Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.20 no.4 Lima oct./dic 2020
http://dx.doi.org/10.25176/rfmh.v20i4.2873
Original Article
The comparison of APACHE II and BISAP scales in the prognosis of acute pancreatitis in a hospital in Peru
1Servicio de Medicina Interna y Unidad de Cuidados Intensivos, Hospital María Auxiliadora, Lima-Perú.
2Facultad de Medicina, Universidad Ricardo Palma, Lima - Perú.
3Instituto de Investigación de Ciencias Biomédicas, Universidad Ricardo Palma, Lima - Perú.
Introduction:
Acute pancreatitis continue to be a disease with significant morbidity and mortality. It is diagnosed by clinical criteria and the inflammatory process can lead to organ failure.
Objective:
This study compared the APACHE II and BISAP scales in organ failure development in patients with acute pancreatitis from a public hospital in Peru.
Methods:
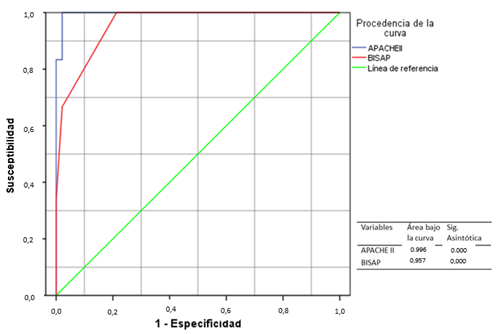
A diagnostic test validation study was carried out. The medical records of patients hospitalized with the diagnosis of acute pancreatitis in the Internal Medicine service and the Intensive Care Unit were evaluated. The APACHE II and BISAP scales were applied, the ROC curve, sensitivity, specificity, positive and negative predictive value were calculated. SPSSv23 was used for statistical analysis.
Results:
146 patient records that met the inclusion criteria were evaluated. An area under the curve of 0.957 was obtained for BISAP and 0.996 for APACHE II. It had a sensitivity and specificity for APACHE II of 83% and 99%, for BISAP of 66% and 99%. The positive and negative predictive value for APACHE II is 83% and 99%, and for BISAP 80% and 98%.
Conclusion:
The APACHE II scale was superior to detect organ failure. It was determined that both scales have high specificity, the sensitivity being more significant in the BISAP scale.
Keywords: Acute pancreatitis; Organ failure
INTRODUCTION
In 2015 in the United States, pancreatitis was the third cause of the most frequent hospital admissions, presenting a worldwide incidence that ranges from 4.9 - 73.4 x 100,000 inhabitants1. Most patients present mild symptoms, and severe conditions can present up to a mortality rate of 20%2. Organ failure is the main cause and determinant of severity and early mortality, while late deaths are due to secondary infections, including infected pancreatic necrosis and sepsis3.
In a study carried out in Mexico, there was 80% mild pancreatitis and a mortality rate of severe pancreatitis of 25% to 30%4. In another study, biliary etiology was the most frequent (66%), followed by alcoholic (15%)5. It has been described that the incidence varies according to alcohol consumption and the presence of gallstones6.
In Peru, there are few studies on this pathology; the Ministry of Health published a study in which the incidence was 28 cases per 100 000 inhabitants7. Other authors showed that the most frequent etiology was biliary, reaching 80-100% in some centers,8the second cause was alcohol, followed by dyslipidemias, and others. The ability to predict the severity and mortality of pancreatitis will help the clinician screen patients with increased morbidity and mortality risk. Several severity rating scales are used, such as APACHE II, BISAP, and RANSON. These can be useful to institute appropriate and timely therapeutic strategies, providing information on the patient's status upon admission and in the first 24 or 48 hours, depending on the scale9,10.
Due to those mentioned above, this study’s objective was to compare the APACHE II and BISAP scales in the prognosis of organ failure in hospitalized patients with acute pancreatitis in a public hospital in Peru.
METHODS
Design and study area study
A diagnostic test validation was carried out and analytical, comparing the PACHE II and BISAP scales’ predictive power in the development of organ failure in acute pancreatitis, considering the new Atlanta classification of the Service of Internal Medicine and Intensive Care Unit of the Hospital María Auxiliadora in 2017, Lima-Peru.
Population and sample
The medical records of patients with a diagnosis of acute pancreatitis, over 18 years of age, hospitalized were reviewed and included, pregnant patients, a history of chronic pancreatitis. Patients seen in the outpatient clinic, and with another associated pathology were excluded acute pancreatitis. It conditions a state of sepsis or increases their hospital stay, such as chronic renal failure, heart disease, COPD, HIV, oncological diseases, and patients who requested their voluntary withdrawal or the datasheet was incomplete.
