Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de la Facultad de Medicina Humana
Print version ISSN 1814-5469On-line version ISSN 2308-0531
Rev. Fac. Med. Hum. vol.20 no.4 Lima Oct-Dec 2020
http://dx.doi.org/10.25176/rfmh.v20i4.3190
Clinical case
Severe pneumonia of torpid evolution in young patient with negative molecular test for new coronavirus
1Hospital Nacional Edgardo Rebagliati Martins-EsSalud, Lima-Perú.
2Universidad Nacional de Piura. Piura-Perú.
3Universidad Nacional Mayor de San Marcos. Lima-Perú.
The coronavirus disease originating in 2019 (COVID-19) has spread rapidly throughout the world, wreaking havoc on the health system and society. The case of a 26-year-old man with a history of asthma and obesity is reported. He returned from the United States and came to the emergency room with respiratory symptoms, hypoxemia, and interstitial infiltrate on the chest X-ray. The admission to the isolation room was decided, and the molecular test RT-PCR of the nasopharyngeal swab was negative, for which he was transferred to a standard emergency room. Initial management was conservative; however, the patient evolved unfavorably requiring ventilatory support, and died on the fifth day of hospitalization. A second positive result for SARS-CoV-2 was received the day after the patient died; he was one of the first young victims in Peru.
Key words: COVID-19; SARS-CoV-2; Pneumonia viral; Coronavirus infections; Emergency medical services (Source: MeSH NLM).
INTRODUCTION
In December 2019, cases of severe viral pneumonia of unknown cause were reported, related to a market in the city of Wuhan (Hubei-China). This recent disease is caused by a new virus, called SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2) and was designated COVID-19 (Coronavirus Disease 2019). It has spread rapidly throughout the world and has affected many health systems1-5.
The first case reported in America was in the United States of America (USA) on January 23, 20206, while in South America, it was presented for the first time in Argentina a month later, and on March 11, the COVID-19 pandemic7. In Peru, the first infected patient was confirmed on March 6, 2020, with a rapid increase in cases, with 4,342 confirmed cases and 121 deaths reported to date, with a fatality rate of 2.79%, claiming the lives of 2 young patients8.
As of April 8, 2020, 1 506 936 cases were confirmed in the world due to this pandemic, claiming 90 057 lives9, this disease is characterized by producing respiratory conditions that quickly require ventilatory assistance and cause death. It affects a more significant proportion of patients over 40 years of age, mostly men; more than 60% of the deceased had at least one medical condition, and older adults had the highest probability of having severe illness. On the other hand, most of the young patients had mild presentations of the disease.
The diagnosis is based on detecting viral RNA using a polymerase chain reaction test (RT-PCR) of the sample of secretions10,11. This test is subject to error. This case report aims to report on a case of a young patient in Peru with COVID-19 and discuss the role of supplementary data such as imaging characteristics. It provides a more reliable value at the time of diagnosis, making a timely therapeutic approach, highlighting the rapid progression of pulmonary involvement, with a disease’s torpid course.
CASE REPORT
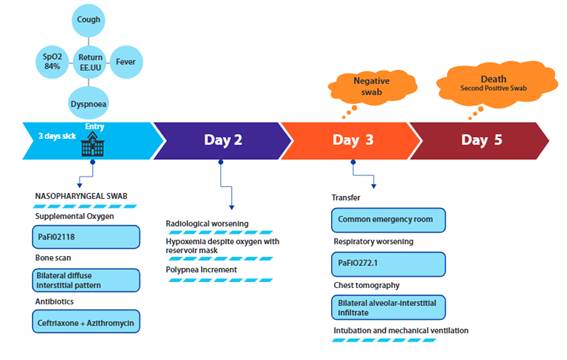
The patient was a 26-year-old male, who was admitted to the emergency service of the Hospital National Edgardo Rebagliati-EsSalud, Lima, Peru, on March 25, 2020, through the differentiated respiratory triage area. He was hospitalized in an observation room emergency services for suspected COVID-19 patients. The patient reported having had three days of cough with little whitish expectoration, a sensation of thermal rise, and the appearance of dyspnea on the day of admission. He also mentioned a history of bronchial asthma and obesity. Ten days before, he was on a trip to the United States.
