Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.20 no.2 Lima abr./jun 2020
http://dx.doi.org/10.25176/rfmh.v20i2.2840
Original article
Risk factors for infertility in women in a Peruvian Hospital
1Hospital Vitarte, Lima - Perú.
2Escuela de Postgrado en Gestión Pública de la Universidad Tecnológica del Perú, Lima - Perú.
Introduction:
We can define infertility as the failure to achieve pregnancy after 12 months of unprotected sex, according to the World Health Organization (WHO). Between 60 to 80 million couples annually suffer from this problem. In Peru, there are no updated reports that allow knowing these figures. In addition, few studies allow knowing the causes of this condition
Objective:
To determine the risk factors associated with infertility in female patients treated in outpatient offices in the Gynecology Service of the Vitarte Hospital, period January 2015 to April 2019.
Methods:
We conducted an observational, analytical, retrospective case-control study, considering a sample of 82 cases and 82 controls. Clinical, demographic and habits of harmful consumption factors were considered and, to measure the association, the crude and adjusted odds ratios were used, for which the statistical package SPSS was used.
Results:
Based on the adjusted OR, dyspareunia was identified (OR: 4.16, 95% CI 1.56-11.14), dysmenorrhea, (OR: 4.22, 95% CI 1.79-9.93), pelvic inflammatory disease (OR: 5.59, 95% CI 2.11-14.84), and alcohol consumption (OR: 2.87, 95% CI 1.10-7.49), as statistically significant risk factors for the development of infertility.
Conclusion:
The factors associated with infertility in the gynecology service of the Vitarte Hospital during the period from January 2015 to April 2019 are dyspareunia, dysmenorrhea, the history of pelvic inflammatory disease and alcohol consumption.
Key words: Infertility; Pelvic Inflammatory Disease; Ectopic pregnancy (source: MeSH NLM)
INTRODUCTION
We can define infertility as couple inability, whether one of them or both, to conceive naturally in a certain period. According to American Society for Reproductive Medicine (ASRM)1, female infertility occurs within a period of 12 months or more in women under 35 years old, or within a period of 6 months in women over 35 years old. Its etiology may be primary when the inability of achieving a spontaneous gestation occurs since the beginning of relationships without contraceptives. Or, it may be secondary, when the inability of achieving a spontaneous gestation occurs after a conception2.
The WHO exhorts to consider infertility as a worldwide health problem3. Fifteen percent of couples of reproductive age are infertile, worldwide. This represents from 60 to 80 million of infertile couples3. In Latin America, we notice high rates of secondary infertility. We can explain this due to sexual and reproductive health4. In Peru, we suspect that the situation is very similar, but there are not any updated reports that allow knowing the number of couples affected with this problem. A 2013 study reported that 4% of women between 15 and 49 years old are infertile, but it did not consider men5,6.
Factors that lead to infertility are not clearly known. Studies performed in Asia, Latin America and Middle East reveal that the main factors that predispose to infertility are: pelvic factor 35% (includes prior tubal disease and endometriosis), male factor with abnormalities in sperm production 40%, cervical factor 7.5%, and with no known cause 5%7-10. Besides, in the last years, women have had a change in their outlook on life, thus, they postpone their motherhood due to career goals and evolution in work11. Regarding this, we carried out the present study, aiming to determine factors associated: demographic, clinical and habits of harmful consumption, associated to female infertility.
METHODS
We conducted an observational, analytical, retrospective case-control stud. We obtained data through reviewing medical records and applying one data collection sheet. This sheet recorded information about demographic aspects, medical history and habits of harmful consumption, which we treated with confidentiality and approval of ethics committees from the hospital and university.
Every women from 18 to 50 years old, who attended gynecology service at Vitarte Hospital for female infertility between January 2015 and April 2019, composed study population. We excluded patients with a history of hysterectomy or bilateral tubular occlusion. Also, patients whose couple has been diagnosed as infertile.
We selected a random simple sample for cases and controls groups. Regarding cases, we included those women with diagnosis of infertility. In controls, we included those women who did not have diagnosis of infertility and puerperal ones.
We registered data collected on a Excel sheet and we analyzed them applying statistical software SPSS 23, considering a significance level of 95%. We employed frequency tables and descriptive statistics.
