Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista Peruana de Ginecología y Obstetricia
versión On-line ISSN 2304-5132
Rev. peru. ginecol. obstet. vol.69 no.3 Lima jul./set. 2023 Epub 16-Oct-2023
http://dx.doi.org/10.31403/rpgo.v69i2557
Case report
Prenatal diagnosis of vasa previa type 3, a case report
1Hospital Nacional Daniel Alcides Carrión, Callao, Perú
2Clinica Santa Isabel, Lima, Perú
3Clinica Delgado- AUNA, Lima, Perú
Vasa previa is a rare condition in which the umbilical vessels are found to run in the vicinity of the internal cervical os. It is usually associated with velamentous insertion of the umbilical cord, placenta succenturiata, low placenta insertion and in vitro fertilization. Early diagnosis in the second trimester has important perinatal implications because it reduces neonatal mortality. We present the first case of prenatal diagnosis of vasa previa type 3 (a little known variant) reported in Peru in a pregnant woman with placenta previa and undiagnosed until the third trimester.
Key words: Vasa previa; Doppler color; Prenatal diagnosis
INTRODUCTION
Vasa previa (VP) is described as the presence of umbilical vessels running over the ovular membranes below the lower segment of the uterus and in the vicinity of the cervix up to 2 centimeters from the internal cervical os (ICO). The prevalence is variable but is estimated at 1 in 2,000-5,000 live births1). In cases associated with velamentous insertion of the umbilical cord, placenta succenturiata or low-lying placenta, the prevalence increases and may be as high as 1 in 50 cases. As the umbilical vessels are devoid of Wharton's jelly protection, they are susceptible to compression. Thus, vasa previa is associated with poor perinatal outcome when not diagnosed prenatally.
We present the first case of prenatal diagnosis of VP type 3 reported in Peru, which due to the morphology of the aberrant vessel that forms the vasa previa is little suspected and frequently overlooked in prenatal diagnosis.
CASE REPORT
A 34-year-old multiparous pregnant woman with no previous cesarean section came to the emergency room complaining of uterine contractions. She had suspected placenta previa.
Ultrasound showed active gestation of 34 weeks 6 days with a fetal weight of 2,110 grams. Marginal insertion of the umbilical cord and presence of umbilical vessels in front of the fetal presentation were found.
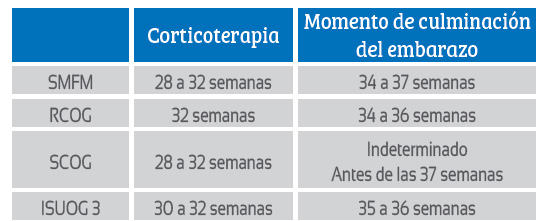
Transvaginal ultrasound was performed, finding the inferior placental border 10 mm from the ICO (Figure 1) and umbilical vessels running along the membrane 3 mm from the ICO (Figure 2). 3D Doppler reconstruction was performed to assess the vascular anatomy, finding an artery and a vein described as a loop close to the ICO related to marginal insertion of the cord (Figure 3). The diagnosis of vasa previa and placenta previa was proposed.
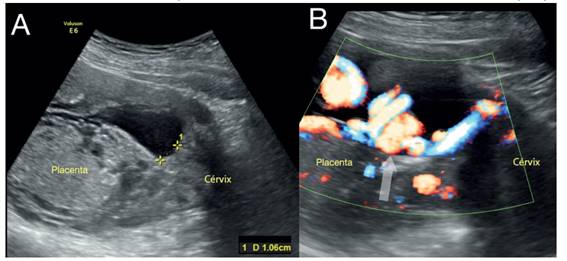
Figure 1 A: Posteriorly inserted placenta, 10 mm from the ICO. B: Marginal insertion of the cord is observed using Doppler (arrow).
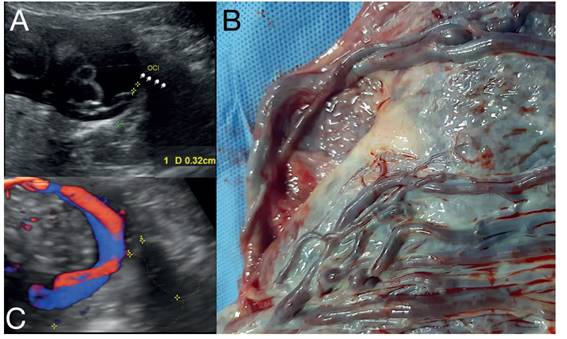
Figure 2 A: The umbilical vessels can be seen in the vicinity of the internal cervical os; the marginal insertion of the cord is also visible. B: Image of the placenta showing the course of two vessels (artery and vein) through the membrane. C: Doppler image showing two vessels (artery and vein) in the vicinity of the cervix, which is shown delineated.
