Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista de la Facultad de Medicina Humana
Print version ISSN 1814-5469On-line version ISSN 2308-0531
Rev. Fac. Med. Hum. vol.21 no.1 Lima Jan-Mar 2021
http://dx.doi.org/10.25176/rfmh.v21i1.3239
Clinical case
Cystic neutrophilic granulomatous mastitis associated with corynebacterium: Case report
1Hospital General María Auxiliadora, Lima-Perú.
2Hospital Edgardo Rebagliati Martins, Lima-Perú.
Cystic neutrophilic granulomatous mastitis (CNGM) is a recently characterized entity, with specific histopathological details that differentiate it from other types of chronic idiopathic mastitis. The presence of gram-positive bacilli within cystic-like spaces surrounded by neutrophils, in a context of suppurative granulomatous inflammation, define this entity. The importance of its recognition in the diagnostic report lies in its association with infection by corynebacterial species, so that treatment with antibiotics can be targeted, beyond the anti-inflammatory treatment that is usually administered to idiopathic mastitis.
We describe the case of a 35-year-old female patient with no related history, with intermittent breast pain, associated with the presence of multiple hard, palpable nodules in both breasts, with results from multiple previous private biopsies that described chronic granulomatous mastitis with a tubercular reaction, for which she received treatment for tuberculosis. Despite this, the clinical response was partial. Histological slides were reviewed at the institution and the diagnosis of CNGM was then established.
The presentation of this case was considered important due to its low recognition among pathologists, despite presenting characteristics already defined by previous studies.
Key words: neutrophilic granulomatous mastitis; Gram-positive bacilli, corynebacteria, chronic mastitis (Source: MeSH NLM)
INTRODUCTION
Inflammatory mastitis is more frequently found in women of childbearing age, who are breastfeeding, that report clinical symptoms of pain, erythema, and swelling1. These conditions are often treated with antimicrobial agents and may require surgical intervention in settings complicated by abscess formation1.
Mastitis is usually classified by duration and inflammatory infiltrate, and includes acute-neutrophilic, subacute-granulomatous and chronic-lymphocytic / plasma mastitis1. The potential causes of this spectrum of diseases are variable and can include both infectious and non-infectious (autoimmune) and idiopathic inflammatory mechanisms1.
We present a case of cystic neutrophilic granulomatous mastitis (CNGM) and its literature review.
LITERATURE REVIEW
Granulomatous lobular mastitis is a rare subtype of mastitis1. This entity can be present as painful palpable breast masses that range from 1 to 10 cm in size1. Despite extensive clinical, imaging, pathological, and microbiological studies, a subgroup of patients with this entity remains undetermined of a specific etiology1. Such patients are sometimes labeled as "idiopathic granulomatous lobular mastitis” (1.
A clinicopathologic review carried out in Auckland-New Zealand, in 2003 by Taylor and collaborators, reported the existence of a strong correlation between Corynebacterium infection and granulomatous lobular mastitis in a cohort of 34 women3.
In 2011, at Baptist Hospital in Miami, Renshaw described specific histopathological features in three patients, including the presence of gram-positive bacilli inside cystic spaces surrounded by neutrophils in a context of suppurative granulomatous inflammation3. In the same way, Renshaw and collaborators gave this condition its name, coining the term cystic neutrophilic granulomatous mastitis (CNGM). (4
In 2017, in Australia, Johnstone and collaborators also studied idiopathic granulomatous mastitis, describing it as a rare inflammatory disease that mostly affects women of reproductive age, and finding that there is growing evidence of an association with infection by corynebacteria, especially in the context of a characteristic histologic pattern, called Cystic Neutrophilic Granulomatous Mastitis5. These authors evaluated 15 patients with a CMGN histologic pattern, subsequently finding corynebacteria by culture or 16S rRNA gene sequencing in samples obtained in surgery or fine-needle aspiration5.
Cystic neutrophilic granulomatous mastitis was also described in 2019 by Gautham et al, retrospectively studying the clinical and imaging characteristics of 6 female patients, whose ages ranged from 31 to 38 years1. In this study, a previous history of breast trauma, previous abscesses and fibrocystic disease were found in some of the patients as important antecedents1. All the patients studied showed histopathological findings compatible with CMGN, including inflammatory cells, and histiocytes, with the presence of granulomas, but mainly cystic spaces surrounded by a predominantly neutrophilic inflammatory infiltrate, as well as evidence of diphtheroid bacteria (type of corynebacteria) and Gram positive bacilli by means such as culture and Gram staining, respectively1. The author proposes to be attentive to this new entity, taking into account certain clinical and histopathological criteria, which are summarized inTable 1 1.
