Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de la Facultad de Medicina Humana
Print version ISSN 1814-5469On-line version ISSN 2308-0531
Rev. Fac. Med. Hum. vol.21 no.1 Lima Jan-Mar 2021
http://dx.doi.org/10.25176/rfmh.v21i1.3194
Original article
Management of glycemic crises in adult patients with diabetes mellitus: Evidence-based clinical practice guideline clinical
1Servicio de Endocrinología, AUNA, Lima, Perú.
2Unidad de Guías de Práctica Clínica, AUNA, Lima, Perú.
3Servicio de Medicina Intensiva, AUNA, Lima, Perú.
4Servicio de Laboratorio, AUNA, Lima, Perú.
5Dirección Científica Académica, AUNA, Lima, Perú.
6Division of Endocrinology, Metabolism and Lipids, Department of Medicine, Emory University School of Medicine, Emory, Atlanta.
Introduction:
The manuscript summarizes the process of elaboration of the Clinical Practice Guide (CPG) for the management of glycemic crises in adult patients with diabetes mellitus of the AUNA Clinic Network. A multidisciplinary team of medical assistants and methodologists carried out the development of the CPG and then there was an external review by a specialist in the field.
Methods:
The Elaboration Group of the CPG (GEG) concluded on 10 PICO questions. A systematic search for CPG, systematic reviews and primary studies was carried out to answer these PICO questions. To make recommendations we used the "GRADE-Adolopment" methodology and the guidelines of the national regulations.
Results:
Ten recommendations were made (nine strong and one weak), 18 points of good clinical practice and two flowcharts for management (one for diagnosis and the other for the treatment of glycemic crises), 04 consensus tables on management and 01 table for surveillance and monitoring. The topics covered by the recommendations for the management of glycemic crises were hyperglycemic crises (glycosylated hemoglobin evaluation; b-hydroxybutyrate evaluation; insulin, potassium, 0.9% sodium chloride, phosphorus, sodium bicarbonate treatments) and hypoglycemic crises (carbohydrate administration, monitoring, educational program to avoid reentry).
Conclusion:
This article summarizes the methodology and evidence-based recommendations of the CPG for the management of glycemic crisis in patients with diabetes mellitus in AUNA.
Key words: Diabetes mellitus; Clinical Practice Guideline; disease management; hypoglycemia; hyperglycemia (Source: MeSH MLN).
INTRODUCTION
Diabetes mellitus is a disease with great impact worldwide1,2. For the year 2019, it has been estimated that 9.3% (463 million) of the world population have this disease3. Its acute complications (hypoglycemia and hyperglycemia) are a frequent cause of admission to hospital emergency services, especially in developing countries4-7.
In Peru, for 2015 the prevalence of diabetes mellitus was estimated between 6.1 - 7%. Within glycemic emergencies, ketoacidosis and hypoglycemia were the most common (21.6%) followed by hyperosmolar hyperglycemic state (18.2%)5. In that year it was approved by R.M. 719-2015 / MINSA the Technical Guide: "Clinical Practice Guide for the Diagnosis, Treatment, and Control of Type 2 Diabetes Mellitus in the First Level of Care" which included some recommendations for the management of glycemic crises; However, in the study carried out by Neira-Sánchez and Germán Málaga where their quality was evaluated using the AGREE II instrument, scores of less than 60% were found in all domains (The percentage in rigor in the elaboration was 17.71%)8,9
During 2019, taking into account the need to have Clinical Practice Guidelines based on the best available scientific evidence for the management of glycemic crises, AUNA proposed to its Academic Scientific Directorate that, through the Unit of Clinical Practice Guidelines, lead the development of the Clinical Practice Guide (CPG) for the management of glycemic crises in adult patients with diabetes mellitus.
METHODS
The process of preparing the clinical practice guide was developed taking into account the methodological proposal "GRADE-Adolopment"10,11and the methodological guidelines of the national regulations12. The GRADE-ADOLOPMENT methodology combines the advantages of formulating recommendations by adopting, adapting, and formulating de novo based on the GRADE strategy that includes, for each PICO question proposed by the panel, a summary of the evidence found (table “SoF”) and a paper discussion with a multidisciplinary team called “From evidence to recommendation” (EtD). The strategy has already been validated by the GRADE team and has been accepted in the construction of some clinical practice guidelines in different countries and organizations at the international and national levels.13-17.
Formation of the GEG and scope of the CPG
The preparation of the CPG was carried out by the Guide Development Group (GEG). The GEG was made up of two teams: the methodological team of the CPG Unit and the team of doctors from the healthcare area of the specialties of endocrinology, internal medicine, intensive medicine, and clinical laboratory.
The GEG decided to develop a CPG that provides guidelines to healthcare professionals (medical specialists, general practitioners, and other health professionals within the scope of their competencies) for the care of adult diabetic patients in emergency services, intermediate care units, or critical care from the AUNA Network clinics.
Formulation of PICO Questions, Systematic Search and AGREE II Evaluation
The PICO questions were selected based on the GEG prioritization criteria. The team of specialists decided during the panel sessions to consider the final structure of the question. A systematic search strategy for Clinical Practice Guidelines related to the study topic was carried out in Medline databases (via Pubmed), TRIP Database, Excerpta Medica Database (EMBASE, via Ovid), Latin American and Caribbean Literature in Health Sciences. Health (LILACS) and Epistemonikos with no start date until August 07, 2019. In addition, a search was carried out in CPG compiling and compiling bodies. The methodological quality was evaluated through two steps: following pre-selection criteria and then the AGREE II tool (https://www.agreetrust.org/) was used to assess the CPGs that passed the pre-selection criteria18-22(Vertable 1).
Review, synthesis, and discussion of the evidence
The clinical questions that could be answered by CPG recommendations that obtained a favorable rating in the AGREE II instrument (see table 1) were submitted to the GEG for discussion and it was decided whether or not they would be updated. For each of the other questions prioritized by the specialists, a systematic search for evidence was developed. In the case of questions answered by a CPG, in which some modification had been made in its structure, the adaptation of the search strategies was considered, while in the case of questions that had not been answered by any CPG, the procedure was to do a de novo search. In all cases, the review of the evidence found followed a process by independent peers that began with a reading phase of titles and abstracts, followed by a full-text reading phase of the potentially relevant citations identified in the previous phase. Any discrepancies were resolved by consensus during the GEG sessions.