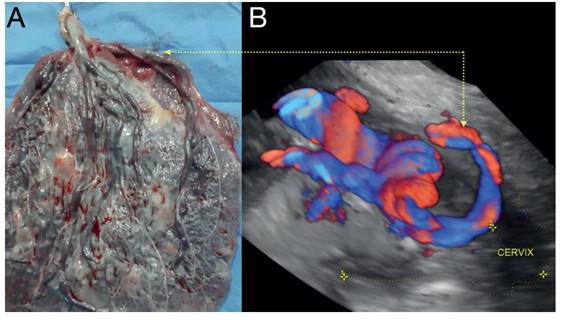
Figure 3 A: Macroscopy of the placenta clearly showing the umbilical vessels (artery and vein) forming a boomerang up to the marginal insertion of the cord and passing through the amniotic membrane. B: 3D Doppler reconstruction showing the loop of umbilical vessels in the vicinity of the cervix.
The patient underwent emergency cesarean section for having gone into labor, obtaining a newborn with Apgar 9-9 and good perinatal outcome until 6 months of follow-up.
The macroscopic study of the placenta confirmed vasa previa, showing marginal insertion of the cord and an aberrant vessel running along the membrane outside the placental border. It was therefore classified as VP type 3 (Figures 2B and 3A).
DISCUSSION
Vasa previa (VP) is defined as the presence of fetal vessels that cross the chorioamniotic membrane and are less than 2 cm from the internal cervical os. The etiology is controversial, and two theories have been proposed regarding velamentous insertion of the umbilical cord. The first one mentions that, in spite of an adequate implantation of the umbilical vessels in the decidua basalis, with fetal growth it becomes inadequate, producing regression in the chorion frondosum surrounding the insertion. The second proposes that the velamentous insertion modifies the decidua basalis resulting in the vessels extending to the margin of the placenta2).
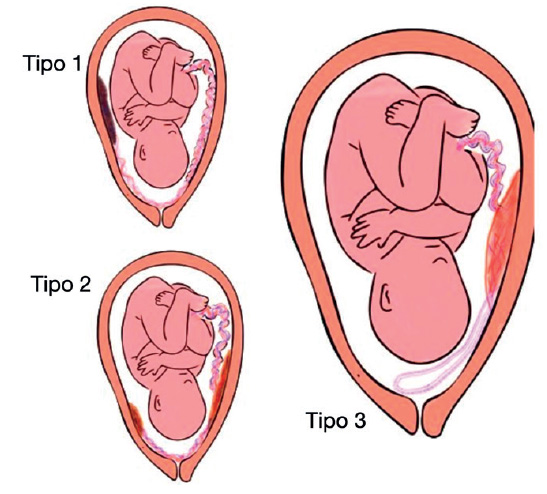
The most accepted classification is defined by the macroscopic findings of the placenta in 3 types3)(Figure 4): Type 1, in which the umbilical vessels cross from the velamentous insertion of the cord. Type 2, in which the crossing umbilical vessels connect the lobes of a bilobed or succenturiata placenta. Type 3, when the crossing vessels describe a boomerang orbit without velamentous insertion of the cord or lobulated placenta (description made by Suekane4) in two cases in 2020), as we can see in the case presented (Figures 2 and 3). Figure 3. A: Macroscopy of the placenta clearly showing the umbilical vessels (artery and vein) forming a boomerang up to the marginal insertion of the cord and passing through the amniotic membrane. B: 3D Doppler reconstruction showing the loop of umbilical vessels in the vicinity of the cervix.
The search and diagnosis of VP by ultrasound is recommended by identifying the insertion of the umbilical cord (search for velamentous or marginal insertion), ruling out the presence of accessory lobes in the placenta and performing a transvaginal ultrasound to search for placental vessels in the vicinity of the ICO. In addition, the use of Doppler to delimit the path of the vessels and to be able to differentiate them from maternal vessels that have flow waves with different heart rate. Also, 3D reconstruction is very useful for the precision of the anatomy of the vessels and their relationship with the ICO (Figure 3)(3,5,6).
The published ultrasound detection rate ranges from 53-100%, depending largely on the year the study was performed, whether it was retrospective and whether transvaginal or Doppler ultrasound was used in the search for cord insertion7). The American Institute of Ultrasound (AIU) in Medicine (AIUM) and the American College of Obstetrics and Gynecology (ACOG) recommend the evaluation of umbilical cord insertion (velamentous or marginal) in the second trimester of pregnancy, by abdominal and transvaginal ultrasound using color Doppler, suggesting that the corresponding follow-up be carried out at 32 weeks of gestation in case of suspicion8,9).
The risk factors associated with the presence of VP described in the literature are: velamentous or marginal insertion of the cord, bilobed or succenturiate placenta and in vitro fertilization (prevalence of 1 in 260)(8). However, up to 11% of cases have no identifiable risk factors5). In the case presented, the factors were marginal insertion and placenta previa (Figure 1). The search for VP as a strategy has been shown to be cost-effective in IVF pregnancies and when in the second trimester signs of suspicion such as placenta previa, low insertion placenta, velamentous or marginal cord insertion and bilobed or succenturiata placenta were found10). Type 3 VP has been recently described (2020). Kamijo's series8 includes this classification and covers a 10-year retrospective analysis of 8,723 deliveries. He found 14 cases with VP, of which 9 were classified as type 1 and 5 as type 3 (36%). In these, the aberrant vessel involved in VP was single (artery or vein). The risk factors identified were in 3 cases placenta with low insertion in the second trimester and in 2 cases in in vitro fertilization. The term of gestation was between 35-37 weeks, except in one case at 33 weeks due to vaginal bleeding.