RESULTS
We reviewed 184 medical records of women who attended to gynecology service from Vitarte Hospital. 82 of them with diagnosis of infertility and 82 without this diagnosis or puerperal ones. Regarding general features: patients from 35 to 50 years old represent 60.9% of total of the cases group’s total. Average age of cases was 35.17 (s=4.96) and of controls, 30.4 (s=6.31). Patients with secondary school completed or higher education represent 75.6% of all cases. Likewise, of all cases, 34.1% presented dyspareunia, 74.4% showed dysmenorrhea, 46.3% submitted pelvic inflammatory disease, 18.3% had ectopic pregnancy and 25.6% showed endometriosis. In addition, 65.9% consume caffeine, 12.2% use tobacco, 39% drink alcohol and 29.3% use pharmaceuticals. SeeTable 1.
Table 1. General features of female assisted patients at Gynecology Service at Vitarte Hospital because of female infertility.
| Factors | Infertility (cases) | No infertility (controles) | Total | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Age | |||||||
| >35 - 50 years | 50 | 60.9% | 22 | 26.82% | 72 | 43.90% | |
| ≤ 35 years | 32 | 47.6% | 60 | 73.17% | 92 | 56.09% | |
| Media (DE) | 35.17 | (4.96) | 30.4 | (6.31) | |||
| Level of education | |||||||
| Incomplete secondary | 20 | 24.4% | 32 | 39.0% | 51 | 31.70% | |
| Complete secondary or higher education | 62 | 75.6% | 50 | 61.0% | 113 | 68.30% | |
| Dyspareunia | |||||||
| Yes | 28 | 34.1% | 12 | 14.6% | 40 | 24.4% | |
| No | 54 | 65.9% | 70 | 85.4% | 124 | 75.6% | |
| Dysmenorrhea | |||||||
| Yes | 61 | 74.4% | 33 | 40.2% | 94 | 57.3% | |
| No | 21 | 25.6% | 49 | 59.8% | 70 | 42.7% | |
| PID | |||||||
| Yes | 38 | 46.3% | 11 | 13.4% | 49 | 29.9% | |
| No | 44 | 53.7% | 71 | 86.6% | 115 | 70.1% | |
| Ectopic | |||||||
| Yes | 15 | 18.3% | 1 | 1.2% | 16 | 9.8% | |
| No | 67 | 81.7% | 81 | 98.8% | 148 | 90.2% | |
| Endometriosis | |||||||
| Yes | 21 | 25.6% | 23 | 28.0% | 44 | 26.8% | |
| No | 61 | 74.4% | 59 | 72.0% | 120 | 73.2% | |
| Caffeine | |||||||
| Yes | 54 | 65.9% | 43 | 52.4% | 97 | 59.1% | |
| No | 28 | 34.1% | 39 | 47.6% | 67 | 40.9% | |
| Tobacco | |||||||
| Yes | 10 | 12.2% | 2 | 2.4% | 12 | 7.3% | |
| No | 72 | 87.8% | 80 | 97.6% | 152 | 92.7% | |
| Alcohol | |||||||
| Yes | 32 | 39.0% | 14 | 17.1% | 46 | 28.0% | |
| No | 50 | 61.0% | 68 | 82.9% | 118 | 72.0% | |
| Pharmaceuticals | |||||||
| Yes | 24 | 29.3% | 15 | 18.3% | 39 | 23.8% | |
| No | 58 | 70.7% | 67 | 81.7% | 125 | 76.2% | |
| Total | 82 | 100.0% | 82 | 100.0% | 164 | 100.0% | |
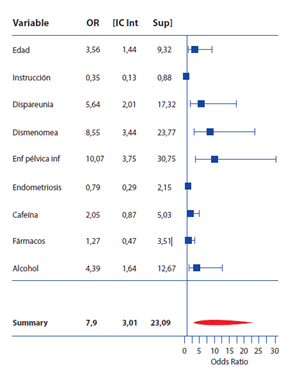
We noted that the factors associated were maternal age over 35 years old; dyspareunia, dysmenorrhea; history of pelvic inflammatory disease; alcohol consumption. Although, it is true that we found statistically significant association with ectopic pregnancy, described by a p value <0.01, we do not consider it a risk factor associated to infertility due to low amount of sample from patients. We can observe this in so wide confidence interval (95%) that ranges from 2.33 to 140.8. The same happens with tobacco use: it has a p value = 0.02, and a risk quantified by an OR 5.56 and a confidence interval (95%) that ranges from 1.18 to 26.2. In a similar way, we display adjusted OR, result of the binary logistic regression model. In this one, we identified as factors statistically significant for infertility development the following ones: dyspareunia (OR: 5.64, CI95% 2.01- 17.32), dysmenorrhea (OR: 8.55, CI95% 3.44-23.77), pelvic inflammatory disease (OR: 10.07, CI95% 3.75- 30.75) and alcohol consumption (OR: 4.39, CI95% 1.64-12.67). (Table 2) (Figure 1).