Variables and Instruments
Concerning the APACHE II scale, several authors take the value of 8 as the cut-off point. Gompertz11carried out a study where he raised the cut-off point requirement from 8 to a cut-off point of 12, obtaining the more certain prediction of complications and mortality. Therefore, this work was decided to take a score greater than 12 to develop organic failure. Likewise, for the BISAP scale, the value of 3 was taken to determine the development of organ failure and the prognosis of the disease12.
Statistic analysis
The SPSS version 23.0 program was used to process the collected data. The ROC curve, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of both scales were calculated to evaluate organ failure risk.
Ethical aspects
This study complies with current regulations on clinical and bioethical research. The authorization was obtained from the Institutional Ethics and Research Committee of the María Auxiliadora Hospital and the Research Institute’s approval in Biomedical Sciences of the Ricardo Palma University. The medical records were consulted, preserving the confidentiality and privacy of the patients. The present work does not evaluate the therapeutic intervention, nor does it present images or personal data that allow patients to be identified.
RESULTS
We included 146 patients diagnosed with acute pancreatitis who met the inclusion criteria.Table 1shows demographic, clinical characteristics, and laboratory data. The average age of 44.2 years was observed; it was more frequent in females with 67.1%. The average hospitalization days were 6 days2,17. Similarly, in the background, 17 patients (11.6%) with Type 2 Diabetes Mellitus were evidenced, and 5 patients (3.4%) had cholecystectomy before acute pancreatitis.
Table 1. Frecuencia de las características clínicas, demográficas y datos de laboratorio
| Variables | Number / Mean | Percentage / Interval |
|---|---|---|
| Age (years) | 44,3 | 41,7 - 46.9 |
| Days of hospitalization | 6,4 | 5,6 - 7.2 |
| Gender | ||
| Female | 98 | 67.1 % |
| Male | 48 | 32.8% |
| Diabetes Type 2 | 17 | 11.6 % |
| Previous cholecystectomy | 5 | 3.4% |
| Previous acute pancreatitis | 10 | 6.8% |
| Etiology | ||
| Biliary | 131 | 89.7% |
| Alcohol | 9 | 6.16% |
| Post ERCP | 2 | 1.4% |
| Dyslipidemias | 3 | 2.1% |
| Others | 1 | 0.7% |
| Laboratory | ||
| Hematocrit % | 36 | 34,6 - 39,3 |
| Leukocytes /ul | 11247 | 9658.5-12258.6 |
| Amylase /ul | 1594 | 1414,5 - 1775 |
| Lipase /ul | 1183 | 1002,0 - 1365,7 |
The distribution according to etiology of acute pancreatitis was: mainly biliary in 131 patients (89.7%), followed by alcohol consumption in 9 patients (6 %), post-ERCP acute pancreatitis (second and third day) in 2 patients (1.4%), dyslipidemia in 3 patients (2.1%) and 1 patient (0.7%) due to idiopathic causes.
The mean hematocrit was 36% within the laboratory tests, and for leukocytes, it was approximately 13000 / ul. The average amylase and lipase were 1594 / ul and 1183 / ul, respectively.
The degrees of severity and organ failure of the APACHE II and BISAP scales were evaluated and are shown inTable 2. For the APACHE II scale, a score greater than or equal to 12 was considered for the detection of organ failure, obtaining 6 patients who had this diagnosis while for the BISAP scale, the cut-off point was 3, obtaining 4 patients with organ failure and two other patients were found below this cut-off.
Table 2. Grades of severity and organ failure according to the APACHE II and BISAP.
| Scales | Number (Percentage) | Organic Failure (Number) |
|---|---|---|
| APACHE II | 3.11 (2.5-3.6) | 0 |
| < 8 | 133 (91%) | 0 |
| 8 | 2 (1.4%) | 0 |
| 9 | 3 (2.1%) | 0 |
| 10 | 1 (0.7%) | 0 |
| 11 | 1 (0.7%) | 0 |
| >=12 | 6 (4.1%) | 6 |
| BISAP | ||
| 0 | 87 (59%) | 0 |
| 1 | 43 (29%) | 0 |
| 2 | 11 (7.5%) | 2 |
| 3 | 3 (2.1%) | 2 |
| 4 | 2 (1.4%) | 2 |
| 5 | 0 (0%) | 0 |
An area under the curve of 0.996 for the APACHE II scale and 0.957 for the BISAP scale, both with a p = 0.000.Figure 1. The sensitivity and specificity for APACHE II were 83% and 99%, while for BISAP, it was 66% and 99%.Table 3.