Regarding management, Table 1 shows the different recommendations of the different societies, in which there is no consensus on the moment when gestational termination should be performed (there is consensus that it should be via the abdominal route), the moment of corticotherapy and the need for prior hospitalization for observation until the end of gestation9,11).
The prognosis of VP is determined by timely diagnosis by ultrasound. In Zhang's meta-analysis12) with 21 included studies, the risk for fetal death and neonatal death was much higher (25 times higher) in cases where there was no prenatal diagnosis (1/226 vs. 32/118 for fetal death and 1/226 vs. 25/118 for neonatal death). Likewise, intact neonatal survival reaches 97% in cases with prenatal diagnosis. In contrast, the morbidity generated by peripartum hypoxia can be up to 50 times higher in cases without prenatal diagnosis.
In conclusion, the search for vasa previa in patients presenting risk factors is fully justified given the implications for perinatal prognosis. For this purpose, the use of transvaginal ultrasound and Doppler are the best choice in the second trimester.
REFERENCES
1. Gagnon R. No. 231-Guidelines for the Management of Vasa Previa. J Obstet Gynaecol Can. 2017;39(10):e415-e421. doi: 10.1016/j.jogc.2017.08.016 [ Links ]
2. Oyelese Y, Smulian JC. Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol. 2006;107(4):927-41. doi: 10.1097/01.AOG.0000207559.15715.9 [ Links ]
3. Ranzini AC, Oyelese Y. How to screen for vasa previa. Ultrasound Obstet Gynecol. 2021;57(5):720-5. doi: 10.1002/uog.23520 [ Links ]
4. Suekane T, Tachibana D, Pooh RK, Misugi T, Koyama M. Type-3 vasa previa: normal umbilical cord insertion cannot exclude vasa previa in cases with abnormal placental location. Ultrasound Obstet Gynecol. 2020;55(4):556-7. doi: 10.1002/uog.20347 [ Links ]
5. Oyelese Y, Chavez MR, Yeo L, Giannina G, Kontopoulos EV, Smulian JC, et al. Three-dimensional sonographic diagnosis of vasa previa. Ultrasound Obstet Gynecol. 2004;24(2):211-5. doi: 10.1002/uog.1097 [ Links ]
6. Lo A, Berman S, Chaiworapongsa T, Asaad R, Gonik B. Vasa previa with pulsed wave Doppler depicting maternal heart rate. Ultrasound Obstet Gynecol. 2020;56(3):460-1. doi: 10.1002/uog.21910 [ Links ]
7. Ruiter L, Kok N, Limpens J, Derks JB, de Graaf IM, Mol BW, Pajkrt E. Systematic review of accuracy of ultrasound in the diagnosis of vasa previa. Ultrasound Obstet Gynecol. 2015;45(5):516-22. doi: 10.1002/uog.14752 [ Links ]
8. Kamijo K, Miyamoto T, Ando H, Tanaka Y, Kikuchi N, Shinagawa M, et al. Clinical characteristics of a novel »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ Type 3 »,» ®,® §,§ ­, ¹,¹ ²,² ³,³ ß,ß Þ,Þ þ,þ ×,× Ú,Ú ú,ú Û,Û û,û Ù,Ù ù,ù ¨,¨ Ü,Ü ü,ü Ý,Ý ý,ý ¥,¥ ÿ,ÿ ¶,¶ vasa previa: case series at a single center. J Matern Fetal Neonatal Med. 2021;9:1-7. doi: 10.1080/14767058.2021.1960975 [ Links ]
9. Society of Maternal-Fetal (SMFM) Publications Committee, Sinkey RG, Odibo AO, Dashe JS. #37: Diagnosis and management of vasa previa. Am J Obstet Gynecol. 2015;213(5):615-9. doi: 10.1016/j.ajog.2015.08.031 [ Links ]
10. Sinkey RG, Odibo AO. Vasa previa screening strategies: decision and cost-effectiveness analysis. Ultrasound Obstet Gynecol. 2018;52(4):522-9. doi: 10.1002/uog.19098 [ Links ]
11. Tsakiridis I, Mamopoulos A, Athanasiadis A, Dagklis T. Diagnosis and Management of Vasa Previa: A Comparison of 4 National Guidelines. Obstet Gynecol Surv. 2019;74(7):436-42. doi: 10.1097/OGX.0000000000000692 [ Links ]
12. Zhang W, Geris S, Al-Emara N, Ramadan G, Sotiriadis A, Akolekar R. Perinatal outcome of pregnancies with prenatal diagnosis of vasa previa: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2021;57(5):710-719. doi: 10.1002/uog.22166 [ Links ]
Received: June 20, 2023; Accepted: September 05, 2023











 texto en
texto en