Table 1. Clinical and histopathological criteria extracted and adapted from the study carried out by Gauthamet al
| Clinical criteria: |
| 1. Female patient, close to the 4th decade of life, with mammary tumor(s). |
| 2. Null or partial response with initial empirical antibiotic treatment (eg antituberculous treatment). |
| Histopathological criteria: |
| 3. Cystic-looking spaces surrounded by mixed inflammation, predominantly neutrophilic; with the presence of non-caseous granulomas. |
| 4. Verification of the presence of Gram-Positive bacilli or corynebacteria (with Gram stain or culture). |
Source:Gautham I, Radford DM, Kovacs CS, et al. Cystic neutrophilic granulomatous mastitis: The Cleveland Clinic experience with diagnosis and management. Breast J. 2019; 25:80-85
Among the differential diagnoses of this entity, we find other granulomatous processes such as tuberculosis, fungi, and atypical mycobacteria in immunosuppressed patients2.
Regarding treatment, the best antibiotics are those lipophilic, with bactericidal activity, among which are rifampicin, clarithromycin, trimethoprim-sulfamethoxazole and clindamycin6. Beta-lactams and quinolones are not useful, because they have low lipid solubility6. In Peru, there are reports of idiopathic granulomatous mastitis, however, there are no reports of cystic neutrophilic granulomatous mastitis. Therefore, it was decided to publish this clinical case.
PRESENTATION OF THE CASE
This report describes a 35-year-old female patient, that was evaluated in the hospital, with no relevant history, with an illness period of time of approximately 1 and a half years and who presented intermittent breast pain associated with the presence of multiple hard palpable nodulations in both breasts. She presented the result of multiple previous particular biopsies, which were described as chronic granulomatous mastitis with multinucleated giant cells and a tuberculous-type reaction, receiving the diagnosis of Mammary Tuberculosis. According to this, antituberculous treatment was started with a sensitive scheme, since August 2019, completing 54 doses of the first phase, and only 13 doses of the second phase, due to an adverse dermal reaction. Subsequently, she restarted the treatment with Isoniazid, after which she again presented a dermal reaction. Even though having received antituberculous treatment, the palpable tumors only partially relented. Because of this reason, revision of the histological plates is requested.
Mixed inflammation was observed, with presence of an inflammatory infiltrate mainly composed of neutrophils, surrounding spaces with a cystic appearance. Due to the suspicion of cystic neutrophilic granulomatous mastitis, and its frequent association with Gram positive bacilli, mainly corynebacteria, Gram staining was performed on the tissue, which showed the presence of Gram-positive bacilli in the empty spaces, surrounded by neutrophils (Figure 1, 2 y 3).
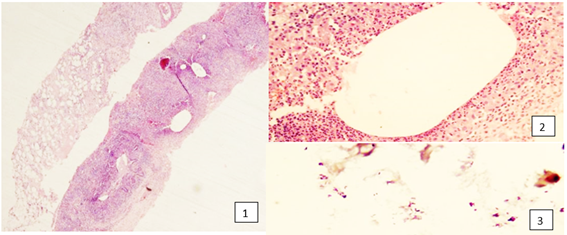
Figure 1. Trucut biopsy of breast tissue, showing cystic-like spaces (10x). Figure 2. Mixed inflammatory component, with a predominance of neutrophils, surrounding cystic-like spaces (40x). Figure 3. Gram bacilli + in cystic aspect space of anterior image (100x).
With these findings, the definitive diagnosis of cystic neutrophilic granulomatous mastitis was established. The patient was reassessed, the antituberculous scheme was suspended, completing her antibiotic treatment with Rifampicin and analgesics, and she was finally discharged due to clinical improvement.
DISCUSSION
Cystic neutrophilic granulomatous mastitis is a recently described entity, diagnosed with well-defined histopathological criteria (Table 1 1). In this case report, all of them were evidenced, which is why they supported the final diagnosis of cystic neutrophilic granulomatous mastitis. Likewise, it is known that it occurs more frequently in women between 30 and 40 years2, which coincides with the age of the patient in the present case, who is 35 years old.
