Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista de la Facultad de Medicina Humana
versión impresa ISSN 1814-5469versión On-line ISSN 2308-0531
Rev. Fac. Med. Hum. vol.20 no.4 Lima oct./dic 2020
http://dx.doi.org/10.25176/rfmh.v20i4.3158
Clinical case
Influenza and Covid-19 co-infection: Report of five cases in a Peruvian Hospital
1Hospital Nacional Dos De Mayo. Lima, Perú.
2Facultad de Medicina Humana, Universidad Nacional Mayor de San Marcos. Lima, Perú.
3Instituto de Investigación de Ciencias Biomédicas, Universidad Ricardo Palma. Lima, Perú.
4Facultad de Medicina Humana, Universidad Ricardo Palma. Lima, Perú.
COVID-19 disease is an easily transmitted infection like other respiratory viruses, with cases of Influenza coinfection reported at seasonal times. There are 5 cases of coinfection of COVID-19 and the influenza virus. Influenza A virus being the most frequent. Symptoms of coinfection between these two viruses may suggest odynophagia and nasal congestion in the patients evaluated, no mortality was observed.
Key words: COVID-19; SARS-CoV-2; Influenza A virus; Coinfection (Source: MeSH NLM).
INTRODUCTION
SARS-CoV-2 is a new strain of Coronavirus that causes COVID-19 disease, characterized by acute respiratory distress. This disease produces significant morbidity and mortality, causing epidemic outbreaks in several countries, so the World Health Organization declared it a pandemic on March 11, 2020. Peru has more than 200,000 confirmed cases and more than 6,000 deaths from this disease being the second country in Latin America with the highest cases of deaths, behind Brazil1.
With regard to influenza, during the epidemic of 2009, it was reported more than 10,000 cases and over 300 deaths2. Recently, in the last two years, more than 650,000 deaths have been reported worldwide. In 2018, Peru had 760 positive cases for influenza and it was recorded that 35% of deaths from influenza syndrome that same year were positive for this virus.3
It is reported that 94.2% of COVID-19 patients may be coinfected with one or more other pathogens, and the main focus is related to bacteria4. Coexistence with other respiratory viruses has been reported. The most frequently found was Influenza, of a similar clinical presentation, transmission mechanism, and of seasonal coincidence.5)-(7
The association of COVID-19 with other respiratory viruses at this time of pandemic is not ruled out, however, early suspicion of this coinfectionis difficult due to the variable and atypical symptoms, which could worsen the prognosis of the patients.
CASE REPORT
We present our experience in 5 cases of coinfection of COVID-19 and the influenza virus, whose general characteristics are shown inTable 1
Table 1. Clinical findings in 5 patients with Influenza and COVID-19 coinfectiontreated at Hospital Dos de Mayo. Lima, Peru, 2020
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | |
| Age | 67 | 20 | 56 | 52 | 52 |
| Gender | Female | Male | Male | Female | Male |
| Comorbidities | |||||
| Cancer | NO | NO | NO | NO | NO |
| Obesity | YES | YES | NO | YES | YES |
| Hypertension | YES | NO | NO | NO | YES |
| Diabetes | YES | NO | NO | NO | YES |
| Heart failure | NO | NO | NO | NO | NO |
| COVID-19 RT-PCR | Positive | Positive | Positive | Positive | Positive |
| Influenza virus | Influenza A | Influenza B | Influenza A | Influenza A | Influenza A |
| Signs and symptoms | |||||
| Fever | YES | YES | YES | YES | YES |
| Cough | YES | YES | YES | YES | YES |
| Dyspnea | YES | YES | YES | YES | YES |
| Myalgia | YES | YES | YES | YES | YES |
| Fatigue | YES | YES | YES | YES | YES |
| Headache | YES | YES | YES | YES | NO |
| Diarrhea | NO | YES | NO | NO | NO |
| Nasal congestion | YES | NO | YES | YES | YES |
| Coughing | NO | YES | NO | NO | NO |
| Odynophagia | NO | NO | NO | YES | YES |
| Laboratory results | |||||
| Leukocytes mm3 | 4470 | 18010 | 19070 | 8850 | 13050 |
| Lymphocytes cel/mm3 | 678 | 1009 | 837 | 1628 | 1110 |
| Ferritin ng/ml | 147 | 725 | 879 | NT | NT |
| D-Dimer, mg / L | 0.51 | 2.74 | 0.89 | NT | 0.76 |
| Po2 mmHg | 67.6 | 73.1 | 47.1 | 52 | 67.3 |
| Pao2/fio2 mmHg | 169 | 348 | 52 | 96 | 321 |
| Procalcitonin | 1.01 | 0.74 | 0.19 | 0.16 | 0.91 |
| Radiological patterns | |||||
| Interstitial | YES | YES | YES | YES | YES |
| Alveolar | NO | YES | NO | NO | YES |
| Evolution | HIGH | HIGH | UCI | HIGH | HIGH |
NT= No
We present 3 male patients (60%) and 2 female patients (40%), with an average age of 49.4 years of age (20 - 67 years old). The most frequent comorbidities were obesity in 80% of the patients, followed by hypertension and diabetes in 40%.