Table 1. Evaluación de calidad metodológica de las GPC de cáncer de mama usando la herramienta AGREE II
| N° | Clinical Practice Guide | Domain 1: Scope and objective | Domain 2: Stakeholder involvement | Domain 3: Rigor in Crafting | Domain 4: Clarity of presentation | Domain 5: Applicability | Domain 6: Editorial independence | Overall evaluation | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Canadian Diabetes Association Diabetes Canada 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. | 76% | 85% | 71% | 96% | 61% | 86% | 78% | |
| 2 | American Diabetes Association Standards of Medical Care in Diabetes—2019 | 92% | 75% | 83% | 89% | 81% | 92% | 92% | |
| 3 | Cenetec Diagnóstico y tratamiento de la Cetoacidosis Diabética en niños y adultos | 94% | 72% | 65% | 56% | 60% | 63% | 75% | |
| 4 | Cenetec Diagnóstico y tratamiento del Estado Hiperglucémico Hiperosmolar en adultos con Diabetes Mellitus tipo 2 | 100% | 81% | 71% | 58% | 63% | 71% | 75% | |
| 5 | NICE Type 1 diabetes in adults: Diagnosis and management | 75% | 81% | 71% | 58% | 67% | 96% | 83% |
Source: Self made.
Formulation and Grading of Recommendations The formulation of the recommendations was carried out during the sessions of the GEG after the review and analysis of the evidence found (seetables 2and3). For the grading of the recommendation (strength and direction), the GRADE system (https://gradepro.org/) was used, which provides 4 criteria for grading the recommendations based on the quality of the evidence, balance between benefits and risks, values and preferences as well as costs and use of resources: strong in favor (The desirable consequences clearly outweigh the undesirable consequences. It is recommended to do so), Weak in favor (The desirable consequences probably outweigh the undesirable consequences. It is suggested to do so), Strong against (The undesirable consequences clearly outweigh the desirable consequences. It is not recommended to do so), Weak against (The undesirable consequences probably outweigh the desirable consequences. It is not suggested to do so) and Good Clinical Practice (Recommended practice, based on clinical experience and / or studies not systematically evaluated by the GEG).
Table 2. Recommendations made by the GEG in cases of hyperglycemic crisis with strength and direction of the recommendation
| N° | Recommendations | Strength and direction | Certainty in the evidence | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Evaluation of glycosylated Hb in diabetic patients diagnosed with hyperglycemia is not suggested for acute management. | Conditional against | Very low (⊕⊝⊝⊝) | ||||||||
| 2 | After the acute management of diabetic patients with hyperglycemia, perform a glycosylated Hb analysis for subsequent follow-up. | BPC | |||||||||
| 3 | The evaluation of B-hydroxybutyrate in the blood in diabetic patients is recommended for the diagnosis of CAD. | Strong for | Very low (⊕⊝⊝⊝) | ||||||||
| 4 | Consider periodic monitoring (every 4 hours until resolution) of B-hydroxybutyrate in the blood of diabetic patients found with CAD in the acute phase. | BPC | |||||||||
| 5 | In diabetic patients with b-hydroxybutyrate> = 1 should be considered to rule out CAD. | BPC | |||||||||
| 6 | It is recommended to start insulin infusion doses at 0.05 - 0.1 U / Kg / | Strong for | Very low (⊕⊝⊝⊝) | ||||||||
| 7 | Adjust the dose to 25% while achieving an average decrease of 50 mg / dL per hour. | BPC | |||||||||
| 8 | Maintain glucose values between 140 - 180 mg / dL in diabetic patients with hyperglycemia in critical or non-critical condition. | BPC | |||||||||
| 9 | It is recommended in adult diabetic patients with hyperglycemic crisis (CAD / EHH) with marked hypokalemia (serum potassium <3.3 mmol / L), add potassium at a dose of 10 - 20 mmol / L | Strong for | Very low (⊕⊝⊝⊝) | ||||||||
| 10 | Avoid the administration of Potassium, if the concentration of K is> 5.2 mEq / l. | BPC | |||||||||
| 11 | In adult diabetic patients with hyperglycemic crisis (CAD / HD) with normokalemia or mild hypokalemia (serum potassium between 3.3 mmol / L to 5 mmol / L, start intravenous potassium administration at concentrations of 10 - 20 mmol / L, at a maximum range 20 mmol / h) once urine output is restored. Taking precaution if the patient has kidney failure. | BPC | |||||||||
| 12 | It is recommended in adult diabetic patients with hyperglycemic crisis (CAD / EHH), initially administer 0.9% NaCl at 1000 ml / h until hypovolemic shock is corrected, then 0.9% NaCl at 500 ml / h for 4 hours and continue at 250 mL / h. | Strong for | Very low (⊕⊝⊝⊝) | ||||||||
| 13 | In adult diabetic patients with hyperglycemic crisis (CAD / EHH), carry out continuous monitoring of diuresis (if necessary, place a urinary catheter). | BPC | |||||||||
| 14 | Phosphorus replacement is not recommended in adult diabetic patients with hyperglycemic crisis (CAD / EHH) and non-severe hypophosphatemia. | Strong agains | Very low (⊕⊝⊝⊝) | ||||||||
| 15 | In cases where hypophosphatemia is severe (<1 mg / dL (0.32 mmol / l), consider its replacement. | BPC | |||||||||
| 16 | In adult diabetic patients with hyperglycemic crisis (CAD / EHH) and hypophosphatemia, monitor serum phosphorus levels. | BPC | |||||||||
| 17 | The administration of sodium bicarbonate is not recommended in adult diabetic patients with CAD with pH ≥ 6.9 | Strong against | Very low (⊕⊝⊝⊝) | ||||||||
| 18 | It is recommended in adult diabetic patients who present severe CAD with pH <6.9 or in shock, the administration of 50 mmol of sodium bicarbonate in 200 mL of normal saline for one hour and continue every 1 - 2 hours until the pH is ≥ 6.9. | Strong for | Very low (⊕⊝⊝⊝) | ||||||||
| 19 | In adult diabetic patients presenting with severe CAD with pH <6.9 or in shock who are replaced with sodium bicarbonate, monitor serum potassium. | BPC |
Source: Self made.