The role of Corynebacterium, a Gram Positive (+) bacillus, in invasive infections is often discussed, since most of these species are part of the endogenous skin flora6. However, the link between Corynebacterium and granulomatous mastitis has been reported periodically since the publication of the case series by Taylor and collaborators in 2003 (3. For this reason, in this particular case, a Gram staining of the biopsied tissue was conducted, finding and proving this association interestingly.
The differential diagnosis from the histopathological point of view arises with other granulomatous processes such as mycobacterial infections, mainlyMycobacterium tuberculosisinfections byMycobacterium aviumcomplex in immunocompromised patients, and infection produced byHistoplasma capsulatumtype of fungus2. For its differential diagnosis, special stains such as Ziehl Neelsen are performed to rule out acid-fast bacilli, corresponding to tuberculosis; and PAS and Grocott stains to rule out fungi2, as well as additional diagnostic methods such as culture2. In this case, Ziehl Neelsen staining was also requested, which was negative.
According to treatment, it is relevant to mention that the corynebacteria survive in the cystic appearing spaces, surrounded by a reactive neutrophilic granulomatous infiltrate, instead of living in swollen tissue6. This inflammatory reaction can be rapid, it can appear in the first week from the onset of clinical symptoms6. In this setting, agents that are highly lipophilic and have a high volume of distribution can achieve adequate tissue concentrations for bactericidal activity, including rifampicin, clarithromycin, trimethoprim-sulfamethoxazole, and clindamycin6. In contrast, beta-lactams and fluoroquinolones have low lipid solubility and, therefore, they are expected to be less effective6. All of the aforementioned would explain the reason why rifampicin, an antituberculous drug, had an important effect on treatment, finally achieving clinical improvement in the patient deciding her medical discharge.
CONCLUSIONS
Cystic neutrophilic granulomatous mastitis is an entity previously described as part of the spectrum of idiopathic granulomatous mastitis. Recently defined and with well-established histopathological criteria, it presents an important association with infection by corynebacteria, which targets the treatment.
It is mandatory to motivate specialists in mammary pathology to take into account this differential diagnosis whenever we face a granulomatous mastitis with these histopathological characteristics. In addition, we recommend studying the presence of Gram-Positive bacilli in these patients, to establish an appropriate and duly supported diagnosis; so that targeted treatment can be provided.
REFERENCES
1. Gautham I, Radford DM, Kovacs CS, et al. Cystic neutrophilic granulomatous mastitis: The Cleveland Clinic experience with diagnosis and management. Breast J. 2019; 25:80-85. [ Links ]
2. Pérez P Juan Antonio, Bohle O John, Sánchez C Gonzalo, Carrasco L Cristian, Mariángel P Pablo. Mastitis granulomatosa idiopática: Diagnóstico y tratamiento en 14 casos. Rev Chil Cir. 2007 Ago; 59(4): 259-263. [ Links ]
3. Taylor GB, Paviour SD, Musaad S, Jones WO, Holland DJ. A clinicopathological review of 34 cases of inflammatory breast disease showing an association between corynebacteria infection and granulomatous mastitis. Pathology. 2003; 35:109-119. [ Links ]
4. Renshaw AA, Derhagopian RP, Gould EW. Cystic neutrophilic granulomatous mastitis: an underappreciated pattern strongly associated with gram-positive bacilli. Am J Clin Pathol. 2011; 136:424-427. [ Links ]
5. Johnstone KJ, Robson J, Cherian SG, Wan Sai Cheong, Kerr K, Bligh JF. Cystic neutrophilic granulomatous mastitis associated with Corynebacterium including Corynebacterium kroppenstedtii. Pathology. 2017 Jun;49(4):405-412. [ Links ]
6. Dobinson HC, Anderson TP, Chambers ST, Doogue MP, Seaward L, Werno AM. 2015. Antimicrobial treatment options for granulomatous mastitis caused by Corynebacterium species. J Clin Microbiol 53:2895-2899. [ Links ]
Received: September 02, 2020; Accepted: December 17, 2020











 text in
text in 


