Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.20 no.4 Lima oct./dic 2020
http://dx.doi.org/10.25176/rfmh.v20i4.3221
Clinical case
Uncommon onset Escherichia Coli sepsis in t-cell and nk lymphoma patient
1Universidad Ricardo Palma, Facultad de Medicina Humana “Manuel Huamán Guerrero”, Lima-Perú.
2Sociedad Científica de Estudiantes de Medicina de la Universidad Ricardo Palma, Lima-Perú.
3Instituto de Investigación de Ciencias Biomédicas, Universidad Ricardo Palma, Lima-Perú.
4Hospital María Auxiliadora, Lima-Perú.
Sepsis occurs in the presence of an infectious focus; in this case by Escherichia coli (E.coli), which have toxins that can cause severe damage to the functionality and morphology of the organism, being worsened in patients with diseases that affect the immune system; as is this case in the presence of hematological neoplasia. A 42-year-old female patient diagnosed with NK-T-cell non-Hodgkin lymphoma, presents a necrotic plaque on the palate, temperature above 38 ° C, a respiratory rate exceeding 20 breaths per minute, and heart rate exceeding 90 beats per minute, upon examination of a positive pharyngeal culture for E.coli, negative urine culture, confirming the pharyngeal infectious starting point; treated with mikacin intravenously for 7 days with good response to antibiotic therapy. A rare case of this type of bacteria is reported in the oral area, and the subject is reviewed.
Key words: Sepsis; Lymphoma; Extranodal NK-T-Cell; Necrosis (Source: MeSH NLM).
INTRODUCTION
This report’s objective seeks to report on a rare case of sepsis originating in the palate by E. coli in a patient with Extranodal T / NK Cell Lymphoma, since it is usually of urinary origin in these patients, as will be explained later.
Non-Hodgkin's lymphoma (NHL) is a malignant neoplasm that mainly affects the lymphatic system, which frequently extends to extranodal sites1. In most cases, it usually affects B lymphocytes intranodal by 90% and 10% in T cells and Natural Killer (NK-t). It is a very aggressive and rare specific type of lymphoma that usually manifests in the upper airway and digestive tract (pharynx, mouth, nasal cavity, paranasal sinuses, among others), due to its rarity, requires specialized treatment2.
According to the National Institute of Neoplastic Diseases (INEN) in Peru, each year, around 2,000 new cases of cancer are diagnosed, and in Metropolitan Lima, the incidence rate of lymphoma is 10 cases per 100,000 healthy inhabitants, representing 5% of the total of malignant neoplasms; It is a heterogeneous group of cancers of the immune system in T cells or B cells characterized by its accelerated spread, and it is estimated that at 75 years of age, 1 in 80 men in Metropolitan Lima will have this disease.3
In recent years the National Institute of Statistics and Informatics (INEI) determined that of around 7000 people; 150 present NHL with localization in the oral cavity and pharynx, in both men and women.4,5
Of all primary cutaneous lymphomas in Peru, nasal-type T-NK lymphoma represents 1.49%, according to some research carried out in our country6.
The infections associated with this type of rare and uncommon lymphoma vary according to the place. If we speak of pharynx-tonsil focus, the most frequent is to find streptococci present, but not Escherichia coli (E. coli), which can trigger urgent sepsis to be treated before of the respective treatment for the underlying pathology. That is why we report the following case as a clinical contribution7-10.
PRESENTATION OF THE CASE A
A 42-year-old female patient from Lima, with a diagnosis of T-NK NHL by pathological anatomy of palate biopsy: palatal mucosa with atypical lymphoid infiltrate; immunohistochemistry: Nasal type T / NK Cell Lymphoma (CD3 +, BVS +, CD56 +, CD8 +, CD4 +, Ki-67: 70%), who is hospitalized in the medical oncology service, after presenting in an outpatient clinic presenting a lesion of 8 x 5 cm on the palate (Figura 1), which involves the tonsillar region, also giving purulent secretions; necrotic in appearance, progressive growth, malodorous. When taking his temperature, he gave a 38 ° C fever peak, he presented dysphagia to solids and partially to liquids, nocturnal diaphoresis.