Table 2. Factors associated to infertility in patients treated in Gynecology Service at Vitarte Hospital.
| Factors associated | P value/1 | OR | OR CI95% | Adjusted OR | Adjusted OR CI95% | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | >35 - 50 years old | 0.001 | 4.21 | 2.11-8.38 | 3.56 | 1.44-9.32 | ≤ 35 years old | |||||
| Level of education | Incomplete secondary | 0.064 | 0.53 | 0.27-1.04 | 0.35 | 0.13-0.88 | Complete secondary or higher education | |||||
| History of Dyspareunia | Yes | 0.004 | 4.16 | 1.40-6.49 | 5.64 | 2.01-17.32 | No | |||||
| Hystory of Dysmenorrhea | Yes | 0.001 | 4.21 | 2.22-8.37 | 8.55 | 3.44-23.77 | No | |||||
| History of Pelvic inflammatory disease | Yes | <0.01 | 5.57 | 2.58-12.03 | 10.07 | 3.75-30.75 | No | |||||
| History of Ectopic pregnancy/2 | Yes | <0.01 | 18.13 | 2.33 -140.8 | - | - | No | |||||
| History of Endometriosis | Yes | 0.6 | 0.83 | 0.41-1.65 | 0.79 | 0.29-2.15 | No | |||||
| Caffeine consumption | Yes | 0.11 | 1.66 | 0.88-3.12 | 2.05 | 0.87-5.03 | No | |||||
| Tobacco use/2 | Yes | 0.016 | 5.56 | 1.18- 26.2 | - | - | No | |||||
| Use of pharmaceuticals | Yes | 0.1 | 1.84 | 0.88-3.85 | 1.27 | 0.47-3.51 | No | |||||
| Alcohol consumption | Yes | 0.002 | 3.1 | 1.50-6.42 | 4.39 | 1.64-12.67 | No |
/1 Level of significance obtained through chi square of association. /2 Due to low simple for its calculation, we omitted it from the logistic regression model and, only for-profit, we show raw OR.
DISCUSSION
This study has great relevance in both clinical-practical field and theoretical field, since because of this we have better vision regarding determinants associated to infertility. We discovered significant association in women over 35 years old. Similar result to research by Ramos et al12with OR = 1.9, CI 95%: 1.3-4.1, p<0.001 and research by Cabrera13who also found association between these two variables. Martínez14determined that 67% of people with infertility were between 30 and 39 years old. Likewise, Malo and Marín15identified that age was a risk factor associated to infertility given by a p value <0.05. Finally, Toledo16in his study established that patients who most attended to examination were 39-year-old women. Regarding level of education, we did not statistically significant association in our sample. However, He X et al17in their study identified that high level of education was a protector factor in women with infertility (OR = 0.522, IC 95%: 0.391-0.696). Moreover, Toledo16states that most women who attended to examination due to infertility had a complete academic level. On the other side, we discovered statistically significant association with dyspareunia. These results confirm the findings by HE X17, who also identified association with these two variables (OR = 2.447, CI 95%: 1.201-4.986). Mayhuasca18did not find any association between dyspareunia and infertility in his retrospective descriptive study. In addition, we discovered statistically significant association between dysmenorrhea and infertility. We confirm this thanks to the study by Mallikarjuna et al19with a (OR: 6.08, p=0.009). HE X17on his own, also discovered association with this factor (OR = 1.62). Furthermore, history of pelvic inflammatory disease turned out to be statistically significant in our study, confirming the findings by HE X17who also identified an association between these two variables with (OR =7.07, IC95% 3.4-14.46). Ramos et al12found out that it was not statistically significant with a p value over 0.05. Martínez13reported a 23% incidence as well as Benavides20who stated a 19% incidence. This contrasts our results, which suggest in our group of cases a 49% incidence. Regarding ectopic pregnancy, although we discovered statistically significant association, this may have been due to few sample of