Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de la Facultad de Medicina Humana
Print version ISSN 1814-5469On-line version ISSN 2308-0531
Rev. Fac. Med. Hum. vol.20 no.1 Lima Jan./Mar. 2020
http://dx.doi.org/10.25176/rfmh.v20i1.2551
Articulo original
Treatment of Ota nevus with Q-switched Alexandrita laser of 755 nm
3Peruvian Institute of Cellular Engineering and Tissue Manufacturing - INGECEL. Lima, Peru.
4Research Institute in Biomedical Sciences, Faculty of Medicine - Universidad Ricardo Palma. Lima, Peru.
Introduction:
Ota nevus is a benign dermal melanocytic hamartoma with a macular appearance, poorly defined and in a gray-black patch that generally affects the first and second branches of the trigeminal unilaterally.
Objective:
To evaluate the efficacy, safety and adverse events caused by the application of 755 nm Alexandrite laser for the treatment of Ota nevus.
Methods:
Case series of 10 phototype IV patients with unilateral Ota Nevus treated between January 2017 and December 2018, which were treated with this light energy and with defined parameters.
Results:
The mean age was 29 years. The patients who completed the treatment did not show repigmentation in the treated lesion and the satisfaction index was acceptable. It was observed that the average of sessions to obtain favorable results varied between 8 and 10 applications. Among the most important adverse effects, post-inflammatory hyperpigmentation and the removal of the superficial layer of the post laser skin stand out. All were controlled without leaving permanent residual lesions.
Conclusion:
The 755 nm Alexandrite Q-switched laser is an effective technology to achieve a high degree of depigmentation in the treatment of Ota nevus and can be considered as a first-line treatment for the management of this pathology.
Keywords: laser 755 nm; Ota nevus, Q-switched; Congenital pigmentary lesions; Congenital facial nevus (source: MeSH NLM).
INTRODUCTION
The Ota Nevus (ON) is named about the Japanese dermatologist Ota, who was the first to describe the entity in 1936.1It is a benign dermal melanocytic hamartoma that occurs at the facial level, with periorbital predominance, frontal, temporal, nose and ocular area being able to compromise sclera, conjunctiva, cornea and even retina.2It is a macular aspect formation poorly delimited in black-gray patch, which affects the first and second nerve branches of the trigeminal.3Approximately 90% of the ON cases are unilateral.
It manifests from childhood as a hyperpigmentation that progressively increases in size and intensity of color until puberty.4Although they may be present in 1% of neonates, they usually start their appearance from 6-12 months and increase in number and size until around 25 years.5
ON can occur in all races, but is more common in Asians,6affects 0.5% of the world's population and its presentation is higher in women with a frequency of 1 to 5.7
The pathogenesis of this dermal melanocytosis is unknown. Different theories have been proposed, but none is entirely satisfactory. Hori Y. and Cols. 8since 1984, proposed that its origin could be attributed to two possible mechanisms: to the descent or migration of melanocytes from the epidermis or the hair bulb to the dermis or the reactivation of melanocytes pre-existing dermal, triggered by inflammatory or degenerative mechanisms. It has also been proposed that there could be a hormonal influence; for example, the appearance of ON is more typical at puberty.9Melanocytes are governed by hormones produced at the level of the anterior pituitary gland, adrenal glands and ovaries in addition to the common mechanisms of their precursors. The diagnosis is made in the office. Biopsy being rarely necessary for diagnostic confirmation.10(Table 1).
Table 1. ON classification according to the size of the lesions
| CLASSIFICATION | PRESENTATION FEATURES |
|---|---|
| Type I | Small: Orbitopalpebral and / or zygomatic. |
| Type II | Intermediate: It affects the orbital, zygomatic and nasal regions. |
| Type III | Extensive: It affects the region of the first and second branches of the trigeminal nerve. |
| Type IV | Bilateral. |
Adapted from: Dermatology. Atlas, diagnosis and treatment. Mc Graw Hill 6th Ed.
Current treatments seek to improve the appearance of patients. Camouflage is an effective treatment to improve coloration and size. Cryotherapy seeks to suppress the function of melanocytes at the epide(rmal level and destroy dermal melanocytes. Skin peeling removes melanin from the epidermis and superficial dermis. One method that is currently no more indicated is microsurgery, because it creates a superficial scar.11
The laser has revolutionized the treatment of ON. To treat these lesions, specific pigment lasers have been developed, among which are: the Ruby Q-switched laser (694 nm), the Alexandrite Q-switched (755 nm), the Neodymium: Yttrium-Aluminum-Garnet (1064 nm and 532 nm), pulsed colorant laser (510 nm), copper vapor laser (578 nm). The Alexandrite Q-switched laser (755 nm) is based on selective photothermolysis that provides high energy with short duration pulses, which allow the selective destruction of melanocytes.