Figure 1. 42-year-old female patient with a foul-smelling necrotic palate lesion measuring approximately 8 x 5 cm, evident on oropharyngeal examination.
The work plan requested was: hemogram, biochemistry, tumor lysis profile (serum electrolytes, uric acid, phosphorus, calcium, and magnesium), HTLV, HIV, hepatotropic virus, Epstein Barr virus (EVB) profile, BK serial sputum-urine-stool, β2 microglobulin, 2 blood cultures, sputum culture, pharyngeal culture, urine culture, and tomography of the head, neck, paranasal sinuses, chest, and abdomen.
Among the auxiliary examinations of highlighted images presented, thickening of the mucosa in ethmoid cells, a radiolucent image in the upper palate (Figura 2), slight adenopathy at the retromandibular level (Figura 3), thickening of the mucosa of both maxillary sinuses, and thickening of the middle turbinate, there is a slight deviation to the left of the nasal septum (Figura 4), in the axial tomography of the head-lower part, a radiopaque image is appreciated in the left area of the palate, consistent with the necrosis evidenced in the physical examination , there is evidence of the presence of contrast hyper-uptake nodules and the presence of small adenopathies (Figura 5).

Figure 2. Sagittal head tomography with contrast showing thickening in the mucosa of the ethmoid cells, lucid radio image in the upper palate corresponding to the necrotic area described in the physical examination, no lymphadenopathy is appreciated.
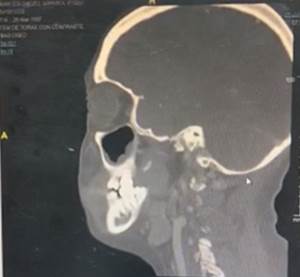
Figure 3. Parasagittal head tomography with contrast, showing thickening of the lower mucosa of the right maxillary paranasal sinus, slight lymphadenopathy at the retromandibular level is no damage to nervous tissue.
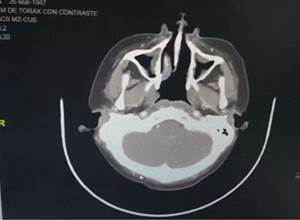
Figure 4. Head-upper axial tomography, evidence of thickening of the mucous membranes of both maxillary sinuses and thickening of the middle turbinate, there is a slight deviation to the left of the nasal septum, the slight circular radiopaque image on the anterior face of the right cerebellar peduncle ; no lymphadenopathy is seen.
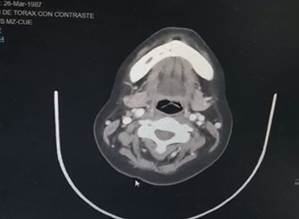
Figure 5. Axial head tomography, lower part, a radiopaque image is appreciated in the palate’s left area, consistent with the necrosis evidenced in the physical examination, the presence of hyper-contrast-uptake nodules, the presence of adenopathies.
At the end of the coronal tomographic reconstruction, slight hepato-splenomegaly, presence of nodulations in the mesogastrium and left iliac fossa, no metastases at the liver or lung level (Figura 6) that could complicate the infectious picture.
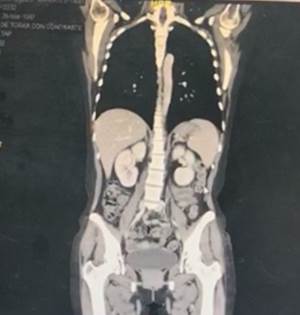
Figure 6. Coronal tomographic reconstruction, slight hepato-splenomegaly, enlarged uterus, presence of nodulations in the mesogastrium and left iliac fossa, kidneys without obvious involvement, bladder with radiopaque content, no evidence of muscle damage.