patients with this history. This is reflected in the so wide confidence interval. Safarinnejad et al21discovered association with ectopic pregnancy (OR= 2.45; CI 95%: 1.90-3.44; p = 0.04). Thounneau22found out association given by a OR: 9.9. Roa Huapaya23also identified association with this factor with a risk quantified by OR: 2.59. History of endometriosis resulted non-significant with infertility, in contrast with the findings by Franco et al24. According to their study, one of the diseases associated to female infertility with higher incidence was endometriosis with a 43.4%. Roa Huapaya23discovered association given by a (OR: 4.1). Mayhuasca18found out association with a p minor than 0.05. Caffeine consumption is not statistically significant, confirming with studies by Soylu et al12, who discovered that regular coffee portions were not a risk (OR: 1.00; IC: 0.97 - 1.03). Ramos et al12, on their own, confirm our results stating that caffeine is not associated to infertility. Lyngsø et al26, in their study, did not find out any association between caffeine consumption and infertility. However, caffeine consumption increases miscarriage according to daily intake. In our study, alcohol consumption is statistically significant. Greenlee et al27studied associated factors of female infertility in 322 cases and 322 controls, mentioning association between alcohol consumption and infertility with (OR= 1.8 IC 95% 1.2- 16.3%). Contrasting with research by Ramos et al11, who discovered that there is not any statistically significant association between alcohol consumption and infertility, given by p values over 0.05. Although, we found statistically significant association with tobacco use, this was due to a few sample of patients regarding tobacco use. Thus, we appreciate a confidence interval so wide, which we should improve performing more studies that calculate an accurate sample size. Moreover, Greenlee et al’s27study did not find out statistically significant association between tobacco use and infertility (OR= 1.6 IC 95% 0.9-2.9). Use of pharmaceuticals is not statistically significant unlike study by He X et al17, who discovered association with history of drug treatment (OR= 23.57, IC 95%: 12.32-45.10). Benito29reports that pharmaceuticals possibly related to sterility are numerous, such as, anti-inflammatories, chemotherapeutic, hormones, antibiotics, and others like, caffeine, chlortetracycline, dapsone, phenothiazines, nifedipine, cimetidine, cyclosporine or spironolactone. We could recommend try to avoid its use in patients with difficulty conceiving, unless it is strictly necessary. Nevertheless, we should consider that sometimes it could be the case of a patient with underlying disease. We recommend that health service professionals register the age of the couple, since it also represents an associated factor according to the literature. At the methodological level, we suggest validating these results in other sample populations and considering associated factors such as ectopic pregnancy and tobacco use, in order to guarantee an accurate representation and results that are more precise.
We state that limitations of this research are the fact that patients who attend due to infertility are referred to a more complex center that has a specialized service of infertility for further studies. There were also medical records with missing information, which did not embrace the total of factors to evaluate.
CONCLUSIONS
In the study, we identified dyspareunia, dysmenorrhea, history of pelvic inflammatory disease, and alcohol consumption as significant risk factors for infertility.
We did not find out statistically significant association between age, level of education, ectopic pregnancy, endometriosis, tobacco use and use of pharmaceuticals with infertility.