The days of hospitalization of patients with acute pancreatitis evaluated with the APACHE II and BISAP scales are represented inTable 4.
Table 3. Assessment of the APACHE scales II and BISAP
| Assessment of Tests | APACHE II | BISAP |
|---|---|---|
| Sensitivity | 83% | 66% |
| Specificity | 99% | 99% |
| Positive Predictive Value | 83% | 80% |
| Negative Predictive Value | 99% | 98% |
Table 4. Days of hospitalization for the APACHE II and BISAP scales
| BISAP SCORE | APACHE II SCORE | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | Total | <8 | 8 | 9 | 10 | 11 | >=12 | Total | ||||
| Days of Hospitalization | 2 | 3 | 0 | 0 | 0 | 0 | 3 | Days of Hospitalization | 2 | 3 | 0 | 0 | 0 | 0 | 0 | 3 |
| 3 | 25 | 3 | 0 | 0 | 0 | 28 | 3 | 28 | 0 | 0 | 0 | 0 | 0 | 28 | ||
| 4 | 21 | 10 | 0 | 0 | 0 | 31 | 4 | 31 | 0 | 0 | 0 | 0 | 0 | 31 | ||
| 5 | 17 | 5 | 1 | 0 | 0 | 23 | 5 | 23 | 0 | 0 | 0 | 0 | 0 | 23 | ||
| 6 | 8 | 6 | 0 | 0 | 0 | 14 | 6 | 13 | 0 | 1 | 0 | 0 | 0 | 14 | ||
| 7 | 6 | 8 | 3 | 1 | 0 | 18 | 7 | 14 | 2 | 1 | 0 | 0 | 1 | 18 | ||
| 8 | 0 | 4 | 2 | 0 | 0 | 5 | 8 | 3 | 0 | 1 | 0 | 0 | 1 | 5 | ||
| 9 | 3 | 3 | 0 | 0 | 0 | 6 | 9 | 5 | 0 | 0 | 1 | 0 | 0 | 6 | ||
| 10 | 1 | 1 | 1 | 0 | 0 | 3 | 10 | 3 | 0 | 0 | 0 | 0 | 0 | 3 | ||
| 11 | 0 | 1 | 2 | 0 | 0 | 3 | 11 | 3 | 0 | 0 | 0 | 0 | 0 | 3 | ||
| 12 | 1 | 1 | 1 | 0 | 0 | 3 | 12 | 3 | 0 | 0 | 0 | 0 | 0 | 3 | ||
| 13 | 0 | 1 | 1 | 0 | 0 | 1 | 13 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | ||
| 15 | 0 | 0 | 0 | 0 | 1 | 2 | 15 | 0 | 0 | 0 | 0 | 1 | 1 | 2 | ||
| 17 | 0 | 1 | 0 | 0 | 0 | 1 | 17 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | ||
| 18 | 1 | 0 | 0 | 0 | 0 | 1 | 18 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | ||
| 20 | 1 | 0 | 0 | 0 | 1 | 2 | 20 | 1 | 0 | 0 | 0 | 0 | 1 | 2 | ||
| 25 | 0 | 0 | 0 | 1 | 0 | 1 | 25 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | ||
| 27 | 0 | 0 | 0 | 1 | 0 | 1 | 27 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | ||
| Total | 87 | 44 | 13 | 6 | 6 | 146 | 133 | 2 | 3 | 1 | 1 | 6 | 146 | |||
DISCUSSION
Acute pancreatitis presents an unpredictable clinical course from patients with few symptoms to patients with high mortality; leading to a search for highly effective severity scales to predict severity and mortality that are accessible, easy to use and cheap for vigorous therapeutic intervention13.
This study found 98 female patients (67.1%) and 48 male (32.8%) with an average age of 44.25 years with values within a range of 41.65- 46.85, similar results were found by other authors regarding these characteristics of the population14,15.
According to the etiology of pancreatitis, biliary, and alcoholic predominate in 89.7% and 6% respectively, our results are similar or reported by other investigations, of 75% and 7% respectively16,17.
In the present validation study, organ failure in acute pancreatitis was considered according to the new Atlanta 2012 classification. Regarding the severity indexes, the majority of acute pancreatitis were mild. In the case of the BISAP scale, about 89% presented a score of 0 or 1, with a score of 3, 4 patients were classified with organ failure, no patients with a score of 5. In the APACHE II scale, the cut-off point of 8 was taken as a cut-off point for this research to classify it as a mild condition, with 91% of the patients being in this category. On the other hand, a value of 12 was taken to qualify it as a severe condition, 6 patients with this score presented organ failure. No deaths were recorded. These findings are similar to those found by Aguilar Gaibor in 2016 in Ecuador, who reported 85% of cases of mild acute pancreatitis and 14.2% of severe cases9.