None of the patients had SARS-VOC-2 contact, the average time of illness was 8.8 days from the onset of symptoms until hospitalization (5 - 14 days). The symptoms were fever, cough, dyspnea, myalgia, and fatigue in 100% of patients, headache and nasal congestion in 80%, odynophagia in 40% and in 20%, diarrhea, and expectoration.
The confirmatory diagnosis of SARS-COV-2 infection was made by the detection of serum IgM / IgG antibodies and RT-PCR by nasopharyngeal swab. For confirmation ofInfluenza, the diagnosis was by IgM using the indirectimmunofluorescence(IFI) technique. IFI ruled out the presence ofChamydophila Pneumoniae, Mycoplasma Pneumoniae, Legionella Pneumophila, Parainfluenza 1,2, and 3, Respiratory Syncytial Virus and Adenovirus.
Laboratory tests showed leukocytosis in 60% of patients, elevated CRP in 100% of patients and lymphopenia in 80% of patients, serum procalcitonin was elevated (>0.25 ng/ml) in 60% of patients. D-dimer test was performed in 4 patients and it was elevated in all of them. Ferritin test was performed in 3 patients, of which it was elevated in 2 of them. All were in Type I respiratory failure with PaO2/FiO2 average 197 mm Hg (52 - 348 mm hg).
The radiological findings show predominantly bilateral peripheral interstitial pattern and only 1 case presented an interstitial alveolar pattern. SeeFigure 1.
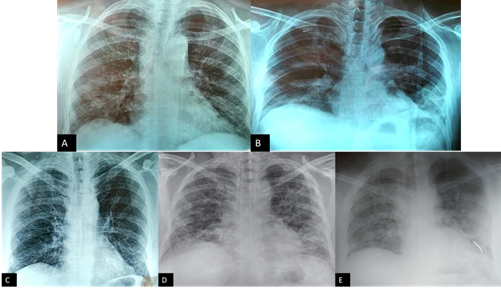
Figure 1. Images of the chest radiograph of patients. A: Patient 1, bilateral interstitial pattern with peripheral predominance is evident. B: Patient 2, a bilateral interstitial pattern associated with left basal alveolar pattern is evident. C: Patient 3, bilateral interstitial pattern with peripheral predominance is evident. D:Paciente 4, se evidencia patrón intersticial bilateral predominio periférico.Patient 4, a peripherally predominant bilateral interstitial pattern is evident. E: Patient 5, a peripherally predominant bilateral interstitial pattern is evident, associated with a left basal alveolar pattern.
No patient received antiviral therapy, patients required supplemental oxygen with a fraction of inspired oxygen O2 on average of 50%. All the patients received the SARS-COV-2 treatment from our institution, which is Hydroxychloroquine, Azithromycin, Methylprednisolone, and Enoxaparin, according to the recommendations of the Ministry of Health (MINSA)8. 80% of the patients had a favorable evolution and an early discharge from the hospital, and only one patient had an unfavorable evolution due to probable overgrowth infection and/or progressive COVID with severe respiratory failure with PaO2 / FiO2 less than 100 mmHg, therefore who is transferred to the intensive care unit (ICU).