His vital signs on admission were: blood pressure 100/70 mmHg, heart rate 80 beats/min, 24 breaths/min, pulse oximetry 84%, reaching 91% with a binasal cannula (5 liters/min). He presented 15 points on the Glasgow coma scale, moist mucous membranes, capillary filling less than 2 seconds on physical examination. His rhythmic heart sounds were of good intensity; polypneic with accessory musculature and crackles were heard in both lung fields.
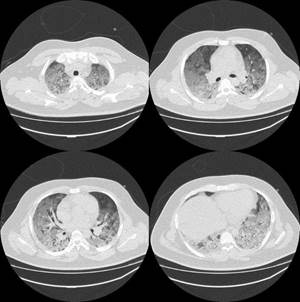
A pharyngeal swab sample, chest X-ray (Figure 1) was taken and antibiotic treatment was started with intravenous ceftriaxone 2g (IV) every 24 hours, azithromycin 500mg orally (PO) every 24 hours and hydrocortisone 100mg IV every 8h. Supplemental oxygen was administered by reservoir mask.
On the second day of hospitalization, he persisted with dyspnea and polypnea, the radiography control showed progression of the bilateral interstitial pattern, he maintained 89% pulse oximetry with a reservoir mask at 15 liters / min and on the third day the negative result of (RT - PCR for SARS-CoV-2), being removed from the room of suspected COVID-19 patients
He was transferred to the hospital’s trauma-shock unit and admitted to a general observation room, where the health team showed an oxygen saturation of 82% with a reservoir mask. A computed tomography (CT) of the chest without substance was performed contrast (Figure 2) and laboratory tests (Table 1), found leukocytosis 15 930 K / ul, PaFiO2 72.1, C-reactive protein 18.88 mg / dl, lactic dehydrogenase 789 U/ L.
Table 1. Laboratory tests during hospitalization
| Arterial gases | 28 - 3 | 29 - 3 | 30 - 3 | |
| PaO2*(mmHg) | 47.3 | 57.7 | ||
| PaCO2**(mmHg) | 33.3 | 33.2 | ||
| PaFiO2● | 118 | 72.1 | ||
| G(A-a)● ● | 197.7 | 469 | ||
| pH | 7.43 | 7.45 | ||
| Lactate (mmol/L) | 1.1 | 1.1 | ||
| Bicarbonate (mEq/L) | 21.9 | 23.2 | ||
| Hemogram | ||||
| Leukocytes (K/ul) | 15.93 | 19.44 | 10.7 | |
| Lymphocytes (K/ul) | 1.480 | 3.06 | 0.63 | |
| Biochemistry | ||||
| Creatinine (mg/dl) | 0.77 | 0.87 | 0.98 | |
| Urea (mg/dl) | 31.4 | 40.5 | 29.1 | |
| Glucose (mg/dl) | 96 | 133 | 129 | |
| Others | ||||
| Dimero D (ug/ml) | 1.39 | |||
| C-Reactive Protein (mg/dl) | 18.88 | 32.53 | 25.34 | |
| DHLa(U/L) | 789 | 811 | ||
| Cardiac Enzymes | ||||
| Troponin I (ng/ml) | 0.004 | |||
| CPKb- MB (ng/ml) | 0.76 | |||
| Coagulation profile | ||||
| TPc(sec) | 11.01 | 12.24 | 11.05 | |
| aPTd(sec) | 32.02 | 36.75 | 30.38 | |
| Fibrinogen (mg/dl) | 725.08 | 633.35 | 547.47 | |
| Hepatic Profile | ||||
| TGOe(U/L) | 49 | 68 | ||
| TGPf(U/L) | 81 | 121 | ||
| Total Bilirubin (mg/dl) | 0.76 | 0.38 |
* Arterial oxygen pressure, ** Arterial carbon dioxide pressure, ● PaO2 / Inspired oxygen fraction ratio, ●● Arterial alveolus gradient. to. Lactic dehydrogenase, b. Creatine phosphokinase, c. Prothrombin time, d. Activated thromboplastin time, e. Glutamic oxaloacetic transaminase, f. Glutamic pyruvic transaminase.
