Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.20 no.2 Lima abr./jun 2020
http://dx.doi.org/10.25176/rfmh.v20i2.2936
Original article
Albumin and neutrophil to lymphocyte ratio as predictors of tumor stage in patients with gastric cancer
1Instituto de Investigación en Ciencias Biomédicas, Facultad de Medicina Humana, Universidad Ricardo Palma, Lima-Perú.
Objective:
To determine the association between albumin, inflammatory markers and tumor stage of gastric cancer patients in a National Hospital of Peru.
Methods:
An observational, analytical and retrospective study corresponding to the 2017 and 2018 years. The frequencies and distribution of the variables were evaluated: clinical stage according to the AJCC 2018, albumin as a nutrition indicator and Neutrophil Lymphocyte-Ratio (NLR) as an indicator of the inflammatory and immune response. The value 2.44 was taken as the cut-off point for high NLI.
Results:
were included 96 patients. The average age was 63.5 years ± 12.8, the male: female ratio was 1: 1, 80.2% came from the region of the coast of Peru; 70.8% had an advanced clinical stage and 85.4% corresponded to tumor size T3 and T4. 64% presented undifferentiated histological grade and 30.1 showed evidence of metastasis. The mean NLR was 2.94 ± 1.7, and albumin was 3.64 g / dl ± 0.6. In the bivariate analysis, a significant association was found between the high level of NLR and the advanced clinical stage (OR: 4.46 95% CI 1.65-13.27 p <0.001), and between low levels of serum albumin with advanced stage (OR: 13.02 95% CI 1.78-563.36 p <0.005).
Conclusion:
A late diagnosis was found in 70% of the patients. High NLR as an indicator of inflammatory response and low albumin as an indicator of nutrition are predictors of the advanced clinical stage in gastric cancer.
Keywords: Stomach Neoplasms; Neoplasm Staging; Neutrophil-to-Lymphocyte Ratio. (source: MeSH; NLM
INTRODUCTION
Gastric cancer (GC) is a public health problem1,2. It remains a major cause of cancer mortality in East Asia, Eastern Europe, and South America with more than 700,000 deaths annually3. More than 70% of new cases and deaths are from developing countries, resulting in an important social burden4. Therefore, the development of cheap and reliable biomarkers to diagnose GC is crucial.
In the USA and Europe, gastric carcinoma has shown a notable decrease in its incidence3. However, despite improvements in surgical and oncological treatments, mortality from this neoplasm remains very high, with survival rates 5 years after diagnosis of only 20-30% in western countries3. Within this general poor prognosis, there is notable individual variability in terms of survival, so it is very important to be able to know the predictive factors about the possible evolution of a certain patient5.
In Peru, the CG is among the three most frequent cancers, with a predominance in the Cajamarca regions, related to poverty indicators(6-8).
Helicobacter pylori infection, low socioeconomic status, a diet high in red meat, sedentary lifestyle and genetic predisposition have been identified as the main risk factors6,9-11.
Inflammation appears to be the backdrop for tumor development and progression, either in the blood or in tumor tissue. The neutrophil-lymphocyte ratio known as the Neutrophil-Lymphocyte Index (INL) has been considered an indicator of systemic inflammation in many current clinical studies, including gastric cancer12-24, in the absence of obvious infection25.
Chronic inflammation-mediated primarily by prolonged neutrophil activation promotes carcinogenesis through genotoxicity, T-cell inhibition, angiogenesis, and invasion (seeFigure 1). On the contrary, the lymphocytic population has an antitumor function by recognizing tumor cells and activating tumor cytolytic activity through NK and TCD8 (+) cells26.
Although tumor size, degree of invasion, lymph node involvement and the presence of metastases have been used for tumor staging and predict the development and aggressiveness of the neoplasm, there is great variability in the survival of patients who are in the same stage, which suggests the existence of additional factors that influence tumor behavior. The division of stages (I and II as localized stages and III and IV as advanced stages) has been proposed in advanced studies27,28. Albumin as an indicator of nutritional status, responsiveness to treatments and complications has been mentioned in multiple studies.
The usefulness of INL and albumin to help classify early to advanced tumor stages is still a controversial issue, therefore, the objective of this study was to evaluate the utility of INL and albumin as predictors of a clinical-stage in patients diagnosed with gastric cancer.