Table 3. Recommendations made by the GEG in cases of hypoglycemia with strength and direction of the recommendation.
| N° | Recommendations | Strength and Direction | Certainty in the evidence |
| 1 | Treat severe hypoglycemia in a conscious person in the emergency area by orally ingesting 20 g of carbohydrates, preferably as glucose tablets or equivalent (eg dilute a tablespoon of sugar in 1 glass with water or observe the equivalent in the tables of nutritional balance of the products to be consumed) | BPC | |
| 2 | Check blood glucose values every 15 minutes and ingest another 20 g of glucose if blood glucose remains <4.0 mmol / L (72 mg / dL). | BPC | |
| 3 | Treat severe hypoglycemia in an unconscious person by intravenous administration of 25 g (4 ampoules of 33% dextrose) of glucose administered during the first 3 minutes. | BPC | |
| 4 | In patients with severe hypoglycemia, consider a residence time of at least 24 hours. | BPC | |
| 5 | In patients with severe hypoglycemia associated with complications, consider that the hospital stay could be longer. | BPC | |
| 6 | In patients with severe hypoglycemia consider monitoring capillary blood glucose every 1-2 hours for the first 6 hours. | BPC | |
| 7 | IT IS RECOMMENDED to standardize an educational program aimed at the patient and / or family while maintaining general glycemic control aimed at avoiding readmission for hypoglycemia. | Source in favor | Very low (⊕⊝⊝⊝) |
| 8 | Include a psycho-behavioral therapeutic intervention directed towards patients if readmissions are recurrent (> 3 times a year). | BPC |
Source: Self made.
Conflicts of Interest of Participants in the GEG
To ensure the integrity and public trust in the activities of the GEG; each one declared their conflicts of interest according to the Form for Declaration of Conflicts of Interest of the Technical Document: Methodology for the Preparation of Clinical Practice Guidelines of the Ministry of Health.
External Review
The CPG was evaluated by an endocrinologist specialized in the subject with expertise in the development of clinical practice guidelines with GRADE methodology. You were asked to declare if you have any conflict of interest to express an opinion on any of the issues reviewed within the CPG. After the review, a tele-meeting was held to discuss the suggestions submitted by the external reviewer and conclude the final version of the clinical practice guideline.
Implementation, monitoring of compliance with Recommendations, and updating of the CPG
The CPG was socialized through internal meetings and space was created on the institutional website: https://clinicadelgado.pe/guias-de-practica-clinica/. Through it, you can access the 2 versions of the CPG (long version and summary version).
To follow up on the recommendations, it was decided to choose key recommendations on which the indicators were built (seetable 3).Said indicators would be evaluated at 06 months and one year after the approval of this CPG.
It was decided at the GEG meeting that the CPG update be carried out within a period of 3 years from the date of its publication, or when relevant information is identified that may modify the meaning of the clinical recommendations included. To identify relevant information, an update of the search strategies for the recommendations will be developed every six months.
RECOMMENDATIONS
Hyperglycemic Crises
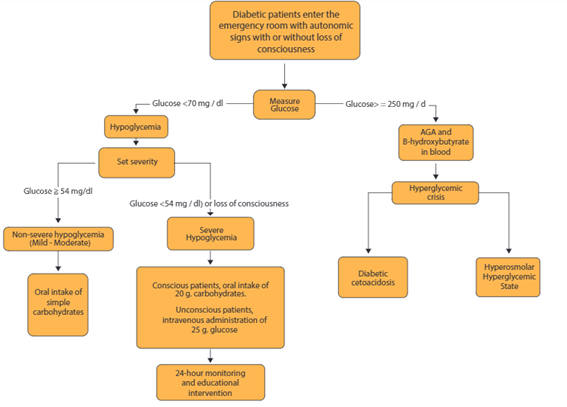
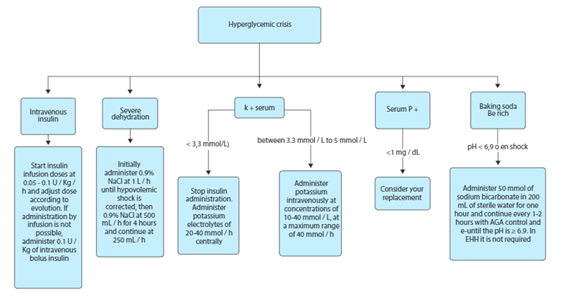
Seven questions were developed regarding hyperglycemic crises. Two tables were prepared, the first to summarize the diagnosis and severity of hyperglycemic crises and the second to establish criteria for electrolyte administration (seetable 4andtable 5). Further; Two figures were prepared, 1 figure that included the diagnosis of hyperglycemic crises and 1 figure that included the treatment of hyperglycemic crises (seefigure 1yfigure 2)
Question 1: In adult diabetic patients with glucose disorders, what is the usefulness of requesting glycated Hb for the management of acute glucose disorders?
Evidence Summary
HbA1c (glycated hemoglobin) is a test used for the diagnosis and monitoring of diabetes and prediabetes23,24. Generally reliable as an indicator of chronic blood glucose, it may be inaccurate in the presence of abnormal red blood cells, hemoglobinopathy, or another disorder that affects red blood cells25.
A systematic search was carried out which concluded in the review of 03 articles for full text (no systematic reviews were found). Two were excluded because they did not include a diabetic patient population or did not specify it as part of the study26,27. The study of Magee MF. et al. 2011 (28, is a cohort study in which 86 patients were analyzed, of which 81% of the participants completed 2 visits, 67% completed 3 visits where repeated A1C measurements were obtained, and 60% completed all 4 visits. Mean glycemia decreased from 356 ± 110 mg / dl at the beginning of the study to 183 ± 103 mg / dl at 4 weeks, representing an average reduction of 173.5 mg / dl (p <0.001 for the paired t-test). There were zero cases of hypoglycemia on day 1, and overall hypoglycemia rates were low (1.3%). At the start of the study, 50% of the A1C values were> 13%. The mean A1C at the start of the study was 12% ± 1.5%. In the 46 subjects for whom A1C was obtained at baseline and at 2 weeks, A1C had decreased by 0.4% at the 2-week visit to 11.6% ± 1.6% (p = 0.05 for Wilcoxon's signed range test ).
From Evidence to Recommendation
The GEG concluded that the use of HbA1c does not support the diagnosis of glycemic crises, although it is useful for monitoring the patient after it has already been stabilized. Furthermore, the undesirable effects of the intervention were trivial, the certainty of the evidence very low, we did not find any cost-effectiveness studies for the intervention. Therefore, it was concluded that the strength and direction of the recommendation are "Conditional Against"
Question 2: In adult diabetic patients with glucose disorders, what is the use of requesting ketone bodies for the management of acute glucose disorders?
Evidence Summary
In the systematic search, two systematic reviews were found(29,30). Brooke's systematic review was excluded because it used capillary blood in its evaluation and the GEG considered that studies, where the sampling was not capillary, should be included. The study by Klocker et al. included 4 studies(31-34)which were reviewed in full text. It was shown that the hydroxybutyrate blood test compared to the hydroxybutyrate urine test is associated with a reduced frequency of hospitalization and shorter recovery time from diabetic ketoacidosis. The blood ketone test is also associated with lower costs and greater patient/caregiver satisfaction.