DISCUSSION
COVID-19 disease can occur simultaneously with other infections such as seasonal influenza and, according to Azekawa et al., it can significantly suppress the host's immune system and be detrimental to the prognosis of the disease, making it difficult to distinguish symptoms of the two conditions from each other and especially during the influenza season.9
In our service, it was found that of 38 patients infected with COVID-19 who were asked for IFI, 13% had an infection due to over aggregated influenza, this being a rate incidence higher than that reported by Qiang6. This result may be because Influenza is a seasonal virus and it is common during the fall season. 80% of patients had Influenza A and only 1 patient had Influenza B, contrary to the data published by Zhu4where the Influenza B virus was the most frequently found in patients with COVID-19 and similar to the data reported by Ding6and Kim(9)concluding that the Influenza A virus is more frequently associated with COVID-19.
In both Influenza and COVID-19, comorbidities such as obesity, hypertension, and diabetes have been found to be associated with an increased risk of severity11), (12. These comorbidities were the most frequently found in this report.
These comorbidities were the most frequently found in this report.13, making it difficult to distinguish them based on symptoms. Other symptoms are nasal congestion and odynophagia which are not common of COVID-19 and their presence makes us think of COVID-19 coinfectionwith Influenza, which is similar to the findings found by Ding.6
The results of the laboratory admission showed leukocytosis in 3 patients and in elevated procalcitonin in 2 patients, which leads to suspicion of an aggregate bacterial infection, which predisposes to a worse prognosis in COVID-19. Other laboratory abnormalities associated with a worse prognosis are elevated CRP, present in 100% of our patients, and lymphopenia in 80%. The severity is also related to increased D-dimer and ferritin.15
The chest x-ray showed bilateral peripheral interstitial pattern in 80% of patients and 40% had an interstitial alveolus pattern. This imaging finding can be attributed to the progression of COVID-19 disease16.
No patient received antiviral treatment for Influenza due to the average illness time, which is 8.8 days. Studies have shown clinical benefit when antivirals are started within 2 days of symptom onset12. There is still no evidence of an effective treatment against COVID-19, however, all patients received the MINSA-approved treatment for COVID-198. Leukocytosis patients received antibiotic treatment associated with the outline for suspected associated bacterial infection.
80% of the patients were discharged due to clinical improvement despite having factors associated with poor prognosis such as comorbidities and laboratory abnormalities. These findings were similar to those reported by Ding where only 15.7% of the patients with COVID-19 and Influenza developed a severe disease6, likewise, Ozaras described that no patient with a coinfection of COVID-19 and Influenza needed ventilatory support and all improved without any complication17suggesting that patients with a coinfection of COVID-19 and the Influenza virus did not significantly worsen the condition, contrary to reported by Zhu, who indicate that co-infections of Influenza A and Influenza B may increase the risks of patients with COVID-194, which is why vaccination is recommended due to the lack of antiviral treatment to be able to adequately combat the Influenza infection3
Among the limitations, we can mention that the reported patients did not have a chest tomography which might be necessary to better characterize the lung lesions, and some patients did not have a ferritin and D-dimer laboratory test due to lack of reagents in our hospital.
CONCLUSIONS
Patients with COVID-19 infection show coinfection with the Influenza virus, and more frequently with the Influenza A virus, so we suggest testing all COVID-19 patients for other viruses and/or bacteria. Nasal congestion and odynophagia are symptoms that may suggest coinfectionwith the Influenza virus. No mortality was observed in the patients described.
More exhaustive studies are needed to corroborate the findings found in this report and thus be able to present more complete and solid conclusions.