METHODS
Design and population
An observational, analytical, retrospective study was carried out, in which all hospitalized patients with a clinical diagnosis of gastric adenocarcinoma were included during the period July 2017 and July 2018 in the Stomach Surgery Service of the Edgardo Rebagliati Martins National Hospital ( HNERM) of the Peruvian social security (ESSALUD).
Patients with incomplete preoperative data (insufficient data from the file of the Stomach Surgery Service) and those who were determined to be tumors of the esophagus-gastric junction were excluded
Study variables
Among the variables included in the study, sociodemographic-clinical variables (sex, age, place of origin), laboratory (Neutrophil-Lymphocyte Index, Albumin) and tumor clinical stage according to the TNM for gastric cancer of the AJCC 2018 were taken into account.
The INL was obtained as the result of the ratio of the number of neutrophils between lymphocytes found in the CBC and the albumin of the biochemical examination taken preoperatively. INL was considered elevated to any value greater than 2.44 based on previous studies in Latin America.
Statistic analysis
Data collection was performed using the datasheet. The digitization of the data was carried out in the Excel 8.0 program and the analysis with STATA 12.0. Descriptive statistics were performed with measures of central tendency and dispersion. For inferential statistics, it was calculated as a measure of association OR, with 95% CI with
RESULTS
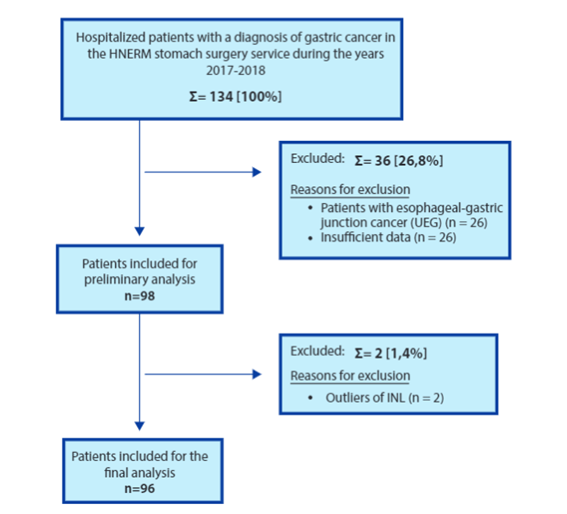
During the period July 2017 to July 2018, 134 hospitalized patients were initially included in the HNERM Stomach Surgery Service with a diagnosis of gastric cancer. Data from 98 patients who met the work inclusion criteria were included in the preliminary analysis. Two patients with atypical INL data were identified according to Tukey's method, which is why they were excluded. Finally, data from 96 patients were analyzed (seeFigure 1).
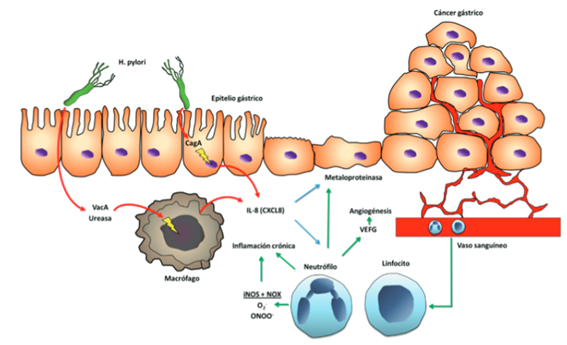
Figure 1. Role of the immune response in the progression of gastric cancer. Adapted from: Gobert AP, Wilson KT. Human and Helicobacter pylori Interactions Determine the Outcome of Gastric Diseases. Curr Top Microbiol Immunol. 2017; 400: 27-52.
The average age was 63.5 years ± 12.8, 68.7% of the patients were between 45 and 75 years old. Age was determined to follow a normal distribution. In the distribution of patients according to sex, the most frequent was female, representing 52% of the total sample, maintaining a ratio of 1: 1. Regarding the place of origin, it is evident that the majority of patients lived in the coastal region of Peru, representing 80.2% of the sample.
Regarding the clinical stage, 70.8% had an advanced stage (cTNM III-IV). Regarding tumor criteria, it was evident that the majority of patients were diagnosed with advanced tumor size in 85.4%, finding positive nodes in 57.2%; regarding the metastasis criterion, it was positive in 30.2% of patients (seeTable 1).