From Evidence to Recommendation
The GEG considered the use of B-hydroxybutyrate in blood in diabetic patients important because the evidence supports the benefits of b-hydroxybutyrate tests over urine acetoacetate tests to reduce the frequency of hospitalization and reduce the costs of care to detect the resolution of ketosis in a more timely manner, that the resources are available to perform the test, that the intervention is accepted by the GEG and that its implementation at the institutional level is feasible. It was concluded as a “Strong in favor” recommendation. In addition, a table was prepared that contains criteria to establish the diagnosis and severity of diabetic ketoacidosis and hyperosmolar hyperglycemic state in which ketone bodies are included (seetable 4).
Table 4. Recommendations made by the GEG in cases of hypoglycemia with strength and direction of the recommendation.
| Indicator Type | Indicator | Indicator Formula | Expected value (At 6 months) | Biannual goal |
|---|---|---|---|---|
| Process | Percentage of diabetic patients with hyperglycemic seizures with B-hydroxybutyrate blood test evaluation | Diabetic patients with hyperglycemic crises seen in emergencies with B-hydroxy-butyrate blood test results / Total Diabetic patients with hyperglycemic crises seen in emergencies | > 60% | 100% |
| Process | Percentage of diabetic patients with a glycemic crisis who have been stabilized in a maximum time of 24 hours | Diabetic patients with glycemic crisis who have been stabilized in a maximum time of 24 hours / Total diabetic patients who have been admitted for glycemic crisis | > 60% | > 80% |
| Process | Percentage of hypoglycemic events in diabetic patients ad-mitted for hyperglycemic crisis | Number of hypoglycemic events that have occurred during the management of hyperglycemic seizures / Total measurements performed in diabetic patients who have been admitted for hyperglycemic seizures | < 5% | < 2% |
| Process | Percentage of diabetic patients admitted to the emergency room due to hypoglycemic cri-sis and have received the educational program | Diabetic patient admitted to the emergen-cy room due to a glycemic crisis and received the educational program / Total number of patients admitted to the emergency room due to a glycemic crisis | > 60% | > 80% |
| Result | Percentage of diabetic patients who are readmitted due to hypoglycemia after having received the educational program | Diabetic patients with hypoglycemia who received the educational program and have been readmitted to the emergency department in the last 3 months / Total diabetic patients with hypoglycemic crisis treated in the emergency room | < 20 % | < 10% |
Source: Self made.
Question 3: In an adult patient with diabetes with a diagnosis of Hyperosmolar Hyperglycemic State / Diabetic Ketoacidosis (EHH / CAD), what is the most useful dose of insulin to manage hyperglycemia?
Evidence Summary
A systematic search was carried out that concluded in the review of 2 articles for full text (no systematic reviews were found)35,36. The study by Andrade-Castellanos et al was excluded because in the full-text review the GEG showed that it did not answer the PICO question posed. The Firestone et al study evaluated a total of 4393 blood glucose readings. For the primary efficacy outcome, hospital stay was reduced from 149.9 ± 134.4 to 114.4 ± 103.1hr (p = 0.039). There was a decrease in the median hospital stay of 102.2 hours (interquartile range (IQR), 68.8-171.4 hours) in the group that received highly intensive insulin therapy at 92.4 hours (IQR, 60.4-131.4hr ) in the group that received moderately intensive insulin therapy (p <0.001). The relative risk (RR) of staying in hospital on day 7 (0.51; 95% CI, 0.29-0.91; p = 0.022) and day 14 (0.28; 95% CI, 0.080-0.97; p = 0.044) were significantly reduced by the moderate-intensity insulin therapy strategy.
From Evidence to Recommendation
The GEG considered, based on the balance of the effects in favor of moderate-intensity insulin therapy, the availability and ease of its implementation, and that all the participants of the GEG accepted the intervention, to start the insulin infusion dose low (0.05 - 0.1 U / Kg / h). In addition, gradually adjust the insulin dose until the patient with a hyperglycemic crisis comes out of critical condition and stabilizes their glucose levels. It was concluded in the strength and direction of “Strong in favor”.
Question 4: In adult patients with diabetes with a diagnosis of HHD / CAD with a K value <= 3.3, what is the most useful dose of potassium replacement to treat hypokalemia?
Evidence Summary
The systematic search concluded in the review of 10 articles for full text (no systematic reviews were found). All articles were excluded for not answering the PICO question posed. The Canadian Clinical Practice Guidelines18were used and the study by Kitabchi37and the study by Chiasson38. was reviewed. In these manuscripts, doses between 10-40 mmol / L of potassium administration are established to control hypokalemia and points to take into account potassium levels in the blood. After analyzing the CPG studies, the GEG decided to adopt a recommendation and also establish 02 points of good practice.
From Evidence to Recommendation
The GEG concluded in a recommendation “strong in favor” of administering potassium at a dose of 10 - 20 mmol / L if serum potassium <3.3 mmol / L because the intervention was accepted by the entire GEG, it is feasible to implement and that no extra resources are required for its implementation. Also, as points of good clinical practice: avoid potassium administration if K is> 5.2 mEq / l and stop insulin administration (seetable 5)
Question 5: In an adult patient with diabetes with a diagnosis of HHD / CAD, what is the most useful dose of electrolyte solution (fluid therapy) to treat the disorder?
Evidence Summary
The systematic search concluded in the review of 04 articles for full text (no systematic reviews were found). All articles were excluded for not answering the PICO question posed. The evidence was obtained from the Canadian Clinical Practice Guidelines18and the American Diabetes Association's Clinical Practice Guidelines19and the studies by Adrogué39and Fein40were extracted. The first study concludes that a moderate and cautious administration of fluid therapy is necessary since it allows faster recovery, cost reduction, and reduction of harmful effects. In the second it is concluded that the administration of fluid therapy at large volumes seems to lead to a hypooncotic state that could cause both subclinical cerebral edema and pulmonary edema.
From Evidence to Recommendation
Taking into account the CPGs and the primary studies analyzed and that during the panel discussion it was evidenced that the balance was in favor of the administration of 0.9% NaCl at 1 L / h, that there was no considerable variation in both the required resources and the in the feasibility of its implementation and that the GEG was unanimously in favor of considering the intervention, it was concluded in a recommendation “strong in favor” regarding the administration of NaCl 0.9% at 1 L / h until correcting the hypovolemic shock and a point of good clinical practice.