It is essential to validate these scales to detect organ failure early and start with the appropriate treatment, which will be different for the severity of the condition; It can be seen that the BISAP scale (99%) and APACHE II (99%) have high specificity for acute pancreatitis. However, the APACHE II scale (83%) has greater sensitivity than the BISAP scale (66%) to detect organ failure in acute pancreatitis patients. In the same way, Alvarado, in 2017, Peru carried out the study "Utility of the BISAP and APACHE II scores as predictors of severity of acute pancreatitis," where he demonstrated that the APACHE II scale was a better predictor than the BISAP scale for organ failure. In this study, the value of 8 for the APACHE II scale and 2 for the BISAPscale was taken to develop organ failure18.
In our work, it was observed that the negative predictive value was high for both scales close to 100%, in addition to the positive predictive value, their results were similar, presenting the APACHE II scale with a minimal difference, showing that the probability of detecting failure of organs in acute pancreatitis having a score equal to or greater than 12 is higher than having a score greater than or equal to 3 on the BISAP scale. The results were similar in the Gompertz study; where most patients have mild symptoms of this disease, they conclude that the BISAP score ≥ 3 has a PPV: 88.33% and NPV: 98.36%11. However, in his study, Alvarado found for the BISAP <2 scales a PPV: 36.36% and NPV: 91.26%; for the APACHE II scale> 9, he found a PPV: 55.17% and an NPV: 95.33%(18). The difference in the various studies results is due to the cut-off point used in the scale.
Both scales studied have a similar area under the curve (APACHE II: 0.996, BISAP: 0.957 both with a p = 0.000), the APACHE II scale being the one with the most significant power to detect the prognosis of this disease. The area under the curve of the BISAP scale is comparable with the results of other studies such as Barcia (0.918)17, Gompertz (0,98)11, Aguilar (0,94)9. The BISAP scale is suitable for predicting organ failure in patients with acute pancreatitis.
Most of the patients had mild acute pancreatitis, and this is correlated with a short hospital stay. However, the patients who developed a severe picture of acute pancreatitis had a prolonged hospital stay, related to organ failure. This is consistent with the result in the Gompertz study11.
The study’s main limitation is the low frequency of severe acute pancreatitis, making the predictive power for severity limited. Still, it has a high negative predictive value to rule out organ failure. However, failure prediction should be used with caution in clinical practice, always paying attention to other clinical signs that patients may present.
A multicenter study must be carried out in the future perspective, with greater statistical power to confirm our results.
CONCLUSION
In our study, the APACHE II scale was superior in predicting and detecting organ failure. It was determined that both scales have high specificity; however, the APACHE II scale presented greater sensitivity than the BISAP scale. The severity of acute pancreatitis is correlated with a hospital stay.
REFERENCES
1. Peery AF, Crockett SD, Barritt AS, et al. Burden of Gastrointestinal, Liver, and Pancreatic Diseases in the United States. Gastroenterology. 2015;149:1731-1741. doi:10.1053/j.gastro.2015.08.045. [ Links ]
2. Kumar AH, Griwan MS. A comparison of APACHE II, BISAP, Ranson’s score and modified CTSI in predicting the severity of acute pancreatitis based on the 2012 revised Atlanta Classification. Gastroenterol Rep. 2018; 6:127-31. doi:10.1093/gastro/gox029 [ Links ]
3. Dumnicka P, Maduzia D, Ceranowicz P, Olszanecki R, Drozd R, Kuśnierz-Cabala B. The Interplay between Inflammation, Coagulation and Endothelial Injury in the Early Phase of Acute Pancreatitis: Clinical Implications. Int. J. Mol. Sci. 2017; 17(2): 1-25; doi:10.3390/ijms18020354. [ Links ]