Table 1. Distribution of patients according to age, sex, place of origin, tumor criteria, lymph node criteria, metastasis criteria and clinical stage.
| (n=96) | % | |
|---|---|---|
| Age (years) | ||
| Media (±SD) | 63,5 | (±12,8) |
| Gender | ||
| Male | 46 | (48%) |
| Female | 50 | (52%) |
| Place of origin | ||
| Coast | 77 | (80,2%) |
| Mountain range | 4 | (4,1%) |
| Jungle | 15 | (15,6%) |
| cT | ||
| T1/2 | 14 | (14,5%) |
| T3/4 | 82 | (85,4%) |
| cN | ||
| Negative N | 41 | (42,7%) |
| N positive | 55 | (57,2%) |
| cM | ||
| Negative N | 67 | (69,8%) |
| N positive | 29 | (30,2%) |
| cTNM | ||
| I-II | 28 | (29,1%) |
| III-IV | 68 | (70,8%) |
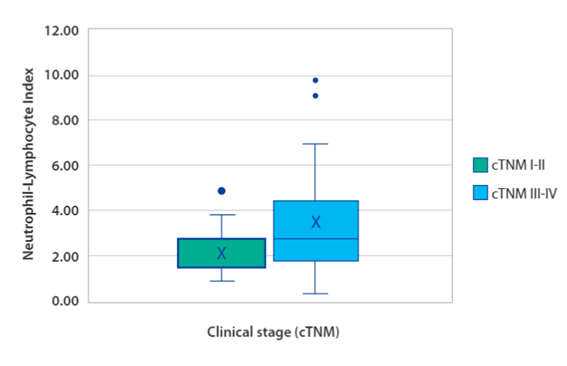
In the analysis of the Neutrophil-Lymphocyte Index (INL) the mean was 2.94 ± 1.7 and the median 2.44 (RIC 1.68-3.84) was also observed to have a non-parametric distribution, confirmed by the Shapiro-Wilk test (p <0.001). According to the clinical stage (cTNM), in the localized stages (cTNM I-II) the mean was 2.13 ± 0.9, the median 1.97 (RIC 1.45-2.63), while in advanced stages (cTNM III-IV) the mean was 3.28 ± 1.8, the median 2.73 (RIC 1.79-4.35) (See Figure3). When comparing both means with the t-student statistic, a statistically significant difference was obtained (p <0.003). The albumin mean was 3.64 g / dl ± 0.6 in the advanced stage group was 3.51 g / dl ± 0.6.
Table 2describes the clinical-laboratory characteristics of patients with gastric cancer according to clinical stage. Variables were analyzed according to their nature with the t-student, chi2 and Fisher's exact tests to determine the p-value. In the clinical stage (cTNM), a higher proportion of patients with advanced stages with high INL (0.94: 1) is evident than in those with normal INL (0.20: 1) (p <0.001). The rest of the variables did not demonstrate to have statistically significant differences.
Table 2. Bivariate analysis of clinical-laboratory characteristics in gastric cancer patients according to the clinical stage.
| Variables | cTNM III-IV n=68 (70,8%) | cTNM I-II n=28 (20,1%) | OR | 95% CI | chi2 | p |
|---|---|---|---|---|---|---|
| Age | 0,75 | 0,27-1,98 | 0,41 | 0,52 | ||
| <65 | 34 (35,4%) | 12 (12,5%) | ||||
| ≥65 | 34 (35,4%) | 16 (16,6%) | ||||
| Gender | 1,08 | 0,41-2,89 | 0,04 | 0,85 | ||
| Male | 33 (34,8%) | 13 (13,5%) | ||||
| Female | 35 (36,4%) | 15 (15,3%) | ||||
| INL | 4,46 | 1,65-13,27 | 11,06 | 0,0009 | ||
| ≥2,44 | 49 (51,0%) | 10 (10,4%) | ||||
| <2,44 | 19 (19,7%) | 18 (18,7%) | ||||
| Serum albumin | 13,02 | 1,78 - 5,36 | 8,79 | 0,0030 | ||
| <3,5 | 24 (30,3%) | 1 (1,2%) | ||||
| ≥3,5 | 35 (44,3%) | 19 (24,0%) |
An OR of 4.64 (95% CI 1.65-13.27) was obtained between the high INL and the advanced clinical stage, which was statistically significant (p = 0.001), similarly with low serum albumin levels OR 13.02 95% CI 1.78-5 , 36 (p = 0.003).
DISCUSSION
Our study found that both high INL, as a marker of inflammatory and immune response, and low albumin, as an indicator of nutrition, were predictive factors of advanced clinical stage in gastric cancer.