Question 6: In adult patients with diabetes who are diagnosed with HHE / CAD with hypophosphatemia, what is the most useful dose of Phosphorus Replacement to treat the disorder?
Evidence Summary
A systematic search was carried out where 236 studies were identified which were removed after the title and abstract review for not answering the PICO question. The evidence was obtained from the Canadian Clinical Practice Guidelines18where Fisher's study was found41. In this study, the effect of phosphate as an intermediate for oxygenation of tissues was evaluated. Thirty patients were studied who were divided into two groups to determine the effect of phosphate on 2,3-DPG, dissociation of oxyhemoglobin, serum levels of phosphorus, calcium, lactate, pyruvate, and electrolytes, and the response in the values of glucose, bicarbonate, and pH. The study concluded that phosphate therapy could accelerate erythrocyte regeneration in a small number of the patients studied and that this could not demonstrate an influence on tissue oxygenation or an improvement in clinical response; in addition, an exaggerated increase in hypocalcemia was evidenced in patients treated with phosphorus, which leads to great caution when using phosphate as therapy.
From Evidence to Recommendation
The GEG considered evaluating the balance against what was reported by the study, taking into account the risk of the administration of the drug and unanimously with respect to the risks of the intervention concluded in adopting the recommendation and graduating it as "strong against". Two points of good clinical practice were raised (seetable 5).
Question 7: In adult patients with diabetes mellitus with a diagnosis of CAD, what is the most useful replacement dose of HCO + to treat the disorder?
Evidence Summary
The systematic search concluded in the review of 2 articles for full text (no systematic reviews were found). The two articles were excluded for not answering the PICO question posed. We worked with the Canadian Clinical Practice Guide from which Chua's systematic review42was extracted. The systematic review evaluated the efficacy and risks associated with the administration of bicarbonate in the emergency treatment of severe acidemic events in patients with diabetic ketoacidosis. They reviewed 508 potential studies of which they included 44 studies of which 3 were controlled clinical trials in the adult population. In addition, a marked heterogeneity in the pH, concentration, amount, and time of administration of bicarbonate was identified between studies. In 2 of the clinical trials reviewed, an improvement in metabolic acidosis was demonstrated with the initial treatment of bicarbonate in the first 02 hours. On the other hand, there was no evidence of improvement in glucose controls or clinical efficacy. An increase in the risk of cerebral edema and prolonged hospitalization time was not found in children who received bicarbonate, the need for potassium supplementation was increased in these patients. No differentiation of type 1 diabetics or type 2 diabetics with diabetic ketoacidosis was reported, which caused the panel to lower the certainty of the evidence; however, it was decided that it should not be administered.
From Evidence to Recommendation
The GEG analyzed the balance of the intervention and taking into account the risks unanimously concluded in a recommendation “Strong against” for cases where the pH <6.9 (because the population included in the studies of the systematic review had these characteristics). In addition, a point of good clinical practice was established (seetable 5).
Hypoglycemia
3 questions were raised regarding hypoglycemia. A table was prepared that summarizes the diagnosis and severity of hypoglycemia (see Table 6). Further; a figure was prepared that included a summary of the diagnosis and management of hypoglycemia (seefigure 1).
Question 8: En pacientes adultos diabéticos que presentan hipoglicemia severa ¿Cuál es la dosis más útil de glucosa (dextrosa) para tratar la hipoglucemia severa?
Evidence Summary
A systematic search was carried out which concluded in the review of 3 articles for full text (no systematic reviews were found). All articles were excluded for not answering the PICO question posed. We worked with the evidence from the Canadian Clinical Practice Guidelines18whereby consensus on the adopted recommendation was raised. Regarding the definition of severe hypoglycemia, it was decided that it would obey clinical criteria or laboratory values as specified intable 6.
From Evidence to Recommendation
Although no primary studies or systematic reviews were found to answer the question, taking into account the information found in the CPG during the discussion, the GEG considered the intravenous treatment of severe hypoglycemia in an unconscious person with intravenous administration of 25 g (4 ampoules of 33% dextrose). Regarding the route of administration, some experts considered the term "severe" to be when there is a loss of consciousness, despite not having found evidence to support it necessarily and that some patients may find themselves with severe hypoglycemia (Glucose <2.8 mg/dl) without being unconscious. If conscious, the GEG considered it necessary to specify that glucose administration is oral. Three points of good practice were formulated.
Question 9: In adult diabetic patients with hypoglycemia, what is the time that they must remain under observation before being discharged?
Evidence Summary
A systematic search was carried out which concluded in the review of 3 articles for full text (no systematic reviews were found). All articles were excluded for not answering the PICO question posed. The Canadian Clinical Practice Guide18was used and the study by Tan H. K.43. was reviewed. In the latter, 9550 patients were analyzed in the 6 months: 138 patients with diabetes (9.5%) and 70 patients (2.7%) without diabetes, who had had an episode of hypoglycemia and had been cared for in the unit. medical evaluation. Patients with diabetes and hypoglycemia at admission had a significantly longer stay (mean SD) (10.3 11.2 vs. 7.3 9.5 days, P = 0.001) and a higher in-hospital mortality rate (14.5 vs. 5.2%, P <0.001) in comparison with those without hypoglycemia Patients without diabetes with hypoglycemia had a longer stay (mean SD) (9.1 10.5 vs. 6.7 9.9 days, P = 0.05) and a higher hospital mortality rate (24.3 vs. 5.4%, P <0.001) compared to those without hypoglycemia. In conclusion, hypoglycemia is associated with a longer duration of hospitalization and an increase in the hospital mortality rate. Hypoglycemia may have contributed to the worse outcome, but it also appears to be a marker of the severity of the disease in poorly controlled patients, especially patients with sepsis.
From Evidence to Recommendation
After the analysis, the GEG concluded that because no direct evidence was found to support issuing a recommendation in this regard and that both the aforementioned study and the Canadian CPG show the need for better surveillance in hypoglycemic patients admitted by emergency that It is necessary to consider three points of good practice that were included in the CPG.
Question 10: In adult diabetic patients with hypoglycemia, what is the usefulness of individualized educational therapy to prevent readmission for hypoglycemia at discharge?
Evidence Summary
A systematic search was carried out which concluded in the review of 5 articles for full text (no systematic reviews were found). 04 studies44-47were excluded for not answering the PICO question. The study by Cox D.48was included, which evaluated 60 adults with DM1 and a history of ≥ 2 episodes of severe hypoglycemia (inability to treat oneself due to hypoglycemic stupor or unconsciousness) for 6 consecutive months. It was concluded that patients with hypoglycemia anticipation, awareness, and treatment training (HAATT) were able to reduce the occurrence of hypoglycemia, as reflected in three different parameters: low glycemic index, lower mean glycemic reading, and glycemic percentage < 3.9 mmol / L. Because the population was small and only patients with type 1 diabetes mellitus were included, a very low certainty of the evidence was established.