4. González-González JA, Castañeda-Sepúlveda R, Martínez-Vázquez MA, et al. Características clínicas de la pancreatitis aguda en México. Rev Gastroenterol Mex. 2012;77:167-173. doi : 10.1016/j.rgmx.2012.08.002 [ Links ]
5. Gonzales Gonzales J, Castañeda Sepúlveda R, Martínez Vazquez M, et al. Características clínicas de la pancreatitis aguda en México. Rev Gastroenterol Mex. 2012;77:167-73. doi:10.1016/j.rgmx.2012.08.002. [ Links ]
6. Madaria E, Martinez J. Páncreas y vías biliares. In: Montoro M, García J, editors. Unidad Patol. Pancreática. Unidad Gastroenterol. y Endosc. Dig. Segunda Edicion, Madrid: Asociación Española de Gastroenterología; 2012, p. 627-44. [ Links ]
7. Ministerio de Salud. Perfil epidemiológico de pacientes en consulta externa y hospitalización. MINSA. Lima- Perú. 2009. [ Links ]
8. Gompertz M, Lara I, Fernández L, et al. Mortalidad de la pancreatitis aguda: experiencia de 20 años en el Hospital Clínico Universidad de Chile. Rev. méd. Chile 2013; 141: 562-567. http://dx.doi.org/10.4067/S0034-98872013000500002 [ Links ]
9. Aguilar Gaibor CI, Salamea Molina JC, TenezacaTacuri Á. Eficacia de la Escala BISAP para Predicción Temprana de Severidad en Pancreatitis Aguda Biliar. Hospital Vicente Corral Moscoso. Enero 2014 - Julio 2015. Rev Médica Del Hosp José Carrasco Arteaga. 2016;8:148-53. doi:10.14410/2016.8.2.ao.24 [ Links ]
10. Hong W, Lillemoe KD, Pan S, Vincent Zimmer, et al. Development and validation of a risk prediction score for severe acute pancreatitis. J Transl Med. 2019; 17: 146. doi.org/10.1186%2Fs12967-019-1903-6. [ Links ]
11. Gompertz M, Fernández L, Lara I, et al . Índice clínico de gravedad en pancreatitis aguda: BISAP (“Bedside Index for Severity in Acute Pancreatitis”). Dos años de experiencia en el Hospital Clínico Universidad de Chile. Rev Med Chil. 2012;140:977-83. doi:10.4067/S0034-98872012000800002. [ Links ]
12. Murillo Zolezzi A, Murakami Morishige P, Toledo Vargas SA, et al. Evaluación de la escala de BISAP en el pronóstico de la pancreatitis aguda. Rev Chil Cirugía. 2010; 62:465-9. doi:10.4067/s0718-40262010000500007 [ Links ]
13. Surco Y, Huerta Mercado J, Pinto J, Piscoya A, De Los Ríos R, et al. Predicción Precoz de Severidad en Pancreatitis Aguda. Rev. Gastroenterol. Perú; 2012; 32-3: 241-250. www.scielo.org.pe › scielo › pid=S1022-51292012000300002. [ Links ]
14. Pérez Campos A, Bravo Paredes E, Prochazka Zarate R, Bussalleu A, Pinto Valdivia J, Valenzuela Granados V. BISAP-O y APACHE-O: utilidad en la predicción de severidad en la pancreatitis aguda según la clasificación modificada de Atlanta. Rev Gastroenterol Perú. 2015;35(1):15-24. http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1022-51292015000100002 [ Links ]
15. Villacís X, Calle P, Patiño J, Calle G. Validación del Score de BISAP como Sistema Pronóstico en Pancreatitis Aguda. Rev. Gastroenterol. Perú; 2011; 31-3: 230-235.http://dev.scielo.org.pe/scielo.php?script=sci_abstract&pid=S1022-51292011000300005&lng=es&nrm=iso&tlng=es [ Links ]
16. Singhi AD, Koay EJ, Chari ST, et al. Early Detection of Pancreatic Cancer: Opportunities and Challenges. Gastroenterology 2019;156:2024-2040. https://doi.org/10.1053/j.gastro.2019.01.259 [ Links ]
17. Barcía Velásquez CA, Felix Mena MA. Estudio comparativo entre las escalas Apache II , Bisap y Marshall modificado en la evaluación del estado de aguda en el Servicio de Emergencia del Hospital San Francisco de Quito . Pontificia Universidad Católica del Ecuador. 2016. [Consultado el 22 de Octubre del 2018].http://repositorio.puce.edu.ec/bitstream/handle/22000/10479/TESIS%20DE%20GRADO%20PDF.pdf?sequence=1&isAllowed=y [ Links ]
18. Alvarado Gutierrez F. Utilidad de los puntajes BISAP y APACHE II como predictores de severidad de pancreatitis aguda en pacientes del Hospital Nacional Dos de Mayo. Universidad Mayor de San Marcos, 2017. [Consultado el 3 de Noviembre del 2018]. http://cybertesis.unmsm.edu.pe/handle/cybertesis/6125 [ Links ]
Received: November 15, 2019; Accepted: August 15, 2020











 texto en
texto en