Gastric cancer is a public health problem, due to its prevalence, aggressiveness, and late diagnosis. It is necessary to develop methods for its timely detection and stratified management8. Multiple variables that influence the prognosis depend on the general state of the patient, nutritional status, age, comorbidities, the histological characteristics of the tumor, the degree of growth and the extension. of the neoplasm, as well as of the patient's systemic inflammatory response to the tumor6,10,17. This inflammatory response is related to the growth and the capacity for invasion and metastasis of the neoplasm18.
The systemic inflammatory response accompanies cancer development, both for early or advanced cancer, which provides new methods for the early identification of GC30,31. Previous studies support the "transformation of inflammation and cancer" hypothesis32-34: chronic gastritis can cause GC32; Chronic viral hepatitis can cause cirrhosis, which in turn leads to liver cancer33. The epithelium of the gastrointestinal tract is continuously exposed to the external environment and is susceptible to inflammation due to various pathogens or other stimuli34.
Various inflammatory indicators on prognosis in tumors of the digestive tract, pancreas, and liver have been evaluated, based on the relationship between inflammatory response and tumor progression11. The Glasgow index based on the values of C-reactive protein and albumin19, the ratio of circulating neutrophils/lymphocytes20, the platelet/ lymphocyte ratio21and platelets/neutrophils, also called the Onodera index22, stand out.
Resectability is a criterion that is confirmed after surgery and that at the time of diagnosis can only be presumed by clinical TNM tumor classification, whose precision is limited and tends to under-stage in at least 20% of cases9,10. Therefore, we need to have other predictive parameters, independent of the clinical TNM, and that can be determined at the time of tumor diagnosis5,6.
In the present study, it was observed that the majority of patients were between 60-75 years old with an average age of 63.5 years ± 12.8, also 62.5% were older than 60 years. No significant association was found between advanced age and advanced clinical stage. This agrees with studies carried out in Brazil by Szor et al.34, however, in the multivariate analysis, it was found that age over 65 could have some influence on the prognosis of patients with gastric cancer.
The proportion of the sample according to sex was 1: 1. No association was found between sex and high INL, low serum albumin, and advanced tumor stage. Although female sex has been associated with an antitumor protective effect when interacting with estrogen receptors, this has not been definitively demonstrated in meta-analyzes and randomized studies35.
The highest proportion of patients (80.2%) came from the coastal area. According to the Ministry of Health, the highest incidence of patients is found on the coast8, this correlates with our findings. This situation is related to the population density in the coastal region of Peru and the internal migratory currents.
Of the patients hospitalized for gastric cancer, 7 out of 10 corresponded to advanced clinical stages, this reflects the low presence of primary and secondary prevention in our health system in terms of a pathology that notably affects our population. Similarly, most patients had advanced tumor criteria in 84.5%, positive lymph node criteria in 57.3%, and positive metastasis criteria in 30.2%.
It is necessary to strengthen the first level of care and improve promotional preventive activities in order to decrease the prevalence and increase the proportion of patients diagnosed in the early stages7, with emphasis on Lifestyle Medicine.
The relationship between systemic inflammation and tumors has been of interest to researchers. In 1869, Ashworth first proposed the CTC “Circulating Tumor Cells” concept. After years of research, CTC tests were approved for clinical use. However, the rarity, heterogeneity, and high cost of CTC tests pose challenges in using them as biomarkers35-37. This has led researchers to seriously consider the phenomenon that cancer cells enter the peripheral blood in the early stage of cancer, but early metastasis is rare38,39. Recent publications have reported that CTCs entering the peripheral blood trigger an immune response that includes an increase in the proportion of macrophages and neutrophils associated with cancer. Li40observed an increase in the proportion of peripheral blood neutrophils in the progression of malignant tumors, which was associated with the prognosis. Burr41noted that non-steroidal anti-inflammatory drugs can reduce the risk of systemic inflammation and tumorigenesis.
The cut-off point for determining the high INL value is currently debated. As an inflammatory marker, it is used in different pathologies, gastric cancer is one of them. In 1976 Nakahara et al. coined the term INL in the medical literature and determined its association with the prognosis of patients with lung cancer. The cut-off point has been defined through ROC curves so that those patients with a poor prognosis can be easily identified28. According to Min et al. the average cutoff point would be 3.00. Deng et al according to their analysis found that the appropriate cut-off point would be 2.46. However, Szor et al in 383 patients of Brazilian origin determined that the appropriate cutoff point would be 2.44, being this the cutoff point used in this study. The INL measure is not standardized, which is why more studies are required in different Latino populations with gastric cancer.