Laboratory tests did not reveal leukocytosis (leukocytes: 8.80 x 103 / ul), hemoglobin 9.6 g / dl, platelets in normal values: 268 x 103 / ul; HTLV, HIV, negative hepatotropic viruses; EBV EA IgG, EBV VCA IgG Antibody and EBV EBNA IgG reactive, EBV VCA IgM non-reactive, b2 microglobulin 3.04 mg / L elevated (serum VN 0.80-2.34): BK in serial sputum, urine and stool negative; liver profile and tumor lysis profile in normal values. During his hospitalization days, he continued to present fever peaks between 38 and 39 ° C, tachypnea, and an increase in heart rate, maintaining values above 90 beats per minute, without a pathological blood count or any change in the biochemistry or tumor lysis profile. Negative urine culture, negative blood culture, the sputum culture shows the presence of Candida albicans.
The result of the pharyngeal secretion culture was positive for Escherichia Coli resistant to ampicillin, cefepime, cefuroxime, ciprofloxacin, fosfomycin, and trimethoprim/sulfamethoxazole.
The diagnostic criteria of sepsis must take into account the presence of an infectious focus and several parameters (general, inflammatory, hemodynamic, tissue perfusion, organ dysfunction, among others); various scores can be used (qSOFA, SOFA, SIRS, etc.); In this case, it was evaluated using the Systemic Inflammatory Response Syndrome (SIRS) criteria, which have as criteria: Temperature (> 38 ° C or <36 ° C), respiratory rate (> 20rpm or PaCO2 <32 mmHg), frequency cardiac (> 90 bpm) and Leukocytes (> 12000 / mm3 or <4000 / mm3); It is necessary to meet at least 2 of these criteria and an infectious focus to be considered as sepsis.12,13
The treatment chosen to counteract sepsis was amikacin 1g every 24 hours intravenously according to the pharyngeal culture’s sensitivity, for 7 days, and medications to relieve symptoms.
The signs and symptoms related to sepsis progressively decreased over the days. The patient achieved clinical improvement with the negative pharyngeal culture after 7 days of antibiotic treatment. With this, she remained hospitalized to continue her basic treatment for T-lymphoma. NK. The signs and symptoms related to sepsis progressively decreased over the days, after which the patient remained hospitalized to continue her specific therapy for lymphoma.
DISCUSSION
Nasal-type extranodal T / NK lymphoma is an aggressive non-Hodgkin group lymphoma, and its response to treatment is very poor. It represents less than 15% of NHL, and in which some epidemiological studies have revealed that it occurs more in Asian countries than Western countries (0.2% of neoplasms)1-3. At present, LC-T / NK represents 1.49% of extranodal lymphomas in Peru. Its etiology is not determined; however, it is closely related to EBV, suggesting an etiopathogenic role. Our patient presents additional tests for EBV, suggesting an active infection by said virus 2. The most frequent presentation is usually in males (3/1). In the fifth decade of life, quite the opposite of our case, which was a young female patient, which is infrequent and implies individualizing the way of acting.
This pathology affects structures mainly in the upper aerodigestive tract; paranasal fossa and sinuses, nasopharynx, oropharynx, oral cavity, and palate already described in the report2,3,5.
The clinical examination suggests excluding other infectious diseases such as histoplasmosis, blastomycosis,paracoccidioidomycosis, leprosy, tuberculosis, Wegner's disease, leishmania, rhinoscleroma, and other neoplasms2,7.
The incidence of infection in non-Hodgkin lymphomas, with a higher prevalence than Hodking lymphoma, due to nosocomial infection can be 29.6% in which cases it increases for the time they remain hospitalized, for which the authors Ruiz and Guzmán AC et al. (Mexico) mention that the largest number of cases for the type of infection that occurs in malignant hematological diseases with a total of 10 confirmed cases correspond to E. coli as the cause of infections7, considering that the prevalence of infections alters depending on the place, this figure is close to infections by enterobacteria according to Catalanapiedra Barbosa M. (Valladollid)8, in the same way, it is confirmed by Arroyo-Peña T, et al. (Bolivia)9) in whose results E.coli would correspond to 26.8% and 77.3% for both blood and urine cultures, respectively.