REFERENCES
1. Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9(12):e1001356. DOI: 10.1371/journal.pmed.1001356 [ Links ]
2. Sañudo Toca L. Consecuencias de la infertilidad/esterilidad en la salud de la mujer. Consequences of infertility/sterility in woman´s health (Internet). 3 de junio de 2014 (citado 7 de febrero de 2020); Disponible en: https://repositorio.unican.es/xmlui/handle/10902/5195 [ Links ]
3. Vayena E, Peterson HB, Adamson D, Nygren K-G. Assisted reproductive technologies in developing countries: are we caring yet? Fertil Steril. 1 de agosto de 2009;92(2):413-6. DOI: 10.1016/j.fertnstert.2009.02.011 [ Links ]
4. Neciosup V. Problemas de Política y Estado Situacional de las técnicas de reproducción humana asistida en el Perú. Departamento de Investigación Documentaria Parlamentaria del Congreso de la República del Perú 2018. Nov. 2018:20.24pp. Disponible en: http://www2.congreso.gob.pe/sicr/cendocbib/con5_uibd.nsf/25ADE7B6962521CC0525834A00726952/$FILE/reproduccion_asisitida_N20.pdf [ Links ]
5. Roa-Meggo Y. La infertilidad como problema de salud pública en el Perú. Rev Peru Ginecol Obstet. 1 de diciembre de 2011;58:79-85. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S2304-51322012000200003 [ Links ]
6. Rojas Quintana P, Medina Tío D, Torres Ajá L. Infertilidad. MediSur. agosto de 2011;9(4):340-50. Disponible en: http://medisur.sld.cu/index.php/medisur/article/view/1692 [ Links ]
7. Vargas JAV, Núñez DAO, Marín IH, Rodríguez JMT, Ayala AR. Análisis epidemiológico de la infertilidad en una población mexicana. Ginecol Obstet Mex. 2005;73:360-4. Disponible en: https://www.medigraphic.com/pdfs/ginobsmex/gom-2005/gom057d.pdf [ Links ]
8. Deyhoul N, Mohamaddoost T, Hosseini M. Infertility-Related Risk Factors: A Systematic Review. Int J Womens Health Reprod Sci. 1 de enero de 2017;5(1):24-9. DOI: 10.15296/IJWHR.2017.05 [ Links ]
9. Grodstein F, Goldman MB, Cramer DW. Infertility in women and moderate alcohol use. Am J Public Health. 1 de septiembre de 1994;84(9):1429-32. DOI: 10.2105/ajph.84.9.1429 [ Links ]
10. Anwar S, Anwar A. Infertility: A Review on Causes, Treatment and Management. . Infertility. 2016;2(6):5. Disponible en: https://scientonline.org/open-access/infertility-a-review-on-causes-treatment-and-management.pdf [ Links ]
11. Vidal C. Esterilidad e infertilidad humanas. Abordaje y tratamiento. Farm Prof. 1 de septiembre de 2001;15(8):96-101. Disponible en: https://www.academia.edu/25102315/Esterilidad_e_infertilidad_humanas._Abordaje_y_tratamiento [ Links ]
12. Ramos RR, Gutiérrez GR, Monroy IA, Sánchez HGM. Factores de riesgo asociados con infertilidad femenina. Ginecol Obstet México. 2008;76(12). Disponible en: https://www.medigraphic.com/pdfs/ginobsmex/gom-2008/gom0812d.pdf [ Links ]
13. Cabrera Figueredo I, Luaces Sánchez P, González González F, González Reigada A, Rodríguez Hernández L, Cruz Fernández CY de la. Análisis de la infertilidad femenina en la población camagüeyana. Rev Arch Méd Camagüey. diciembre de 2017;21(6):705-16. Disponible en: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1025-02552017000600004 [ Links ]
14. Martínez Guadalupe ÁI, Mascaro Rivera YS, Méjico Mendoza SW, Mere del Castillo JF. Características epidemiológicas, clínicas y quirúrgicas de pacientes con embarazo ectópico en el Hospital Nacional Arzobispo Loayza. Rev Peru Ginecol Obstet. julio de 2013;59(3):171-6. Disponible en: http://www.scielo.org.pe/scielo.php?pid=S2304-51322013000300005&script=sci_abstract [ Links ]
15. Malo Chiclayo CC, Marin Chalan LB. Relación entre los factores de riesgo reproductivo y la infertilidad de las trabajadoras sexuales atendidas en e Hospital Regional Docente de Trujillo 2016. Univ Priv Antenor Orrego - UPAO (Internet). 22 de septiembre de 2017 (citado 8 de febrero de 2020); Disponible en: http://repositorio.upao.edu.pe/handle/upaorep/3029 [ Links ]