From Evidence to Recommendation
Based on the evidence and the discussion of the GEG that included the balance in favor of the intervention, the unanimity in including the intervention, its low cost and feasibility in the implementation (both since it would not involve an extra cost to standardize the program such as training a group of nursing or psychology professionals to provide therapy), it was concluded to recommend the standardization of the educational program as a “strong in favor” recommendation and add a point of good clinical practice
Table 5. Criteria for the diagnosis and severity of diabetic ketoacidosis and hyperosmolar hyperglycemic state in diabetic patients.
| Criterios Diagnósticos | Cetoacidosis Diabética | Estado Hiperosmolar | ||
| Mild (Plasma Glucose >=250 mg/dl) | Moderate (Plasma Glucose >=250 mg/dl) | Severe (Plasma Glucose >=250 mg/dl) | (Plasma Glucose >=600 mg/dl) | |
| Arterial Ph | 7.25-7.30 | 7.00 a <7.25 | <7.00 | >7.30 |
| Anion Gap | >10 | >12 | >12 | Variable |
| Blood Osmolarity | Variable | Variable | Variable | >320 mOsm/Kg |
| Bicarbonate of Blood | 15-18 mEq /L | 10-<15 mEq /L | <10 mEq /L | >18 mEq /L |
| Ketonic Bodies in Blood / Urine | Positive | Positive | Positive | Slightly positive |
| Neurological Status | Alert | Alert/Sleep | Stupor / Coma | Stupor / Coma |
Source: Prepared based on the translated criteria of Kitabchi AE, Umpierrez GE. Hyperglycemic crises in adult patients with diabetes. ADA. 2009; 32 (7): 1336.
Table 6. Criteria for the administration of electrolytes (potassium, phosphorus and bicarbonate) in diabetic ketoacidosis and hyperosmolar hyperglycemic state.
| Diagnostic criteria | Standard to start administration | ||
|---|---|---|---|
| Diabetic cetoacidosis | Hyperosmolar hyperglycemic state | ||
| Match | Consider phosphate replace-ment if serum phosphate <1 mg / dL (0.32 mmol / L) (also consider phosphate replacement in patients with cardiac dysfunction, anemia, or respiratory distress) | Limit phosphorus replacement to persistent hypophosphatemia (after the acute phase has elapsed). | |
| Potassium | If K ≥ 5.2 mEq / L (5.2 mmol / L), no replacement but continuous monitoring every 2 hours. | Potassium is usually elevated, generally due to extracellular change caused by insulin deficiency, hypertonicity, and acidemia. | |
| If K ≥ 3.3 mEq / L and K <5.2 mEq / L (5.2 mmol / L); replenish potassium as recommended | |||
| If K <3.3 mEq / L (3.3 mmol / L) re-places potassium earlier as recommended before starting insulin therapy. | |||
| Baking soda | Replenish usually if the pH is less than 6.9. (Consider replacement in special conditions such as vascular collapse or cardiac arrhythmias) | It does not require | |
Source: Elaborated based on the translated criteria Kitabchi AE, Umpierrez GE. Hyperglycemic crises in adult patients with diabetes. ADA. 2009; 32 (7): 1336.
Table 7. Criteria for the diagnosis and severity of hypoglycemia in diabetic patients.
| Mild (level 1) | Moderate (level 2) | Severe (level 3) |
|---|---|---|
| Autonomic signs: tremor, palpitations, sweating, anxiety, nausea pre-sent and / or | Autonomic and neuroglycopenic symptoms (Difficulty concentrating,Confusion, weakness, drowsiness, vision changes, headache, dizziness) present and / or | It could be unconscious.Severe event characterized by men-tal and physical alterations and / or |
| Glucose minus 70 mg / dL and ≧ 54 mg / dL. (3.9 mmol / L) | Glucose <54 mg / dL. (3 mmol / L) | Glucose usually less than 50 mg / dL. (2.8 mmol) |
Source: Elaborado en base a los criterios traducidos de CJD “Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada y los criterios traducidos de ADA. “American Diabetes Association Standards of Medical Care in Diabetes”—2019”.
REFERENCES
1. Muka T, Imo D, Jaspers L, Colpani V, Chaker L, van der Lee SJ, et al. The global impact of non-communicable diseases on healthcare spending and national income: a systematic review. Eur J Epidemiol. 2015;30(4):251-277. DOI: 10.1007/s10654-014-9984-2 [ Links ]
2. Seuring T, Archangelidi O, Suhrcke M. The Economic Costs of Type 2 Diabetes: A Global Systematic Review. Pharmacoeconomics. 2015;33(8):811-831. DOI: 10.1007/s40273-015-0268-9. [ Links ]
3. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. DOI: 10.1016/j.diabres.2019.107843. [ Links ]
4. McNaughton CD, Self WH, Slovis C. Diabetes in the Emergency Department: Acute Care of Diabetes Patients. Clin Diabetes. 2011;29(2):51-59. Disponible en: https://doi.org/10.2337/diaclin.29.2.51. [ Links ]
5. Villena JE. Diabetes Mellitus in Peru. Annals of Global Health. 2015;81(6):765-775. Disponible en: https://doi.org/10.1016/j.aogh.2015.12.018. [ Links ]
6. Jawaid A, Sohaila A, Mohammad N, Rabbani U. Frequency, clinical characteristics, biochemical findings and outcomes of DKA at the onset of type-1 DM in young children and adolescents living in a developing country - an experience from a pediatric emergency department. J Pediatr Endocrinol Metab. 2019;32(2):115-119. DOI: 10.1515/jpem-2018-0324. [ Links ]
7. Iloh GUP, Amadi ANk. Epidemiology of Diabetic Emergencies in the Adult Emergency Department of a Tertiary Hospital in South-Eastern Nigeria. Int J Trop Dis Health. 2018;1-10. Disponible en: https://doi.org/10.9734/IJTDH/2018/28806. [ Links ]