To the prevalence of tonsil or pharyngeal infectious focus in the case of adults with NHL, it is equivalent to 5 to 15% in which case the bacterial infection is 10 to 20% in which the main bacteria are streptococci pyogenes or streptococcus beta-hemolytic, this disease is equivalent to 16.8% morbidity in Peru10,11.
In our patient, the diagnosis of sepsis was made using the SIRS criteria, adding a confirmed infectious focus; our patient complied with increased heart rate, increased respiratory rate, and elevated temperature, but did not present a variation in leukocytes; in other words, the patient fulfilled 3 of the 4 criteria and the infectious focus of E. coli of confirmed tonsil onset.12-14
Investigations are reported in patients with oncological neoplasms such as those described by Ruiz and Guzmán AC and Arroyave-Peña T, in which approximately 60% of the most frequent infections are gram-negative, specifically E. coli, especially in tract infections urinary7,9,12. The scenario varies if it is a lesion on the upper palate, as in the case of the patient, showing a necrotized plaque with a positive pharyngeal culture E. coli which has not been reported in the national literature on it, and against the etiology of the frequency of infections and with negative urine culture; both in the investigations and in the patient, the treatment to choose was according to the antibiogram and sensitivity of the germ.12,13
Sepsis is associated with a decrease in the perfusion of oxygen to the tissues, due to the vasodilation that it generates. However the presence of E. coli suggests that its endotoxin also contributed to the peripheral necrosis of the patient described; In our case, the patient had NK-T-cell NHL, which in the face of immunosuppression due to the neoplasia predisposes her to obtain an infection, and this increases the risk of being susceptible to the action of endotoxin in the body, probably causing the necrotic plaque.14,15
In the case report of Castro BJI, a similar lesion is evidenced, as it describes a necrotic induration of the right nostril associated with the fetid whitish seropurulent discharge of 3 months of evolution. However, microbiological examinations found that it was of fungal origin, in which it also focuses on the rarity of infection in the mentioned area.15
There were limitations such as administrative problems that predispose patients to attend the office when the lesion is of significant size and presents deteriorated clinical symptoms, making the diagnosis to treat the underlying pathology and associated infections late.
CONCLUSIONS
Infections in immunocompromised people, such as T-NK lymphoma, are usually severe, causing a picture of sepsis. There is little international and national bibliography that reports a pharynx-tonsillar infection by E.coli. Few reports are mentioned on this type of nasal extranodal lymphoma. For this reason, our work contributes to the scientific and academic literature.
REFERENCES
1. Mayo Clinic. Linfoma no hodgkiniano. Mayo Clinic (Internet). Citado el Jueves 11 de Julio del 2019, de: https://www.mayoclinic.org/es-es/diseases-conditions/non-hodgkins-lymphoma/symptoms-causes/syc-20375680 [ Links ]
2. Saavedra RJD, Linfoma Nasal de Céluas T/Natural Killer Extranodal Refractario Mal Diagnosticado Tratado de Manera Exitosa: Informe de Caso. Case Rep Oncol. 2017;10:1092-1097. [ Links ]
3. Solidoro Santiesteban A, Misad Núñez O. Linfomas en el Perú y el Mundo: Un estudio multinacional de las neoplasias del sistema linfático. Acta Cancerológica. 19(2):15-26, 1988. 2013. [ Links ]
