrome. Matern-Fetal Med [Internet]. 2020;02(01):34- 47. doi: https://doi.org/10.1097/FM9.0000000000000035 [ Links ]
3. Molina-Giraldo S, Hincapié-Porras C. Cirugía fetal láser en síndrome de transfusión feto feto y restricción selectiva del crecimiento intrauterino. Rev Peru Ginecol Obstet [Internet]. 2018;64(4):587-98. doi: https://doi.org/10.31403/rpgo.v64i2128 [ Links ]
4. Djaafri F, Stirnemann J, Mediouni I, Colmant C, Ville Y. Twin-twin transfusion syndrome - What we have learned from clinical trials. Semin Fetal Neonatal Med. 2017; 22(6):367-75. doi: https://doi.org/10.1016/j.siny.2017.08.005 [ Links ]
5. Sueters M, Oepkes D. Diagnosis of twin-to-twin transfusion syndrome, selective fetal growth restriction, twin anaemia- polycythaemia sequence, and twin reversed arterial perfusion sequence. Best Pract Res Clin Obstet Gynaecol [Internet]. 2014;28(2):215-26. doi: https://doi.org/10.1016/j.bpobgyn.2013.12.002 [ Links ]
6. Khalil A, Rodgers M, Baschat A, Bhide A, Gratacos E, Hecher K, et al. ISUOG Practice Guidelines: role of ultrasound in twin pregnancy. Ultrasound Obstet Gynecol. 2016;47(2):247-63. doi: https://doi.org/10.1002/uog.15821 [ Links ]
7. Quintero RA, Dickinson JE, Morales WJ, Bornick PW, Bermúdez C, Cincotta R, et al. Stage-based treatment of twin-twin transfusion syndrome. Am J Obstet Gynecol. 2003;188(5):1333-40. doi: https://doi.org/10.1067/mob.2003.292 [ Links ]
8. Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK, Kruger M. Staging of Twin-Twin Transfusion Syndrome. J Perinatol [Internet]. 1999;19(8):550-5. doi: https://doi.org/10.1038/sj.jp.7200292 [ Links ]
9. Gratacós E. Terapia y cirugía fetal: indicaciones y resultados actuales. Prog Obstet Ginecol [Internet]. 2008;51(9):541-58. doi: https://doi.org/10.1016/S0304-5013(08)72328-8 [ Links ]
10. Di Mascio D, Khalil A, D'Amico A, Buca D, Benedetti Panici P, Flacco ME, et al. Outcome of twin-twin transfusion syndrome according to Quintero stage of disease: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2020;56(6):811-20. doi: https://doi.org/10.1002/uog.22054 [ Links ]
11. Lewi L, Deprest J, Hecher K. The vascular anastomoses in monochorionic twin pregnancies and their clinical consequences. Am J Obstet Gynecol [Internet]. 2013;208(1):19-30. doi: https://doi.org/10.1016/j.ajog.2012.09.025 [ Links ]
12. Fichera A, Azzaretto VV, Fratelli N, Mancino S, Marella D, Negri B, Fetoscopic laser ablation therapy in monochorionic diamniotic twin pregnancies with twin-to-twin transfusion syndrome treated at a single centre over 10 years: a retrospective study. J Perinat Med. 2021 Sep 15;50(1):34-41. https://doi.org/10.1515/ jpm-2021-0058 [ Links ]
13. Ventura Laveriano W, Novoa Reyes R, Castillo Urquiaga W, Zárate Girao M, Huertas Tacchino E, Nazario Redondo C, et al. Fetoscopia y fotocoagulación láser en el manejo del síndrome de transfusión feto fetal: serie de los primeros casos tratados en el Perú. Rev Peru Ginecol Obstet [Internet]. 2019;65(2):197-201. DOI: https://doi.org/10.31403/rpgo.v65i2174 [ Links ]
6The present publication is original and has not been previously published in another institution and/or scientific journal. The study has been approved by the institutional ethics committee and had the permission of the institution.
Funding: The authors certifythat we have not received specific financial support, equipment or materials from individuals, public and/or private institutions for the conduct of this study.
Received: May 29, 2023; Accepted: August 18, 2023











 text in
text in