16. Caro T, Elsa C. Abordajes terapéuticos sobre infertilidad en mujeres atendidas en el servicio de fertilidad del Hospital Nacional Arzobispo Loayza durante el año 2018. Univ Priv S Juan Baut (Internet). 2019 (citado 8 de febrero de 2020); Disponible en: http://repositorio.upsjb.edu.pe/handle/upsjb/2014 [ Links ]
17. He X, Hou Q, Jiang H, Huang H. (A case-control study on the risk factors of female infertility). Zhonghua Liu Xing Bing Xue Za Zhi Zhonghua Liuxingbingxue Zazhi. abril de 2009;30(4):352-5. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/19731526 [ Links ]
18. Mayhuasca Quispe R. Factores asociados a infertilidad en el servicio de reproducción humana del Hospital Nacional Madre - Niño "San Bartolomé" en el periodo enero a julio del 2012. Repos Tesis - UNMSM (Internet). 2014 (citado 8 de febrero de 2020); Disponible en: http://cybertesis.unmsm.edu.pe/handle/cybertesis/9871. [ Links ]
19. Mallikarjuna MN, Rajeshwari BV. Selected risk factors of infertility in women: case control study. . Int J Reprod Contracept Obstet Gynecol. 2015; 4(6):1714 -19. DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20151129 [ Links ]
20. Benavides Montes de Oca R. Factores de Riesgo Asociados a Infertilidad en Mujeres Atendidas en el Servicio de Ginecología y Obstetricia del Hospital Daniel Alcides Carrión de Tacna de Enero de 2012 a Diciembre de 2016. Univ Priv Tacna (Internet). 2019 (citado 8 de febrero de 2020); Disponible en: http://renati.sunedu.gob.pe/handle/sunedu/425436 [ Links ]
21. Safarinejad MR. Infertility among couples in a population-based study in Iran: prevalence and associated risk factors. Int J Androl. junio de 2008;31(3):303-14. DOI: 10.1111/j.1365-2605.2007.00764.x [ Links ]
22. Thonneau P, Quesnot S, Ducot B, Marchand S, Fignon A, Lansac J, et al. Risk factors for female and male infertility: results of a case-control study. Hum Reprod Oxf Engl. enero de 1992;7(1):55-8. DOI:10.1093/oxfordjournals.humrep.a137557 [ Links ]
23. Huapaya R, Angeles MDL. Factores de riesgo asociados a la infertilidad en mujeres entre 25 a 35 años atendidas en el consultorio de infertilidad del Instituto Nacional Materno Perinatal durante el periodo 2018. Univ Priv S Juan Baut (Internet). 2019 (citado 8 de febrero de 2020); Disponible en: http://repositorio.upsjb.edu.pe/handle/upsjb/1967 [ Links ]
24. Franco A, Salvador J, Lostaunau A, Madariegue E. Hallazgos Laparoscópicos en pacientes con infertilidad. Experiencia en el Hospital Nacional Cayetano Heredia. 1995-1998. Rev Peru Ginecol Obstet. 2004;50(3):153-9. Disponible en: http://www.spog.org.pe/web/revista/index.php/RPGO/article/view/426 [ Links ]
25. Soylu LÍ, Jensen A, Juul KE, Kesmodel US, Frederiksen K, Kjaer SK, et al. Coffee, tea and caffeine consumption and risk of primary infertility in women: a Danish cohort study. Acta Obstet Gynecol Scand. 2018;97(5):570-6. DOI: 10.1111/aogs.13307 [ Links ]
26. Lyngsø J, Ramlau-Hansen CH, Bay B, Ingerslev HJ, Hulman A, Kesmodel US. Association between coffee or caffeine consumption and fecundity and fertility: a systematic review and dose-response meta-analysis. Clin Epidemiol. 2017;9:699-719. DOI: https://doi.org/10.2147/CLEP.S146496 [ Links ]
27. Greenlee AR, Arbuckle TE, Chyou P-H. Risk factors for female infertility in an agricultural region. Epidemiol Camb Mass. julio de 2003;14(4):429-36. DOI: 10.1097/01.EDE.0000071407.15670.aa [ Links ]
28. Ramos RR, Gutiérrez GR, Monroy IA, Medina HG. Factores de riesgo asociados con infertilidad femenina. Ginecol Obstet México. 2008; 76(12): 717 - 21 Disponible en: https://www.medigraphic.com/pdfs/ginobsmex/gom-2008/gom0812d.pdf. [ Links ]
29. Heredia Benito M, Sanchez Ruiz de Gordoa M, Ruiz Martín de la Torre R, Lopez Sanchez P, Flor García A. Fármacos e infertilidad: revisión. Clínica E Investig En Ginecol Obstet. marzo de 2012;39(2):69-72. DOI: 10.1016/j.gine.2011.09.004. [ Links ]
Received: March 05, 2020; Accepted: March 19, 2020











 texto en
texto en