Golberg et al.12were the first to report the use of Q-switched Ruby for the treatment of ON. The efficacy of this treatment was then supported in a study involving 114 patients treated with this laser.13The side effects were hyperpigmentation. Because ON mostly occurs in individuals with pigmented skin, care should be taken when selecting the modality of the laser and creep to minimize injury to non-injury melanocytes.14
A comparison of the Q-switched Ruby laser; The Alexandrite Q-switched laser has longer wavelengths and is less absorbed by melanin, which prevents damage to the epidermis and allows deeper penetration.15Consequently, it can selectively remove epidermal and dermal pigmentation, which is why it is ideal for the treatment of deep lesions such as these, a reason for study.
Due to this, the objective of this study is to evaluate the efficacy, safety and adverse effects in the treatment of ON with the Q-switched 755 nm laser Alex Trivantage - Candela.
METHODS
This is a series of cases with carried out between January 2017 and December 2018 on a sample of 10 patients with an average of 29 years (from 16 to 40 years old) and with a clinical diagnosis of unilateral (ON). All of them with type IV skin photo type, treated in the skin clinic. The Alex Trivantage Candela Q-switched Alexandrite 755 nm laser was used with defined energy parameters of 6 j / cm2 and 3Hz frequency and 3mm spot. All included patients signed the informed consent that includes the use of their photographic record for scientific purposes. Likewise, the study was authorized by the institutional ethics committee. Patients treated with oral retinoids, active infections or suspicious lesions of malignancy, pregnant or lactating patients and patients who did not accept informed consent were excluded.
The photographic records were given with a Canon T3i camera under the same photographic technical parameters at the beginning of the treatment. All of them were applied topical anesthesia in the area to be treated and occluded with plastic film for 30 min. Then the laser was applied to the area of injury. Subsequently, cold packs were placed for 5 minutes and then Mupirocin cream with Betamethasone topically. As a medical prescription indicated creams with gentamicin / clotrimazole / betamethasone every 8 hours for 3 days, Bepanthen (cream): application every 8 hours for 15 days. the 4th day started Isdin Ultra 90 (photoprotector) conditional application to exposure and with reference hours 9am, 12pm and 3pm for 30 days, starting on the 4th day.
In all patients, variables such as; of lesion size, frequency and number of sessions, whether or not complete treatment, as well as side effects. To assess the outcome of the treatment, a scale was created in which the assessment of the patient and the assessment of the doctor were assessed. This scale only finally shows the assessment of the change according to the pigmentation, with which it was estimated whether the treatment was effective or not. For this, a simple qualitative table was developed for the patient and the operator, which contained the study variables and their characteristics including reducing the size of the lesion; the improvement in pigmentation; the presence of side effects (hyper or hypopigmentation) and the assessment of the lesion (depigmentation or not).
In case of presenting post-application hyperpigmentation, the topical application of a master formula of 2% kojico acid, 5% mandelic acid, Triamcinolone 0.025% for night use was recommended. If irritation occurs to this formula, he was instructed to apply cloths with cold chamomile for 3 to 5 minutes, every 6 hours, for 5 days. In cases of severe irritation, a 0.05% Betamethasone formulation was applied every 12 hours for 3 days. Once this episode was over, the use of depigmenting formulation was restarted on an inter daily basis, until the next laser session according to protocol.
RESULTS
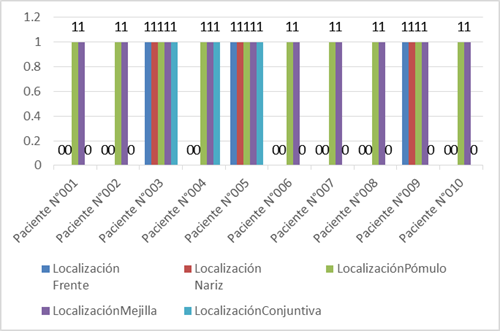
All the patients attended were female, with photo type IV, with the 20 to 30 year old group being the most representative with 6 patients. The affected areas in all treated patients were located unilaterally on the cheekbone and cheek. Three of the patients presented conjunctival and nasal involvement. (Figure 1). most patients presented commitment from two or more locations.