In our study the average INL was 2.94 ± 1.7, 61.5% of the patients had a high INL value, particularly the group with an advanced clinical stage (72.0%) with a mean of 3.28 ± 1.8 having this value statistically significant difference. with the mean of the group with the localized stage (p <0.003). In the bivariate analysis, it was found that patients with high INL were 4 times more at risk of presenting an advanced clinical stage. Likewise, Rodríguez C. in a Cajamarca hospital found a 6-fold increase in the probability of having an advanced clinical-stage, similarly in China, Min et al. demonstrated a 1.5-fold increase in risk
Neutrophils make up 50-70% of all white blood cells in the human circulation with an average life span of 5.4 days in the homeostatic condition of oxidative stress response42. They are currently believed to promote cell proliferation, vascularization, and metastasis cancer by producing pro-angiogenic chemokines and vascular endothelial growth factor43,44. Peripheral blood lymphocytes are currently believed to cause synergistic cytotoxicity and exert tumor suppressive properties45.
Interestingly, a recently published work by Tiangy Fang et al46, showed that the systemic inflammatory markers INL and IPL were more valuable for the diagnosis of GC than the traditional tumor markers CEA and CA19-9, this diagnostic value was higher in patients male than a female with CG.
Furthermore, the INL was significantly higher in GC patients than in normal subjects, which also indicated that the inflammatory response of the neutrophil-based tumor in the peripheral blood of the tumor patients was stronger than the lymphocyte-based antitumor immune effect45.
In our study, albumin was the only biochemical parameter that presented statistical significance (p = 0.003) that is related as a predictor of advanced disease in our population.
Numerous biomarkers have been proposed in gastric cancer. The greatest contribution of our work is that albumin as a marker of the nutritional status of the patient with gastric cancer and INL as an inflammatory indicator and immune response, constitute two simple parameters, easily accessible and very low cost, with the ability to predict the clinical stage in patients with gastric cancer. Our analysis would represent one of the first reports in the Peruvian population that mentions hypoalbuminemia and INL associated with advanced stage in patients with gastric cancer.
Like other published works, ours has the limitation of not being prospective, which could reduce the accuracy of the data collected in the medical record. Corresponds to a single-center study, with a limited sample size. Like other published works, ours has the limitation of not being prospective, which could reduce the accuracy of the data collected in the medical record. Corresponds to a single-center study, with a limited sample size.
REFERENCES
1. Bray, F., Ferlay, J., Soerjomataram, I., Siegel, RL, Torre, LA y Jemal, A. (2018), Estadísticas globales de cáncer 2018: Estimaciones de incidencia y mortalidad de GLOBOCAN en todo el mundo para 36 cánceres en 185 países. CA: A Cancer Journal for Clinicians, 68: 394-424. doi: 10.3322 / caac.21492 [ Links ]
2. The Lancet. GLOBOCAN 2018: counting the toll of cancer,The Lancet, Volume 392, Issue 10152, 985. https://doi.org/10.1016/S0140-6736(18)32252-9 [ Links ]
3. RL Siegel, KD Miller y A. Jemal, "Estadísticas de cáncer, 2018", CA: a Cancer Journal for Clinicians , vol. 68, no. 1, págs. 7-30, 2018.Ver en: Sitio del editor | Google Académico. [ Links ]