Due to the extensive alveolar and interstitial infiltrate evidenced in the tomography, a pharyngeal swab was repeated. Due to the poor ventilatory pattern, orotracheal intubation was performed, and mechanical ventilation was connected. Treatment was started with hydroxychloroquine 200 mg by nasogastric tube every 12 hours and imipenem 500 mg IV every 6 hours. Klebsiella ESBL received a positive urine culture result, which is why antibiotic coverage is maintained.
On the fifth day of hospitalization, the patient presented asystole, proceeding to perform advanced cardiopulmonary resuscitation maneuvers for 20 minutes without success, confirming his death. One day after death, the result of the second nasopharyngeal swab was obtained, being positive for SARS-CoV-2.
For this report, the principle of confidentiality was followed and authorization was obtained from the respective hospital service. Informed consent was not obtained because the patient died; however, the authorization was obtained from the Head of the Rebagliati Hospital Emergency Service.
DISCUSSION
This case corresponds to the youngest deceased patient reported in the country to date, who had risk factors for severe COVID-19 (bronchial asthma and obesity) and who was a potentially serious case according to the service's care flow chart12for which he was hospitalized in an observation room for suspected COVID-19 patients. The patient had a first negative nasopharyngeal swab result that led to suspicion of another etiology such as influenza virus or mycoplasma; however, in times of pandemic, the possibility of error in diagnostic tests should be considered8,9. Initially, the SARS-COV-2 infection was ruled out, and he was taken to a common observation room, together with patients with other pathologies, with a conservative initial therapeutic approach, where ventilatory support was delayed despite the failure characteristics Oxygen therapy and radiographs, knowing the course of pulmonary involvement in patients with COVID-19, the evolution was torpid (Figure 3).
The largest number of confirmed cases in Peru are in patients between 30 and 39 years of age. being the highest fatality in older adults, reporting only three young deaths, corresponding to the economically active population and an important group that does not comply with isolation measures8; similar to that reported in the province of Zhejiang (Wuhan - China) with a median age of 41 years and 56% of males in those infected by SARS-COV-213. On the other hand, in a cohort of 799 patients from Tongji Hospital, 113 deceased and 161 recovered; the median age of the deceased being 68 years, significantly higher than those recovered and no patient under 40 years of age died10.
Guan. Et al11, reports data from 1,099 laboratory-confirmed COVID-19 patients from 552 hospitals in 30 provinces, finding a median age of 47 years, 41.9% of women were affected, patients ≥65 years and between 15 and 49 years of age presented severe disease in 42.2% and 41.1% of the cases respectively, figures higher than the other age groups.
The patient studied had as a precedent having been in an area with a significant number of COVID-19 cases, where he probably acquired the infection. The estimated time of onset of symptoms from exposure was four to seven, being in the range of the incubation period; This time is difficult to specify as reported by Xu et al13, who were able to determine the exact date of close contact with an infected person in only 56 patients, calculating an average incubation period of four days, which coincides with that found by Guan et al. at11and close to three days reported in our patient. A retrospective study in 71 deceased reported that the average time from the onset of symptoms to hospital admission was ten days and the average time from admission to death was five days10, data that are similar to the case reported.
The most common symptoms were fever on admission and cough, similar to that found by Xu et al13. On the other hand, patients who died developed tachycardia and tachypnea more frequently compared to recovered patients, 72 (64%) of deceased patients and only 19 (12%) who recovered had a percutaneous oxygen saturation ≤93%10, findings similar to those recorded on admission in this patient.
Lymphopenia is a frequent finding in patients with COVID-19, being persistent and more severe in those who die, however, it did not occur in this case. The presence of leukocytosis, as in this patient, could be due to a bacterial coinfection as evidenced by the isolation of Klebsiella in the urine culture examination of the patient10,11,13.