5 patients had a large lesion, greater than 10cm; 4 patients with a lesion of medium size <10cm and> 5cm. only 1 patient presented an injury less than 5 cm. For different reasons, different session frequencies were generated and only 4 patients respected the agreement regarding the time indicated between sessions every 30 days; 3 patients had frequency between sessions of 60 days; the rest, one attended every 45 days, pray every 90 days and the last every 120 days
6 patients successfully completed the treatment and 4 patients left it at the 7th session for various reasons, the main one being the appearance of side effects and which, according to the assessment scale, showed no improvement in their injury.
The patients who completed the treatment were those who had 8 or more sessions and it was evident that the treatment was satisfactory from the 8th session. 70% of patients had side effects, however, only 20% of this group did not complete the treatment; These patients presented frequencies of laser application every 30 days and every 120 days.(Table 2)
Table 2. Frequency of sessions, number of sessions, abandonment and side effects
| Case side | Frequency sessions (days) | Number of sessions | Complete treatment | Effects |
| 1 | 60 días | 10 | YES | YES |
| 2 | 30 días | 10 | YES | YES |
| 3 | 60 días | 8 | YES | YES |
| 4 | 120 días | 5 | NO | YES |
| 5 | 60 días | 9 | YES | NO |
| 6 | 45 días | 8 | YES | YES |
| 7 | 30 días | 6 | NO | NO |
| 8 | 30 días | 5 | NO | YES |
| 9 | 90 días | 6 | NO | NO |
| 10 | 30 días | 10 | YES | YES |
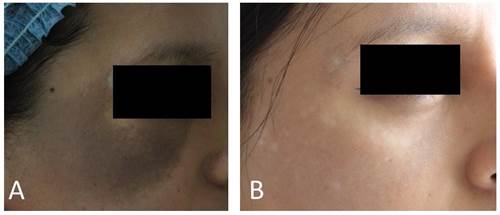
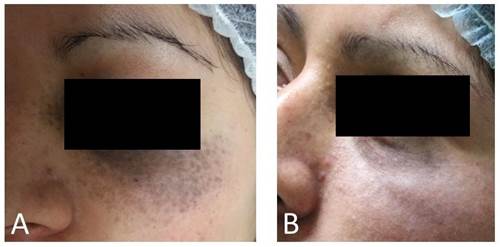
Figure 2. 22years old female. The frequency of their sessions was 60 days and they were performed 10 sessions in total. It presented side effects of hypopigmentation. He did not need depigmenting. A) Before and B) after treatment .

Figure 3. Woman 32 years old. The frequency of his sessions was 60 days and there were 8 sessions in total. It presented side effects of post inflammatory pigmentation and needed depigmenting between sessions. A) Before and B) after treatment
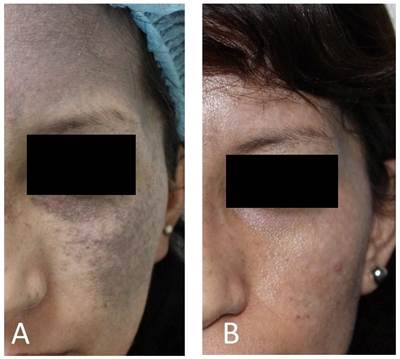
Figure 4. 29-years-old female. The frequency of their sessions was 60 days and There were 9 sessions in total. It had no side effects. A) Before and B) after treatment.
DISCUSSION
There are multiple treatments with the intention of minimizing the psychological impact on patients, but in addition to being ineffective, they can form inesthetic scars that further aggravate the problem.11The laser has revolutionized the treatment for these lesions, the Q-switched together with the concept of selective photothermolysis, which generates better long-term results. This has made it the treatment of choice for injuries such as ON16.
It is evident in this skin phototype that side effects occur easily, but it has been possible to verify that depigmented treatment areas do not re-pigment; as long as the patient takes appropriate care measures, otherwise he may have hyperpigmented lesions.
The patients who completed the treatment and followed the indications did not show repigmentation in the treated lesion, so the satisfaction rate was acceptable.
The number of sessions is relative in each patient, however, it has been shown that the average for favorable results varies between 8 and 10 sessions. The long-term result (20 months) is the same as that applied every 30 days, like the one applied every 60 days.
The important thing is that it was found that the frequency of sessions did not alter the final result of depigmentation and / or the appearance of side effects.
CONCLUSIONS
The 755 nm Alexandrite Q-switched laser applied with a minimum of 8 sessions in a span of not less than 30 days with an intensity of 6 J / cm2 was an effective therapy in cases of ON, achieving a high degree of depigmentation. Therefore, it should be considered as a first-line treatment for the management of this pathology.