REFERENCES
1. COVID-19 Map (Internet). Johns Hopkins Coronavirus Resource Center. (citado 8 de mayo de 2020). Disponible en: https://coronavirus.jhu.edu/map.html [ Links ]
2. Suárez-Ognio L, Arrasco J, Gómez J, Munayco C, Vílchez A, Cabezas C, et al. Mortalidad relacionada a influenza A H N en el Perú durante la pandemia en 2009-2010. Rev Peru Epidemiol. 2011;15(1):1-7. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=3749926 [ Links ]
3. Laguna-Torres VA, Gómez J, Hernández H, Francia-Romero J, Bisso-Andrade A, Guerreros A, et al. Vigilancia, prevención y control del virus de la influenza en Perú. Rev Peru Med Exp Salud Pública. 2019;36(3):511-4. DOI: 10.17843/rpmesp.2019.363.4481 [ Links ]
4. Zhu X, Ge Y, Wu T, Zhao K, Chen Y, Wu B, et al. Co-infection with respiratory pathogens among COVID-2019 cases. Virus Res. agosto de 2020;285198005. DOI: 10.1016 / j.virusres.2020.198005 [ Links ]
5. Khodamoradi Z, Moghadami M, Lotfi M. Co-infection of Coronavirus Disease 2019 and Influenza: A Report from Iran. 19 de marzo de 2020 (citado 16 de abril de 2020); Disponible en: https://www.preprints.org/manuscript/202003.0291/v1 [ Links ]
6. Ding Q, Lu P, Fan Y, Xia Y, Liu M. The clinical characteristics of pneumonia patients coinfected with 2019 novel coronavirus and influenza virus in Wuhan, China. J Med Virol. 2020;1-7. DOI: 10.1002/jmv.25781 [ Links ]
7. Cuadrado-Payán E, Montagud-Marrahi E, Torres-Elorza M, Bodro M, Blasco M, Poch E, et al. SARS-CoV-2 and influenza virus co-infection. Lancet Lond Engl. 2020;395(10236):e84. DOI: 10.1016/ S0140-6736(20)31052-7 [ Links ]
8. Modifican el Documento Técnico: Prevención, Diagnóstico y Tratamiento de personas afectadas por COVID-19 en el Perú-RESOLUCION MINISTERIAL-N° 270-2020-MINSA (Internet). (citado 8 de mayo de 2020). Disponible en: http://busquedas.elperuano.pe/normaslegales/modifican-el-documento-tecnico-prevencion-diagnostico-y-tr-resolucion-ministerial-n-270-2020-minsa-1866159-4/ [ Links ]
9. Azekawa S, Namkoong H, Mitamura K, Kawaoka Y, Saito F. Co-infection with SARS-CoV-2 and influenza A virus. IDCases. 2020;20:e00775. DOI: 10.1016 / j.idcr.2020.e00775 [ Links ]
10. m D, Quinn J, Pinsky B, Shah NH, Brown I. Rates of Co-infection Between SARS-CoV-2 and Other Respiratory Pathogens. JAMA. 2020;323(20):2085-2086. DOI: 10.1001/jama.2020.6266 [ Links ]
11. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-5. DOI: 10.1016 / j.ijid.2020.03.017 [ Links ]
12. Chow EJ, Doyle JD, Uyeki TM. Influenza virus-related critical illness: prevention, diagnosis, treatment. Crit Care. 2019;23:214. DOI: https://doi.org/10.1186/s13054-019-2491-9 [ Links ]
13. Balla M, Merugu GP, Patel M, Koduri NM, Gayam V, Adapa S, et al. COVID-19, Modern Pandemic: A Systematic Review From Front-Line Health Care Providers' Perspective. J Clin Med Res. 2020;12(4):215-29. DOI: 10.14740/jocmr4142 [ Links ]
14. Wu D, Lu J, Ma X, Liu Q, Wang D, Gu Y, et al. Coinfection of Influenza Virus and Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-COV-2). Pediatr Infect Dis J. 2020;39(6):e79. DOI: 10.1097 / inf.0000000000002688 [ Links ]
15. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020;395(10229):1054-62. DOI: 10.1016/S0140-6736(20)30566-3 [ Links ]
16. Khaddour K, Sikora A, Tahir N, Nepomuceno D, Huang T. Case Report: The Importance of Novel Coronavirus Disease (COVID-19) and Coinfection with Other Respiratory Pathogens in the Current Pandemic. Am J Trop Med Hyg. 2020; 102(6):1208-1209. DOI: 10.4269/ajtmh.20-0266 [ Links ]
17. Ozaras R, Cirpin R, Duran A, Duman H, Arslan O, Bakcan Y, et al. Influenza and COVID-19 coinfection: Report of six cases and review of the literature. J Med Virol. 2020;1-9. DOI: https://doi.org/10.1002/jmv.26125 [ Links ]
Received: July 09, 2020; Accepted: July 23, 2020











 texto en
texto en 