4. Global Burden of Disease Cancer Collaboration, "Incidencia global, regional y nacional del cáncer, mortalidad, años de vida perdidos, años vividos con discapacidad y años de vida ajustados por discapacidad para 32 grupos de cáncer, 1990 a 2015: un análisis sistemático para el estudio de la carga global de la enfermedad, " JAMA Oncology , vol. 3, no. 4, págs. 524-548, 2017.Ver en: Sitio del editor | Google Académico. [ Links ]
5. Van Cutsem E, Sagaert X, Topal B, Haustermans K, Prenen H. Gastric cancer. Lancet Lond Engl. 26 de 2016;388(10060):2654-64. [ Links ]
6. Ramos W, Guerrero N, Medina J, Guerrero PC. Análisis de la situación del cáncer en el Perú, 2018. Lima: Centro Nacional de Epidemiología, Prevención y Control de Enfermedades; 2019. [ Links ]
7. Torres-Román JS, Grados-Sánchez O. Cáncer gástrico en el Perú: una realidad susceptibilidad de cambio. Rev. gastroenterol. Perú [Internet]. 2015 Jul [citado 2019 Feb 05]; 35(3): 276-276. Disponible en: http://www.scielo.org.pe/scielo. php?script=sci_arttext&pid=S1022-51292015000300013&lng=es [ Links ]
8. Ministerio de Salud. Analisis de la situacion del cancer en el Peru, 2013. Lima: Ministerio de Salud; 2013. Disponible en: http://www.dge.gob.pe/portal/docs/ asis_cancer.pdf [ Links ]
9. de Martel C, Forman D, Plummer M. Gastric cancer: epidemiology and risk factors. Gastroenterol Clin North Am. junio de 2013;42(2):219-40. [ Links ]
10. Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F. Gastric Cancer: Descriptive Epidemiology, Risk Factors, Screening, and Prevention. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. mayo de 2014;23(5):700-13. [ Links ]
11. Kelley JR, Duggan JM. Gastric cancer epidemiology and risk factors. J Clin Epidemiol. enero de 2003;56(1):1-9. [ Links ]
12. Ayala de la Peña F, Yufera Soler JC, Ivars MA, Fernandez Sanchez A, Navarro Manzano E, De la Morena Barrio P, et al. PNeutrophil-lymphocyte ratio (NLR) as a prognostic factor in metastatic breast cancer. Ann Oncol [Internet]. el 1 de septiembre de 2017 [citado el 12 de junio de 2018];28(suppl_5). Disponible en: http://academic.oup.com/annonc/article/doi/10.1093/annonc/mdx365.046/41085 12/283PNeutrophillymphocyte-ratio-NLR-as-a-prognostic [ Links ]
13. Azab B, Camacho-Rivera M, Taioli E. Average Values and Racial Differences of Neutrophil Lymphocyte Ratio among a Nationally Representative Sample of United States Subjects. PLOS ONE. el 6 de noviembre de 2014;9(11):e112361. [ Links ]
14. Chen Y, Yan H, Wang Y, Shi Y, Dai G. Significance of baseline and change in neutrophil-to-lymphocyte ratio in predicting prognosis: a retrospective analysis in advanced pancreatic ductal adenocarcinoma. Sci Rep. el 9 de abril de 2017;7(1):753. [ Links ]
15. Huang Q, Zhou L, Zeng W, Ma Q, Wang W, Zhong M, et al. Prognostic Significance of Neutrophil-to-Lymphocyte Ratio in Ovarian Cancer: A Systematic Review and Meta-Analysis of Observational Studies. Cell Physiol Biochem. 2017;41(6):2411-8. [ Links ]
16. Lalani A-KA, Xie W, Martini DJ, Steinharter JA, Norton CK, Krajewski KM, et al. Change in neutrophil-to-lymphocyte ratio (NLR) in response to immune checkpoint blockade for metastatic renal cell carcinoma. J Immunother Cancer. el 22 de enero de 2018;6:5. [ Links ]
17. Orditura M, Galizia G, Diana A, Saccone C, Cobellis L, Ventriglia J, et al. Neutrophil to lymphocyte ratio (NLR) for prediction of distant metastasis-free survival (DMFS) in early breast cancer: a propensity score-matched analysis. ESMO Open. el 1 de marzo de 2016;1(2):e000038. [ Links ]
18. Ou Q, Cheng J, Zhang L, Wang H, Wang W, Ma Y. The prognostic value of pretreatment neutrophil-to-lymphocyte ratio in breast cancer: Deleterious or advantageous? Tumor Biol. el 1 de junio de 2017;39(6):1010428317706214. [ Links ]
19. Ozyurek BA, Ozdemirel TS, Ozden SB, Erdogan Y, Kaplan B, Kaplan T. Prognostic Value of the Neutrophil to Lymphocyte Ratio (NLR) in Lung Cancer Cases. Asian Pac J Cancer Prev APJCP. 2017;18(5):1417-21. [ Links ]