8. MINSA. Guía Técnica: "Guía de Práctica Clínica para el diagnóstico, tratamiento y control de la diabetes mellitus tipo 2 en el primer nivel de atención". 2015. Disponible en: https://cdn.www.gob.pe/uploads/document/file/194552/193275_RM_719-2015 MINSA.pdf20180904-20266-1tlkwzr.pdf. [ Links ]
9. Neira-Sanchez ER, Málaga G. ¿Son las guías de práctica clínica de hipertensión arterial y diabetes mellitus tipo 2 elaboradas por el MINSA, confiables? Rev Peru Med Exp Salud Pública. 2016; 33(2):377. Disponible en: https://rpmesp.ins.gob.pe/index.php/rpmesp/article/view/2093/2254. [ Links ]
10. Schünemann HJ, Wiercioch W, Brozek J, Etxeandia-Ikobaltzeta I, Mustafa RA, Manja V, et al. GRADE Evidence to Decision (EtD) frameworks for adoption, adaptation, and de novo development of trustworthy recommendations: GRADE-ADOLOPMENT. J Clin Epidemiol. 2017;81:101-110. DOI: https://doi.org/10.1016/j.jclinepi.2016.09.009. [ Links ]
11. Tugwell P, Knottnerus JA. Adolopment - a new term added to the Clinical Epidemiology Lexicon. J Clin Epidemiol. 2017;81:1-2. DOI: 10.1016/j.jclinepi.2017.01.002. [ Links ]
12. Ministerio de Salud. Norma Técnica de Salud para la elaboración y Uso de Guías de Práctica Clínica. 2015. Disponible en: http://bvs.minsa.gob.pe/local/MINSA/3300.pdf. [ Links ]
13. Wong CHL, Wu IXY, Adams J, Steel A, Wardle J, Wu JCY, et al. Development of Evidence-Based Chinese Medicine Clinical Service Recommendations for Cancer Palliative Care Using Delphi Approach Based on the Evidence to Decision Framework. Integr Cancer Ther. 2020;19:1-13. DOI: 10.1177/1534735420940418 [ Links ]
14. Kallenbach M, Conrad S, Hoffmann F, Matthias K, Gartlehner G, Langer G, et al. GRADE Evidence-to-Decision-Tabellen für die Übernahme, Anpassung und De-novo-Entwicklung von vertrauenswürdigen Empfehlungen: GRADE-ADOLOPMENT. Z Für Evidenz Fortbild Qual Im Gesundheitswesen. 2019;144(145):90-99. Disponible en: https://doi.org/10.1016/j.zefq.2019.06.001 [ Links ]
15. Darzi A, Harfouche M, Arayssi T, Alemadi S, Alnaqbi KA, Badsha H, et al. Adaptation of the 2015 American College of Rheumatology treatment guideline for rheumatoid arthritis for the Eastern Mediterranean Region: an exemplar of the GRADE Adolopment. Health Qual Life Outcomes. 2017;15(1):183. Disponible en: https://hqlo.biomedcentral.com/articles/10.1186/s12955-017-0754-1. [ Links ]
16. Timana-Ruiz R. Desarrollo de Guías de Práctica Clínica en el Seguro Social del Perú. Rev Cuerpo Méd HNAAA. 2019;12(2):95-96. Disponible en: https://doi.org/10.35434/rcmhnaaa.2019.122.503. [ Links ]
17. Cabrera PA, Pardo R. Review of evidence based clinical practice guidelines developed in Latin America and Caribbean during the last decade: an analysis of the methods for grading quality of evidence and topic prioritization. Glob Health (Internet). 19 de febrero de 2019 (citado 26 de agosto de 2020);15. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6380043. [ Links ]
18. Diabetes Canada Clinical Practice Guidelines Expert Committee. Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. 2018;42(1):320-325. Disponible en: http://guidelines.diabetes.ca/cpg. [ Links ]
19. American Diabetes Association. American Diabetes Association's Standards of Medical Care in Diabetes-2019. Clin Diabetes. 2019;37(1):11-34. Disponible en: https://doi.org/10.2337/cd18-0105. [ Links ]
20. NICE. Type 1 diabetes in adults: diagnosis and management. 2015. Disponible en: https://www.nice.org.uk/guidance/ng17. [ Links ]
21. CENETEC. Dagnóstico y Tratamiento de la cetoacidosis diabética en niños y adultos. 2016. Disponible en: http://www.cenetec-difusion.com/CMGPC/SS-227-09/ER1.pd. [ Links ]
22. CENETEC. Diagnóstico y tratamiento del estado hiperglucémico hiperosmolar en adultos con diabetes mellitus tipo 2. 2016. Disponible en: http://www.cenetec-difusion.com/CMGPC/SS-227-09/ER1.pdf [ Links ]
23. Liang K, Sun Y, Li W, Zhang X, Li C, Yang W, et al. Diagnostic efficiency of hemoglobin A1c for newly diagnosed diabetes and prediabetes in community-based Chinese adults aged 40 years or older. Diabetes Technol Ther. diciembre de 2014;16(12):853-857. DOI: 10.1089/dia.2014.0157 [ Links ]
24. Yang C, Liu Y, Li X, Liang H, Jiang X. Utility of hemoglobin A1c for the identification of individuals with diabetes and prediabetes in a Chinese high risk population. Scand J Clin Lab Invest. 2012;72(5):403-409. DOI: 10.3109/00365513.2012.689324 [ Links ]
25. Guo W, Zhou Q, Jia Y, Xu J. Increased Levels of Glycated Hemoglobin A1c and Iron Deficiency Anemia: A Review. Med Sci Monit Int Med J Exp Clin Res. 2019;25:8371-8. DOI: 10.12659/MSM.916719. [ Links ]
26. Greci LS, Kailasam M, Malkani S, Katz DL, Hulinsky I, Ahmadi R, et al. Utility of HbA1c Levels for Diabetes Case Finding in Hospitalized Patients With Hyperglycemia. Diabetes Care. 2003;26(4):1064-1068. DOI: 10.2337/diacare.26.4.1064 [ Links ]
27. Su Y-W, Hsu C-Y, Guo Y-W, Chen H-S. Usefulness of the plasma glucose concentration-to-HbA1c ratio in predicting clinical outcomes during acute illness with extreme hyperglycaemia. Diabetes Metab. 2017;43(1):40-47. DOI: 10.1016/j.diabet.2016.07.036 [ Links ]
28. Magee MF, Nassar C. Hemoglobin A1c Testing in an Emergency Department. J Diabetes Sci Technol. 2011;5(6):1437-1443. DOI: 10.1177/193229681100500615. [ Links ]