The patient's admission chest X-ray showed an interstitial pattern, considering that the initial images with chest X-ray (RX) and computed tomography (CT) may be normal in non-severe disease, up to 18% of patients have an X-ray or normal initial CT, but only 3% in severe disease, in the case presented oxygen compromise was evident with three days of onset of symptoms. A study in 121 symptomatic patients found normal CT scans in 56% of patients scanned within 48 hours of symptom onset, whereas normal CT scans were only seen in 9% and 4% of patients scanned within 48 hours. the three to five days and six to twelve days, respectively. Radiographic abnormalities are more likely to be found on CT after six days of symptoms14. Upon admission, ground glass opacity was the most common radiological finding on chest CT11. Typical chest CT findings were bilateral areas or multiple lobar or subsegmental consolidation or bilateral ground glass opacity13.
The result of RT-PCR taken from the patient upon admission was negative, for which it was decided to transfer the patient to the general adult emergency area where at the moment the health personnel who attend do not have adequate biosecurity measures for the care of suspicious or infected patients. RT-PCR is specified to be the Gold standard, and the sensitivity ranges from 60 to 70%, and as such multiple negative tests may be required to exclude COVID-19. The interval between a first negative test to a second positive has been reported to be four to eight days14.
In a group of 258 patients who underwent sequential RT-PCR tests, 205 (80%), 45 (17%), 8 (3%) positivity were detected with two, three and four tests performed, respectively15. The positivity rate is variable according to the samples obtained, nasal swabs 63%, pharyngeal swabs 32%, bronchoalveolar lavage 93%, tracheal secretions 32%, however; the latter have a higher risk of transmission for the personnel obtaining the samples16.
Tomography provides benefits for the diagnosis of COVID-19, showing typical features in almost all patients, including ground glass opacities, consolidation in multifocal patches, and interstitial changes with a peripheral distribution. In a study of 1014 patients, 59% had positive RT-PCR results and 88% had positive CT scans, the sensitivity of chest CT was 97%. In patients with negative RT-PCR results, 75% had positive findings on chest CT, the interval between initial negative to positive results was 6.9 ± 2.3 days, similar to that reported by Rodrigues J. et al. . The negative predictive value of chest CT was 84% and 80% for patients <60 and ≥60 years, respectively.
As reviewed, it was an inappropriate action to take a patient with a negative result of the RT-PCR test for SARS-COV-2 to a general ward, having high suspicion based on clinical, epidemiological and radiological characteristics, exposing the personnel of health and patients who were admitted to these emergency rooms; shortly after, a technical document was published that dictates recommendations on the care of suspicious patients, with negative tests for COVID-19, indicating that it should be transferred to the corresponding area according to severity, maintaining the standards of prevention and control of infections17, however , there is a lack of isolation areas even in more complex hospitals such as ours, where this patient should have been destined until the absence of SARS - COV - 2 infection was corroborated with sequential examinations. Among the limitations of the case we have not Studies were carried out for other viruses or other atypical agents (mycoplasma or chlamydia) and that there were delays in some processes due to the increasing demand generated by the advance of the pandemic.
CONCLUSION
In the current health emergency, the low sensitivity of nasopharyngeal swab RT-PCR for SARS-COV-2 means that several COVID-19 patients are not identified and do not receive timely treatment, increasing mortality due to the rapid progression of the disease also increases the risk of infecting health workers. In this context, tomography provides diagnostic benefits with specific findings such as multilobar ground glass lesions. Also, we must bear in mind that young patients are not free from COVID-19, and must assess other aspects such as risk factors and clinical characteristics.