REFERENCES
1. Seo H-M, Choi C-W, Kim W-S. Beneticial effects of early treatment of nevus of Ota qith low fluence 1064nm q-switched Nd:Yag láser. Dermatol Surg. 2015; 41 (I): 142-148. doi: 10.1097/DSS.0000000000000212 [ Links ]
2. Falabella R, Victoria, M. Barona, L. Fundamentos de Medicina: Dermatología, 7° Edición 2009; 420-26. Disponible en: https://es.scribd.com/book/350142962/Dermatologia-Fundamentos-de-medicina-8%C2%AA-edicion [ Links ]
3. Alcala D, Valente I. Nevos melanociticos y no melanociticos. Revisión de la literatura. Rev Cent Dermatol Pascua. 2010; 19(2): 49-58. Disponlibe en: https://www.medigraphic.com/pdfs/derma/cd-2010/cd102a.pdf [ Links ]
4. Hasson A, Navarrete-Dechent C, Nicklas C, Carreño N. Láser Q-Switched Nd:Yag 1064 nm para el tratamiento del Nevus de Ota: resultados en 22 pacientes y revisión de la literatura. Piel(Barc). 2012; 27(3): 113-17. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=3955306 [ Links ]
5. Rex J, Ferrandiz C. Nevus Melanociticos. 185-91. Disponible en: https://www.aeped.es/sites/default/files/documentos/nevus.pdf [ Links ]
6. Shah V, Bray F, Aldahan A, Mlacker S, Nouri K. Lásers and Nevus of ota: a comprenhensive review. Lásers med Sci. 2016; 31(1): 179-85. doi: 10.1007/s10103-015-1834-2 [ Links ]
7. Saracoglu S. Case Report: Treatment of Nevus of Ota with 1064 nm Q-switched Nd:Yag. Journal of tha Láser and Health Academy. 2013; 2013(2):42-5. Disponible en: https://www.laserandhealthacademy.com/media/objave/academy/priponke/42_45___case_report___saracoglu___qsw_ndyag_treatment_of_nevus_of_ota.pdf [ Links ]
8. Hori Y, Kawashima M, Oohara K, Kukita A. Acquired, bilateral nevus of Ota-like macules. J Am Acad Dermatol. 1984 Jun;10(6):961-4. https://doi.org/10.1016/s0190-9622(84)80313-8 [ Links ]
9. Stanford DG, Georgouras KE. Dermal melanocytosis: a clinical spectrum. Australas J Dermatol. 1996 Feb;37(1):19-25. https://doi.org/10.1111/j.1440-0960.1996.tb00989.x [ Links ]
10. Henry H.L. Chan, MB, FRCPG, FRCPE, Taro Kono, MD. Nevus of Ota: Clinical Aspects and Management. SKINmed .2003; 2(2): 89-98. https://doi.org/10.1111/j.1540-9740.2003.01706.x [ Links ]
11. Toshio Kobayashi MD. Microsurgical Treatment of Nevus of Ota. The Journal of Dermatologic Surgery and Oncology. 1991; 17(12): 936 - 41. doi: https://doi.org/10.1111/j.1524-4725.1991.tb01693.x [ Links ]
12. Watanabe S. Takahashi H. Treatment of nevus de Ota with Q-switched rubi laser. N Engl j Med. 1994; 331:1745-1750 https://doi.org/10.1056/NEJM199412293312604 [ Links ]
13. Chan HH, Kono T. Nevus of Ota: clinical aspects and management. Skinmed. 2003 Mar-Apr; 2(2): 89-96; quiz 97-8. https://doi.org/10.1111/j.1540-9740.2003.01706.x [ Links ]
14. Felton SJ, Al-Niaimi F, Ferguson JE, Madan V. our perspective of the treatment of naevus of ota with 1064 - 755 - and 532 nm wavelength láser. Láser Med Sci. 2013; 29(5):1745-49. https://doi.org/10.1007/s10103-013-1332-3 [ Links ]
15. Choi J, Bong J, Beom K, Soon B, Yeo U, Hun C, Hoon J, Chul Y. A retrospective analysis of the clinical efficacies of q-switched alexandrite and q-switched Nd:Yag lásers in the treatment of nevus of Ota in Korean patients. Journal of dermatological treatment. 2015; 26(3): 240-45. https://doi.org/10.3109/09546634.2014.930409 [ Links ]
16. Aurangabadkar S. QYAG5 Q-switched Nd:Yag Láser Treatment of Nevus of Ota: An Indian Study of 50 Patients. J cutan Aesthet Surg. 2008; 1(2): 80-4. https://doi.org/10.4103/0974-2077.44164 [ Links ]
Received: August 08, 2019; Accepted: November 03, 2019











 text in
text in