29. Brooke J, Stiell M, Ojo O. Evaluation of the Accuracy of Capillary Hydroxybutyrate Measurement Compared with Other Measurements in the Diagnosis of Diabetic Ketoacidosis: A Systematic Review. Int J Environ Res Public Health. 2016;13(9):837. DOI: 10.3390/ijerph13090837. [ Links ]
30. Klocker AA, Phelan H, Twigg SM, Craig ME. Blood ß-hydroxybutyrate vs. urine acetoacetate testing for the prevention and management of ketoacidosis in Type 1 diabetes: a systematic review. Diabet Med. 2013;30(7):818-824. DOI: 10.1111/dme.12136. [ Links ]
31. Prisco F, Picardi A, Iafusco D, Lorini R, Minicucci L, Martinucci ME, et al. Blood ketone bodies in patients with recent-onset type 1 diabetes (a multicenter study). Pediatr Diabetes. 2006;7(4):223-228. DOI: 10.1111/j.1399-5448.2006.00187.x. [ Links ]
32. Laffel LMB, Wentzell K, Loughlin C, Tovar A, Moltz K, Brink S. Sick day management using blood 3-hydroxybutyrate (3-OHB) compared with urine ketone monitoring reduces hospital visits in young people with T1DM: a randomized clinical trial. Diabet Med. 2006;23(3):278-284. DOI: 10.1111/j.1464-5491.2005.01771.x. [ Links ]
33. Vanelli M, Chiari G, Capuano C, Iovane B, Bernardini A, Giacalone T. The direct measurement of 3-beta-hydroxy butyrate enhances the management of diabetic ketoacidosis in children and reduces time and costs of treatment. Diabetes Nutr Metab. 2003;16(5-6):312-316. Disponible en: https://pubmed.ncbi.nlm.nih.gov/15000443/ [ Links ]
34. Noyes KJ, Crofton P, Bath LE, Holmes A, Stark L, Oxley CD, et al. Hydroxybutyrate near-patient testing to evaluate a new end-point for intravenous insulin therapy in the treatment of diabetic ketoacidosis in children. Pediatr Diabetes. 2007;8(3):150-156. DOI: 10.1111/j.1399-5448.2007.00240.x. [ Links ]
35. Andrade-Castellanos CA, Colunga-Lozano LE, Delgado-Figueroa N, Gonzalez-Padilla DA. Subcutaneous rapid-acting insulin analogues for diabetic ketoacidosis. Cochrane Metabolic and Endocrine Disorders Group, editor. Cochrane Database Syst Rev (Internet). 21 de enero de 2016 (citado 20 de febrero de 2020); Disponible en: http://doi.wiley.com/10.1002/14651858.CD011281.pub2 [ Links ]
36. Firestone RL, Parker PL, Pandya KA, Wilson MD, Duby JJ. Moderate-Intensity Insulin Therapy Is Associated With Reduced Length of Stay in Critically Ill Patients With Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State: Crit Care Med. 2019;47(5):700-705. DOI: 10.1097/CCM.0000000000003709 [ Links ]
37. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic Crises in Adult Patients With Diabetes. Diabetes Care. 2009;32(7):1335-1343. Disponible en: https://doi.org/10.2337/dc09-9032. [ Links ]
38. Chiasson J-L, Aris-Jilwan N, Bélanger R, Bertrand S, Beauregard H, Ekoé J-M, et al. Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state. CMAJ Can Med Assoc J J Assoc Medicale Can. 2003;168(7):859-866. Disponible en: https://europepmc.org/article/med/12668546. [ Links ]
39. Adrogué HJ. Salutary Effects of Modest Fluid Replacement in the Treatment of Adults With Diabetic Ketoacidosis: Use in Patients Without Extreme Volume Deficit. JAMA. 1989;262(15):2108. DOI: 10.1001/jama.1989.03430150076029. [ Links ]
40. Fein IA. Relation of Colloid Osmotic Pressure to Arterial Hypoxemia and Cerebral Edema During Crystalloid Volume Loading of Patients with Diabetic Ketoacidosis. Ann Intern Med. 1982;96(5):570. DOI: 10.7326/0003-4819-96-5-570. [ Links ]
41. Fisher JN, Kitabchi AE. A Randomized Study of Phosphate Therapy in the Treatment of Diabetic Ketoacidosis*. J Clin Endocrinol Metab. 1983;57(1):177-80. DOI: 10.1210/jcem-57-1-177. [ Links ]
42. Chua H, Schneider A, Bellomo R. Bicarbonate in diabetic ketoacidosis - a systematic review. Ann Intensive Care. 2011;1(1):23. DOI: 10.1186/2110-5820-1-23. [ Links ]
43. Tan HK, Flanagan D. The impact of hypoglycaemia on patients admitted to hospital with medical emergencies. Diabet Med. 2013;30(5):574-580. DOI: 10.1111/dme.12123. [ Links ]
44. Naylor M. Comprehensive Discharge Planning for the Hospitalized Elderly: A Randomized Clinical Trial. Ann Intern Med. 1994;120(12):999. Disponible: https://www.diagnostic.grifols.com/en/clinical-diagnostics?gclid=CjwKCAiA_eb-BRB2EiwAGBnXXgAc3MBX4jP Ktm4_SUbMncfo6JEzVAoKK6by9weJIaNpTkOuVwmKhoCJ_gQAvD_BwE. [ Links ]
45. Dai Y-T, Chang Y, Hsieh C-Y, Tai T-Y. Effectiveness of a pilot project of discharge planning in Taiwan. Res Nurs Health. 2003;26(1):53-63. DOI: 10.1002/nur.10067. [ Links ]
46. Jayakody A, Bryant J, Carey M, Hobden B, Dodd N, Sanson-Fisher R. Effectiveness of interventions utilising telephone follow up in reducing hospital readmission within 30 days for individuals with chronic disease: a systematic review. BMC Health Serv Res (Internet). 18 de agosto de 2016 (citado 20 de febrero de 2020). Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4990979/ [ Links ]
47. Thompson CJ, Cummings F, Jung RT, Newton RW. The effects of an integrated education programme on the management of diabetic ketoacidosis. Pract Diabetes Int. 1995;12(5):235-237. Disponible en: https://doi.org/10.1002/pdi.1960120518. [ Links ]
48. Cox DJ, Kovatchev B, Kovatchev B, Koev D, Koeva L, Dachev S, et al. Hypoglycemia anticipation, awareness and treatment training (HAATT) reduces occurrence of severe hypoglycemia among adults with type 1 diabetes mellitus. Int J Behav Med. 2004;11(4):212-218. DOI: 10.1207/s15327558ijbm1104_4. [ Links ]
Received: December 01, 2020; Accepted: January 06, 2021











 text in
text in