REFERENCES
1. Wu F, Zhao S, Yu B, Chen Y-M, Wang W, Song Z-G, et al. A new coronavirus associated with human respiratory disease in China. Nature (Internet). marzo de 2020 (citado 5 de abril de 2020);579(7798):265-9. DOI: https://doi.org/10.1038/s41586-020-2008-3 [ Links ]
2. Lee A. Wuhan novel coronavirus (COVID-19): why global control is challenging? Public Health (Internet). febrero de 2020 (citado 5 de abril de 2020);179:A1-2. DOI: https://doi.org/10.1016/j.puhe.2020.02.001 [ Links ]
3. Cheng ZJ, Shan J. 2019 Novel coronavirus: where we are and what we know. Infection (Internet). abril de 2020 (citado 7 de abril de 2020);48(2):155-63. DOI: https://doi.org/10.1007/s15010-020-01401-y [ Links ]
4. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet Lond Engl (Internet). 2020 (citado 9 de abril de 2020);395(10223):470-3. DOI: 10.1016/S0140-6736(20)30185-9 [ Links ]
5. Bogoch II, Watts A, Thomas-Bachli A, Huber C, Kraemer MUG, Khan K. Potential for global spread of a novel coronavirus from China. J Travel Med (Internet). 27 de enero de 2020 (citado 9 de abril de 2020);27(2). DOI: 10.1093/jtm/taaa011 [ Links ]
6. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med (Internet). 5 de marzo de 2020 (citado 5 de abril de 2020);382(10):929-36. DOI: 10.1056/NEJMoa2001191 [ Links ]
7. Alocución de apertura del Director General de la OMS en la rueda de prensa sobre la COVID-19 celebrada el 11 de marzo de 2020 (Internet). (citado 5 de abril de 2020). Disponible en: https://www.who.int/es/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [ Links ]
8. Sala situacional COVID19 Perú (Internet). Sala Situacional Covid19. (citado 5 de abril de 2020). Disponible en: https://covid19.minsa.gob.pe/sala_situacional.asp [ Links ]
9. Cumulative COVID-19 cases reported by countries and territories in the Americas (Internet). (citado 5 de abril de 2020). Disponible en: https://who.maps.arcgis.com/apps/webappviewer/index.html?id=2203b04c3a5f486685a15482a0d97a87&extent=-17277700.8881%2C-1043174.5225%2C-1770156.5897%2C6979655.9663%2C102100 [ Links ]
10. Chen T, Wu D, Chen H, Yan W, Yang D, Chen G, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ (Internet). 26 de marzo de 2020 (citado 5 de abril de 2020);m1091. DOI: https://doi.org/10.1136/bmj.m1091 [ Links ]
11. Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med (Internet). 28 de febrero de 2020 (citado 5 de abril de 2020);NEJMoa2002032. DOI: 10.1056/NEJMoa2002032 [ Links ]
12. Acosta G, Escobar G, Bernaola G, Alfaro J, Taype W, Marcos C, et al. Caracterización de los pacientes con COVID-19 grave atendidos en un Hospital de referencia nacional del Perú. Rev Peru Med Exp Salud Publica. 2020;37(2):1-5. DOI: https://doi.org/10.17843/rpmesp.2020.370.5437 [ Links ]
13. Xu X-W, Wu X-X, Jiang X-G, Xu K-J, Ying L-J, Ma C-L, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ (Internet). 19 de febrero de 2020 (citado 5 de abril de 2020);m606. DOI: https://doi.org/10.1136/bmj.m606 [ Links ]
14. Rodrigues JCL, Hare SS, Edey A, Devaraj A, Jacob J, Johnstone A, et al. An update on COVID-19 for the radiologist - A British society of Thoracic Imaging statement. Clin Radiol (Internet). mayo de 2020 (citado 5 de abril de 2020);75(5):323-5. DOI: https://doi.org/10.1016/j.crad.2020.03.003 [ Links ]
15. Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology (Internet). 26 de febrero de 2020 (citado 5 de abril de 2020);200642. DOI: https://doi.org/10.1148/radiol.2020200642 [ Links ]
16. Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA (Internet). 11 de marzo de 2020 (citado 9 de abril de 2020). DOI: 10.1001/jama.2020.3786 [ Links ]
17. Resolución Ministerial N° 193-2020-MINSA (Internet). (citado 17 de abril de 2020). Disponible en: https://www.gob.pe/institucion/minsa/normas-legales/473575-193-2020-minsa [ Links ]
Received: April 28, 2020; Accepted: May 30, 2020











 text in
text in