4. Instituto Nacional de Estadística e Informática. Mujeres con diagnóstico de cáncer, según órgano comprometido (Internet).Perú: INEN; 2017(revisado: 02 de Marzo del 2020). Disponible en: https://www.inei.gob.pe/media/MenuRecursivo/indices_tematicos/c_9_3.xlsx [ Links ]
5. Instituto Nacional de Estadística e Informática. Hombres con diagnóstico de cáncer, según órgano comprometido (Internet).Perú: INEN; 2017(revisado: 02 de Marzo del 2020). Disponible en: https://www.inei.gob.pe/media/MenuRecursivo/indices_tematicos/c_10_3.xlsx [ Links ]
6. Bletrán Gárate Brady, Morales Luna Domingo, Quiñones Ávila Pilar, Hurtado de Mendoza Fernando, Riva Gonzales Luis, Yabar Berocal Alejandro et al . Linfomas cutáneos primarios: estudio retrospectivo clinicopatológico durante el periodo 1997 - 2004 en el Hospital Edgardo Rebagliati Martins, Essalud, Lima, Perú. Acta méd. peruana (Internet). 2008 Abr (citado 2020 Abr 12); 25(2): 81-84. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1728-59172008000200007&lng=es [ Links ]
7. Ruiz y Guzmán AC, Peña-Pérez CA, Vargas Ruiz AG, Hernández-Castañeda B, Domínguez-Sandoval ZNC, Villagómez-García I, et al. Infecciones nosocomiales en pacientes con neoplasias hematológicas. Rev Sanid Milit Mex 2017;71(1):22-30. [ Links ]
8. Cantalapiedra Barbosa M. características clínico-biológicas y factores asociados a bacteriemias en pacientes oncológicos(tesis doctoral) España: Universidad de Valladolid: 2019. [ Links ]
9. Arroyave-Peña T, Puerta-Rojas J, Beltrán-Benavidez R, Salgado-Gómez T, Ramírez-Cadavid D, Arroyave Ávila D, et al. Características de los pacientes adultos con neutropenia febril en un hospital universitario (Medellín, 2012-2016). MEDICINA U.P.B. 38(2):108-113 [ Links ]
10. Cots Yago J, Alós Cortés J, Caamaño M, Boleda Relats X, Cañada Merino J, Gómez Gabaldón N,et al. Guía clínica para el manejo de la faringoamigdalitis aguda del adulto. Farmacéuticos Comunitarios(Internet). 2015;7(1):20-31.Disponible en: doi:10.5672/FC.2173-9218.(2015/Vol1).001.04 [ Links ]
11. María Cristina G, Albino José A. actualización del tratamiento de la faringoamigdalitis recurrente del adulto. Revisión. Rev. ORL(Internet). 2016, 7(1): 23-34. Disponible en: http://dx.doi.org/10.14201/orl201671.13531 [ Links ]
12. Vaduva, C., Gómez, J. I. T., Zaid, D. M., & Rivera-Rodríguez, T. (2019). Patología infecciosa aguda de foco otorrinolaringológico. Medicine - Programa de Formación Médica Continuada Acreditado, 12(91), 5339-5351. doi:10.1016/j.med.2019.11.021 [ Links ]
13. Cubas Santiago, Varela Martín, Noria Alejandro, Ibarra Sebastián, Martínez José Pablo, González Fabián et al . SIRS como predictor de severidad en la pancreatitis aguda. Rev. Méd. Urug. (Internet). 2017 Sep (citado 2020 Abr 04) ; 33(3): 26-37. Disponible en: http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-03902017000300026&lng=es. http://dx.doi.org/10.29193/rmu.33.3.2 [ Links ]
14. Minasyan H. Sepsis: mecanismos de lesión bacteriana para el paciente. Scand J Trauma Resusc Emerg Med . 2019; 27 (1): 19. Publicado el 14 de febrero de 2019 doi: 10.1186 / s13049-019-0596-4 [ Links ]
15. Castro B José I., Jiménez H Mario J., Herrera L. Sandra. Linfoma nasal de células T/NK (granuloma letal de la línea media), una neoplasia agresiva. Reporte de un caso. Rev. Otorrinolaringol. Cir. Cabeza Cuello (Internet). 2018 Jun (citado 2020 Abr 04) ; 78( 2 ): 197-201. Disponible en: https://pubs.rsna.org/doi/10.1148/radiol.2462070712 [ Links ]
Received: June 22, 2020; Accepted: July 20, 2020











 texto en
texto en 