20. Tang X, Du P, Yang Y. The clinical use of neutrophil-to-lymphocyte ratio in bladder cancer patients: a systematic review and meta-analysis. Int J Clin Oncol. el 1 de octubre de 2017;22(5):817-25. [ Links ]
21. Urrejola GI, Bambs CE, Espinoza MA, Gellona J, Zúñiga ÁM, Molina ME, et al. Un índice neutrófilo/linfocito elevado se asocia a peor pronóstico en cáncer de colon etapa II resecado. Rev Médica Chile. mayo de 2013;141(5):602-8. [ Links ]
22. Wang J, Jia Y, Wang N, Zhang X, Tan B, Zhang G, et al. The clinical significance of tumor-infiltrating neutrophils and neutrophil-to-CD8+ lymphocyte ratio in patients with resectable esophageal squamous cell carcinoma. J Transl Med. el 7 de enero de 2014;12:7. [ Links ]
23. Xue P, Kanai M, Mori Y, Nishimura T, Uza N, Kodama Y, et al. Neutrophil-tolymphocyte ratio for predicting palliative chemotherapy outcomes in advanced pancreatic cancer patients. Cancer Med. abril de 2014;3(2):406-15. [ Links ]
24. Beltrán BE, Castro D, De La Cruz-Vargas JA, Cotrina E, Gallo A, Sotomayor EM, et al. The neutrophil-lymphocyte ratio is prognostic in patients with early stage aggressive peripheral T cell lymphoma. Br J Haematol. febrero de 2019;184(4):650-3. [ Links ]
25. Szor DJ, Roncon Dias A, Pereira MA, Ramos MFKP, Zilberstein B, Cecconello I, et al. Neutrophil-lymphocyte ratio is associated with prognosis in patients who underwent potentially curative resection for gastric cancer. J Surg Oncol. abril de 2018;117(5):851-7. [ Links ]
26. He Q, Li G, Ji X, Ma L, Wang X, Li Y, et al. Impact of the immune cell population in peripheral blood on response and survival in patients receiving neoadjuvant chemotherapy for advanced gastric cancer. Tumor Biol. el 1 de mayo de 2017;39(5):1010428317697571. [ Links ]
27. NY Kim, D.-H. Chun, SY Kim et al., "Valor pronóstico de los índices inflamatorios sistémicos, NLR, PLR y MPV, para predecir la supervivencia a 1 año de pacientes sometidos a cirugía citorreductora con HIPEC", Journal of Clinical Medicine , vol. 8, no. 5, p. 589, 2019.Ver en: sitio del editor | Google Académico [ Links ]
28. Deng Q, He B, Liu X, Yue J, Ying H, Pan Y, et al. Prognostic value of pre-operative inflammatory response biomarkers in gastric cancer patients and the construction of a predictive model. J Transl Med [Internet]. el 18 de febrero de 2015 [citado el 14 de enero de 2019];13. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC4343078/ [ Links ]
29. Jhony A. De La Cruz-Vargas, Lucy E. Correa Lopez, Maria del Socorro Alatrista Gutierrez de Bambaren, Hector Sanchez Carlessi, Consuelo Luna Muñoz, Maria Loo Valverde, et all. Promoting research in medical students and increasing scientific production in universities: Experience of the Undergraduate Thesis Workshop Course. Educacion Medica, Volume 20, Issue 4, July-August 2019, Pages 199-205. https://doi.org/10.1016/j.edumed.2018.06.003 [ Links ]
30. CI Diakos, KA Charles, DC McMillan y SJ Clarke, "Inflamación relacionada con el cáncer y efectividad del tratamiento", The Lancet Oncology , vol. 15, no. 11, págs. E493 - e503, 2014.Ver en: sitio del editor | Google Académico [ Links ]
31. RD Dolan, BJA Laird, PG Horgan y D. McMillan, "El valor pronóstico de la respuesta inflamatoria sistémica en ensayos clínicos aleatorizados en cáncer: una revisión sistemática", Critical Reviews in Oncology / Hematology , vol. 132, págs. 130-137, 2018.Ver en: sitio del editor | Google Académico [ Links ]
32. RD Dolan, ST McSorley, PG Horgan, B. Laird y DC McMillan, "El papel de la respuesta inflamatoria sistémica en la predicción de resultados en pacientes con cáncer inoperable avanzado: revisión sistemática y metaanálisis ", Critical Reviews in Oncology / Hematology , vol. 116, pp. 134-146, 2017.Ver en: sitio del editor | Google Académico [ Links ]
33. H. Kuper, W. Ye, U. Broomé et al., "El riesgo de cáncer de hígado y de vías biliares en pacientes con hepatitis viral crónica, alcoholismo o cirrosis" , Hepatology , vol. 34, no. 4, págs. 714-718, 2001.Ver en: Sitio del editor | Google Académico [ Links ]
34. J. Candido y T. Hagemann, "Inflamación relacionada con el cáncer", Journal of Clinical Immunology , vol. 33, Suplemento 1, págs. 79-84, 2013.Ver en: Sitio del editor | Google Académico [ Links ]
35. T. Wu, B. Cheng y L. Fu, "Aplicaciones clínicas de las células tumorales circulantes en farmacoterapia: desafíos y perspectivas", Molecular Pharmacology , vol. 92, no. 3, págs. 232-239, 2017.Ver en: Sitio del editor | Google Académico [ Links ]
36. Z. Shen, A. Wu y X. Chen, "Tecnologías de detección actuales para las células tumorales circulantes", Chemical Society Reviews , vol. 46, no. 8, págs. 2038-2056, 2017.Ver en: sitio del editor | Google Académico [ Links ]
37. Z. Zhu, S. Qiu, K. Shao e Y. Hou, "Progreso y desafíos de secuenciar y analizar las células tumorales circulantes", Cell Biology and Toxicology , vol. 34, no. 5, págs. 405-415, 2018.Ver en: Sitio del editor | Google Académico [ Links ]
38. A. Dasgupta, AR Lim y CM Ghajar, "Células tumorales circulantes y diseminadas: ¿heraldos o iniciadores de metástasis?" Oncología Molecular , vol. 11, no. 1, págs. 40-61, 2017.Ver en: Sitio del editor | Google Académico [ Links ]
39. DS Micalizzi, S. Maheswaran y DA Haber, "Un conducto a la metástasis: biología celular tumoral circulante", Genes & Development , vol. 31, no. 18, págs. 1827-1840, 2017.Ver en: Sitio del editor | Google Académico [ Links ]
40. TJ Li, YM Jiang, YF Hu et al., "Los neutrófilos productores de interleucina-17 vinculan los estímulos inflamatorios con la progresión de la enfermedad al promover la angiogénesis en el cáncer gástrico", Clinical Cancer Research , vol. 23, no. 6, págs. 1575-1585, 2017.Ver en: Sitio del editor | Google Académico [ Links ]
41. NE Burr, MA Hull y V. Subramanian, "¿El uso de medicamentos antiinflamatorios no esteroideos con aspirina o sin aspirina previene el cáncer colorrectal en la enfermedad inflamatoria intestinal?" World Journal of Gastroenterology , vol. 22, no. 13, págs. 3679-3686, 2016.Ver en: Sitio del editor |Google Académico [ Links ]
42. J. Pillay, I. den Braber, N. Vrisekoop et al., "El marcado in vivo con 2H2O revela una vida útil de neutrófilos humanos de 5,4 días" , Blood , vol. 116, no. 4, págs. 625-627, 2010.Ver en: Sitio del editor | Google Académico [ Links ]
43. W. Liang y N. Ferrara, "El papel complejo de los neutrófilos en la angiogénesis y metástasis tumorales", Cancer Immunology Research , vol. 4, no. 2, págs. 83-91, 2016.Ver en: Sitio del editor |Google Académico [ Links ]
44. A. Swierczak, KA Mouchemore, JA Hamilton y RL Anderson, "Neutrófilos: contribuyentes importantes para la progresión tumoral y la metástasis", Cancer Metastasis Reviews , vol. 34, no. 4, págs. 735-751, 2015.Ver en: sitio del editor | Google Académico [ Links ]
45. R. Ogiya, N. Niikura, N. Kumaki et al., "Comparación de linfocitos infiltrantes de tumores entre tumores primarios y metastásicos en pacientes con cáncer de mama", Cancer Science , vol. 107, no. 12, págs. 1730-1735, 2016.Ver en: sitio del editor | Google Académico [ Links ]
46. Fang T, Wang Y, Yin X, Zhai Z, Zhang Y, Yang Y, You Q, Li Z, Ma Y, Li C, Song H, Shi H, Zhang Y, Yu X, Gao H, Sun Y, Xie R, Xue Y. Diagnostic Sensitivity of NLR and PLR in Early Diagnosis of Gastric Cancer. J Immunol Res. 2020 Mar 7;2020:9146042. doi: 10.1155/2020/9146042. PMID: 32211444; PMCID: PMC7081040. [ Links ]
Received: December 16, 2019; Accepted: March 30, 2020











 texto en
texto en